The Landscape of HIV Among Women in the United States
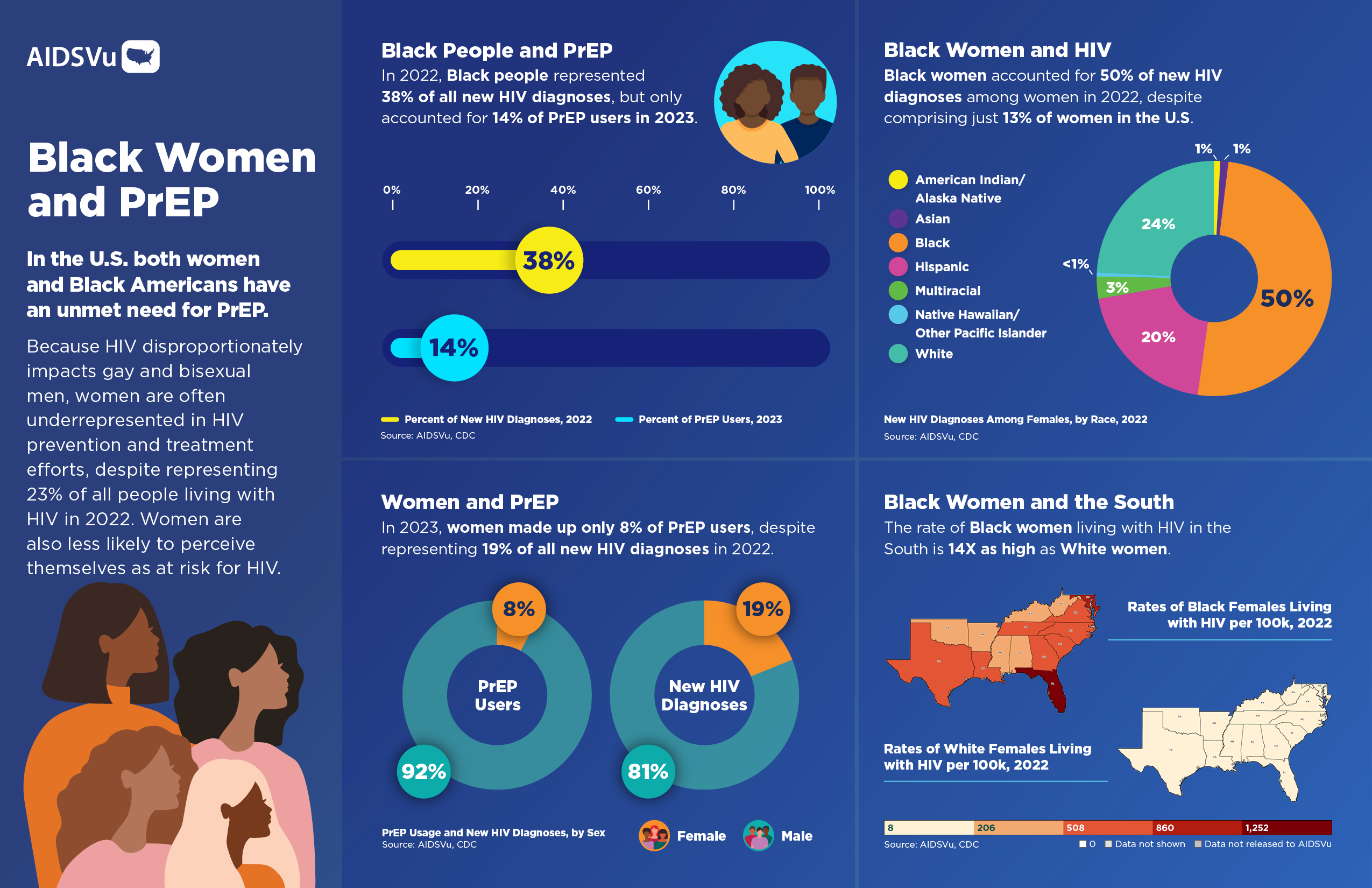
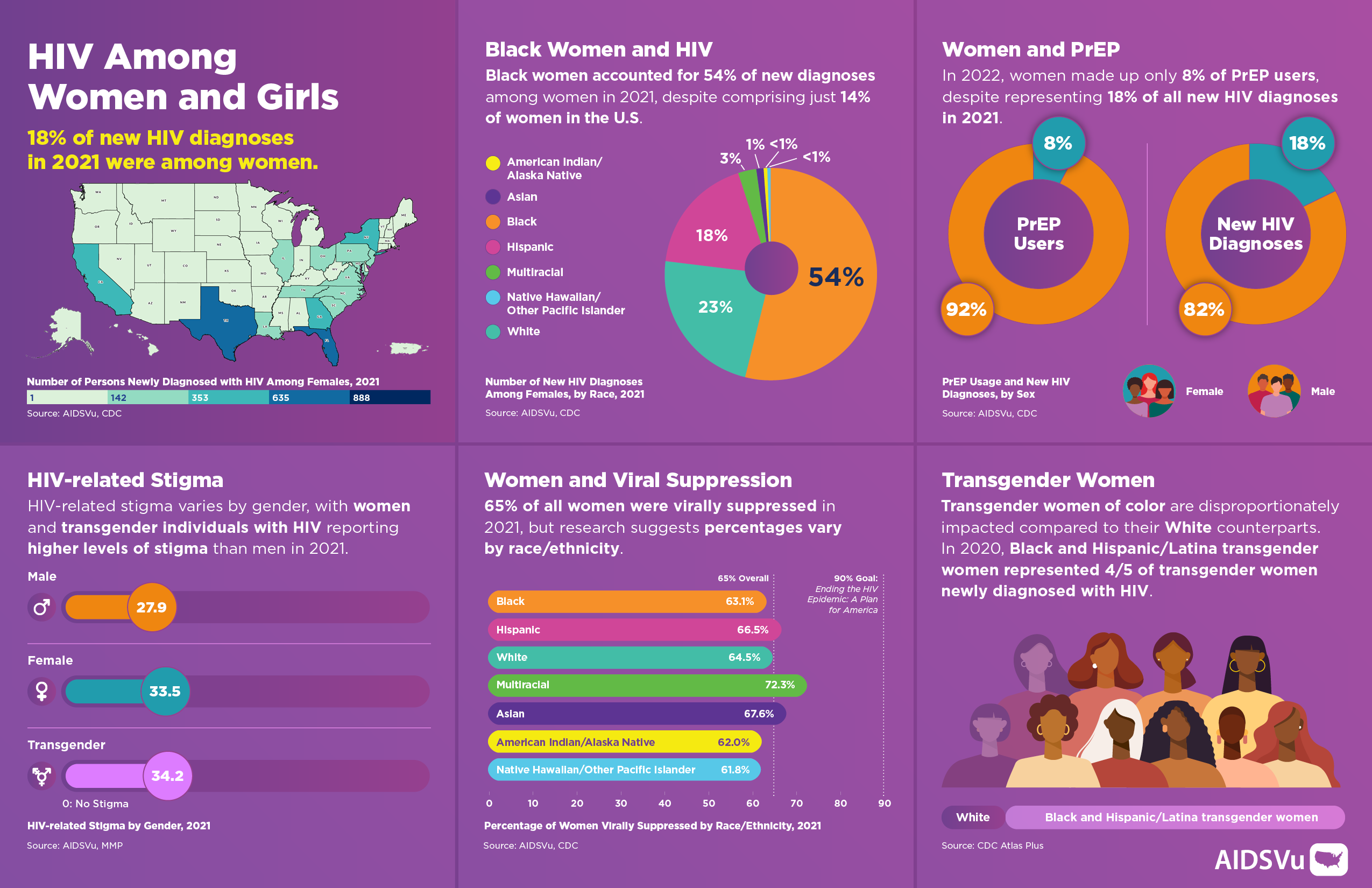
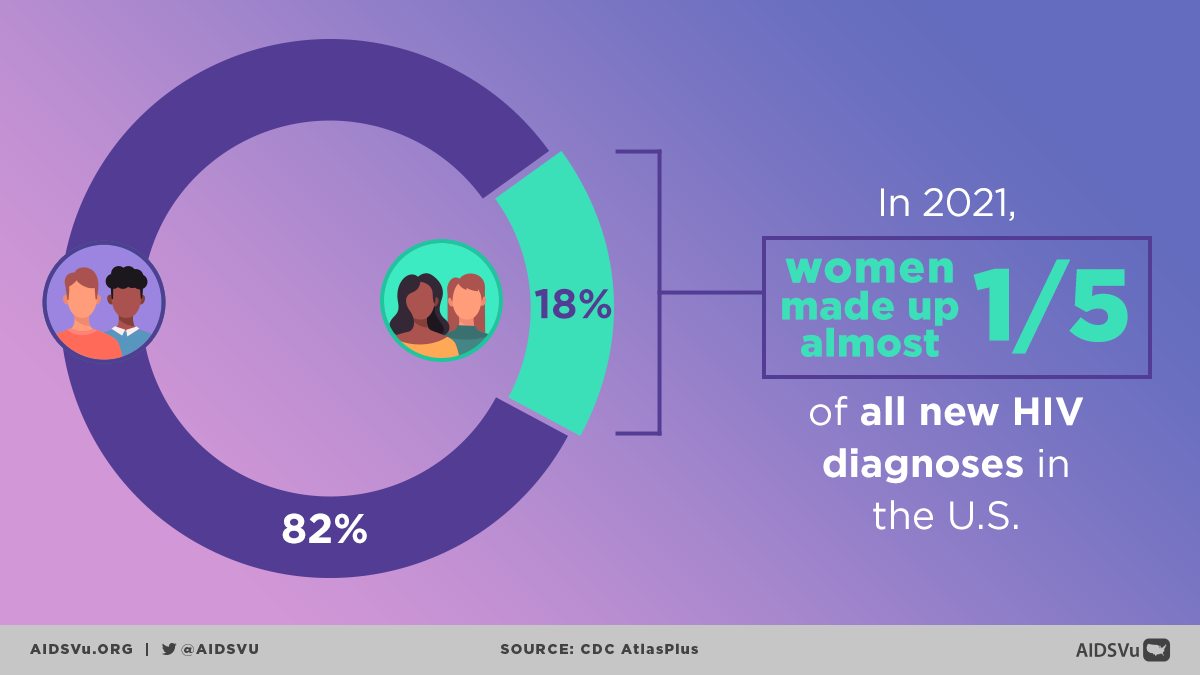
Women continue to bear a significant burden of HIV in the United States, though their experiences are often overshadowed by the epidemic’s disproportionate impact on gay and bisexual men. In 2023, 19% (7,350) of all new HIV diagnoses were among women, and women represent approximately 23% of all people living with HIV. These