We sat down with Dr. Charlene Flash, Assistant Medical Director of HIV Prevention Services for Harris Health System in Houston, TX, and Assistant Professor of Medicine in the Division of Infectious Disease at Baylor College of Medicine to talk about her history of working with PrEP and disparity in use between men and women.
Q: You are one of the nation’s leading experts in the implementation of PrEP. What motivated you to focus your efforts on PrEP?
A: I clearly remember going to an AIDS hospice and visiting with the patients early in my career. There was not a lot that I could do for these patients except to be with them and support them through a horrendous experience. This, layered with personal experiences of people in my community who died from the disease and the stigma that followed them, drove me to want to pursue a career in ending AIDS.
When I later learned about PrEP during my fellowship, before it was FDA approved, I was skeptical but curious to investigate what the community thought of this as a new prevention method. I wondered why we were only talking about men when women are also impacted by this epidemic, and why no one at the time was exploring how to address HIV in heavily impacted communities in the southern U.S.
While touring the walk-up HIV testing program at Houston’s Harris Health System, I met a primary tester named Nicole who helped inspire me to implement PrEP there. She was testing her patients and discussing their risk profile while also encouraging them to adjust their risk behavior. For those at high-risk, she could only offer future testing. It was then that I realized PrEP could help high-risk patients like these. I began researching how to reach patients in resource-limited settings. I investigated how you can make PrEP work in communities in need by looking at the structural, institutional, and personal barriers to preventing new HIV infections. I wanted to examine what it means to try to prevent someone from getting this disease.
Q: You developed one of the first comprehensive HIV prevention programs in the U.S. to prescribe PrEP to high-risk heterosexual individuals and men who have sex with men. What did you learn in the process and what still needs to be done?
Having these (PrEP) visuals through AIDSVu will help us to clearly see where disparities are happening, so we can apply our collective brainpower to figure out how to address them.
A: I learned that it is hard work because you can’t just stabilize a single variable and move forward. Working in PrEP is about dealing with people’s perceptions, institutional cultures, and the ways they are willing to diffuse this innovation in their institutions. It is also important to reflect on our national healthcare landscape and how to move our dialogue away from only thinking about health issues like cardiovascular disease, diabetes, and obesity, to also include sexual health in the discussion.
If someone does not have a clear perception of their risk, then they are not going to necessarily embrace the idea of using PrEP. Institutional barriers can also influence personal perceptions. We need to address the stigma around HIV transmission and clarify what motivates people’s actions as we help institutions and the people who work there really think about drivers of behavior.
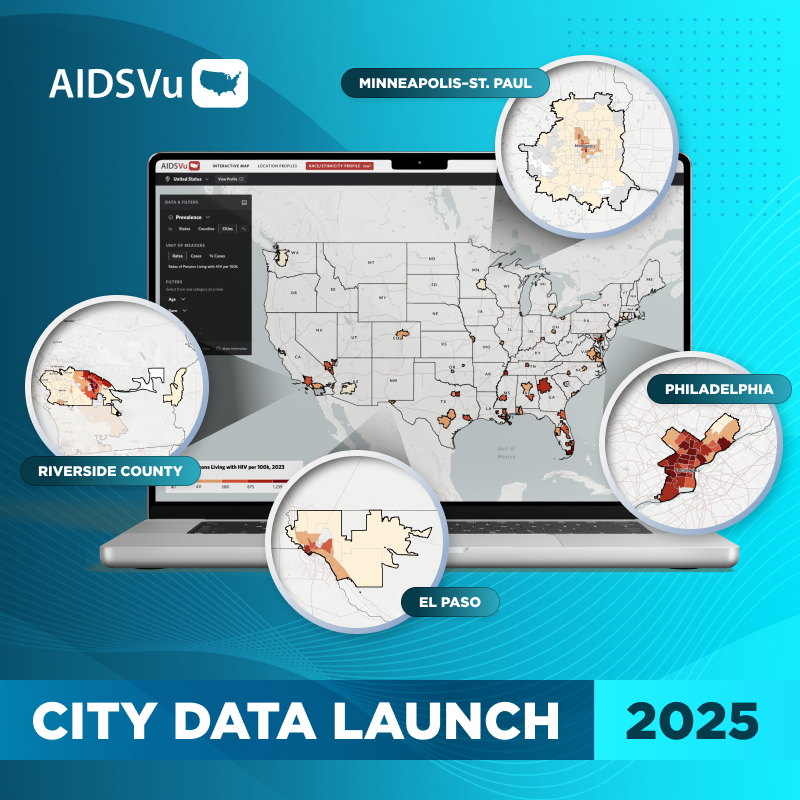
Q: AIDSVu recently launched the first-ever maps visualizing PrEP use at the state-level. How can individuals and academics use these maps to create awareness and expand use of PrEP?
A: These maps help tease out some of the things that people on the ground already know, mainly that some institutions embrace the concept of PrEP but there are also entire regions where the community is not engaged in a dialogue around HIV prevention. I think looking at the PrEP data maps and the new HIV diagnoses maps make the vast disparity in PrEP use painfully obvious.
Even to those who may not be very engaged in their community, these maps can stir conversation. People can point to all the new HIV diagnoses and ask why PrEP is not being prescribed in their communities. Personally, I utilize AIDSVu often because visualizing the epidemic makes it a local issue. Making the conversations personal often encourages people to take action.
Q: AIDSVu maps revealed that only 7 percent of PrEP users in 2016 were women but they accounted for 19 percent of new diagnoses that same year. What needs to be done to close this gap?
When PrEP was initially being prescribed, we found that 50 percent of prescriptions were written for women and 50 percent for men, but as the years moved forward, we saw a gender disparity start to emerge. Layered on that gender disparity was a racial disparity where more and more prescriptions were being written for white individuals and in white communities and not as many prescriptions were being written in Black and Hispanic/Latino communities.
One challenge is that the initial studies around PrEP were interpreted to show that PrEP might not work for women as well as it did for men. Later analysis soon revealed that it was not true. The disparity came from the fact that women who were being prescribed PrEP in the context of these clinical trials didn’t self-attribute risk and were not necessarily taking the medication as prescribed. Moving that news through the scientific community takes time.
Furthermore, the availability and FDA approval of PrEP was more well-funded and highly promoted to men. Historically, many of our champions in HIV advocacy work and political action have been in the community of men who have sex with men. As advocacy remains low among women, communities of color, and young people, the disparity in PrEP use has become more pronounced. Having these visuals through AIDSVu will help us to clearly see where disparities are happening, so we can apply our collective brainpower to figure out how to address them. If we want to equitably increase the appropriate use of PrEP in communities at risk, it means doing the hard work of reaching out to what people may label as historically hard to reach populations.