numbers represent not just statistics but individual lives affected by complex interactions of gender, race, poverty, and systemic inequities that shape vulnerability to HIV.
The HIV epidemic among women is fundamentally an epidemic of inequity. Most women who acquire HIV face multiple, intersecting disadvantages that increase their risk of exposure and limit their access to prevention and care services. Understanding HIV among women requires examining not only individual behaviors but also the social, economic, and structural conditions that create environments where HIV transmission occurs.
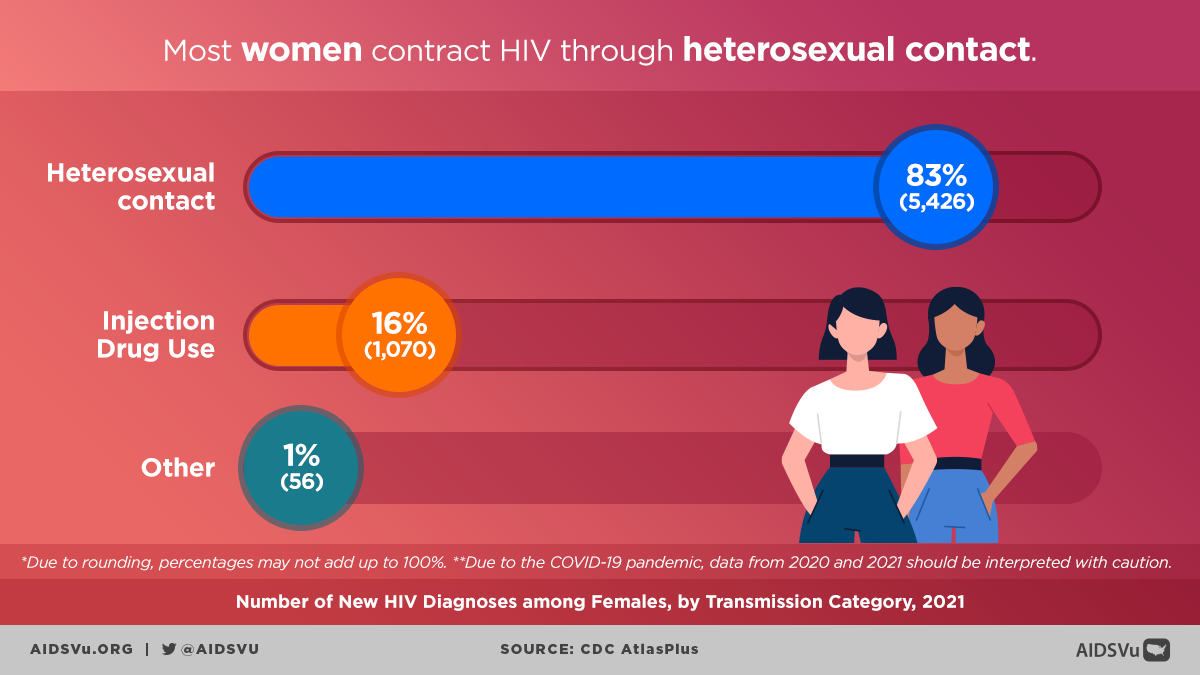
The most common route of HIV transmission for women is heterosexual contact with a male partner who has HIV. This mode of transmission accounts for the vast majority of new infections among women, highlighting how women’s HIV risk is often tied to factors beyond their direct control, including their partners’ risks, behaviors, and HIV status awareness.
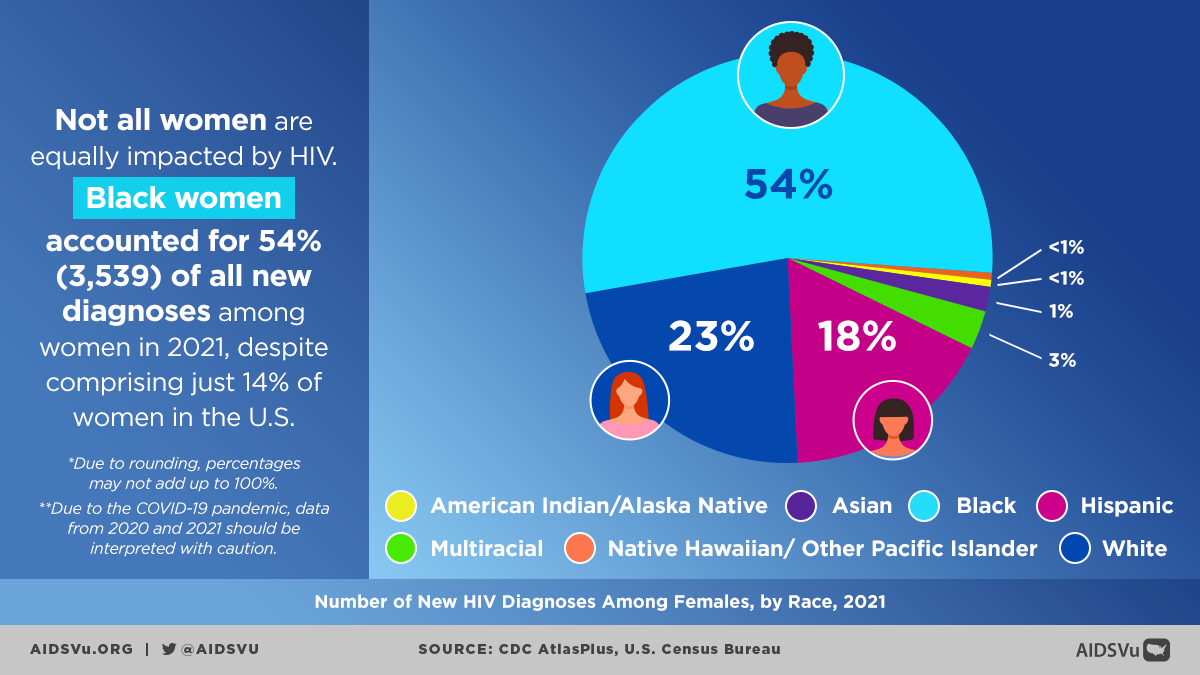
Black Women: Bearing the Greatest Burden
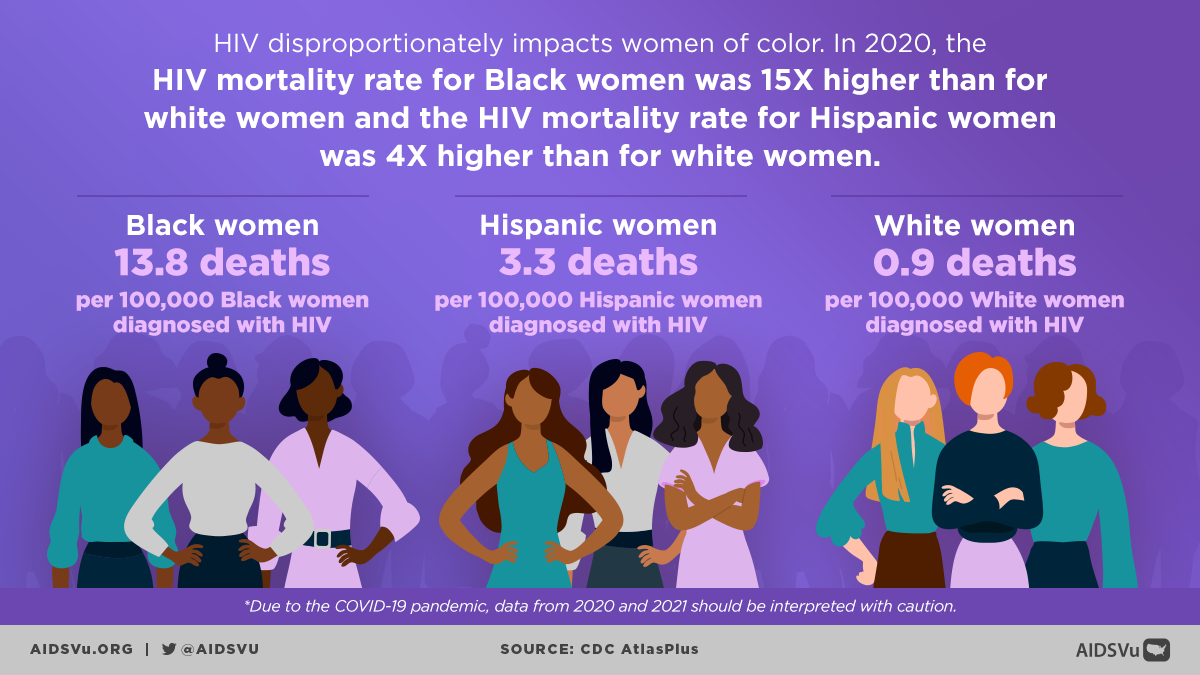
The HIV epidemic among women is heavily concentrated among Black women, who face extraordinarily high rates of infection that reflect the intersection of racism, sexism, and poverty. Black women accounted for half (50%) of HIV diagnoses among women but represent only 13% of the female population. This represents a diagnosis rate that is dramatically higher than women of other racial and ethnic groups.
Black women had the highest HIV diagnosis rate (19.6 per 100,000), which was 3 times the rate among Hispanic/Latino women (6.7) and 11 times the rate among White women (1.8). These stark disparities reflect not individual choices but rather systematic inequities that have created conditions of vulnerability for Black women.
The Structural Roots of Disparity
The disproportionate impact of HIV on Black women cannot be understood without examining the historical and contemporary structural factors that create risk:
- Economic Inequality: Black women experience poverty at higher rates than other groups, limiting their ability to negotiate safer sexual practices, access healthcare, and leave relationships that may put them at risk.
- Geographic Concentration: Many Black women live in areas with high HIV prevalence, creating community-level factors that increase risk of exposure to HIV.
- Healthcare Barriers: Systematic racism in healthcare, limited access to quality reproductive health services, and provider bias all create barriers to HIV prevention and care for Black women.
- Mass Incarceration: The high rates of incarceration among Black men create disrupted social networks and relationships that can increase HIV transmission risk within Black communities.
- Limited Partner Options: The intersection of racism and economic marginalization can limit Black women’s pool of potential partners, potentially increasing the likelihood of relationships with men who have undisclosed HIV risk factors.
A Love Letter to Black Women
The Role of Heterosexual Transmission
Among Black women living with HIV, approximately 85% of infections are attributed to heterosexual contact. This highlights several critical issues:
- Partner Risk Factors: Many women acquire HIV from male partners who may be unaware of their own HIV status, use injection drugs, have sex with men, or have other HIV risk factors.
- Power Dynamics: Gender-based power imbalances can limit women’s ability to negotiate condom use, request HIV testing, or discuss sexual histories with partners.
- Hidden Risk: Many women may not perceive themselves as being at risk for HIV, particularly in long-term relationships or marriages, leading to delayed testing and diagnosis.
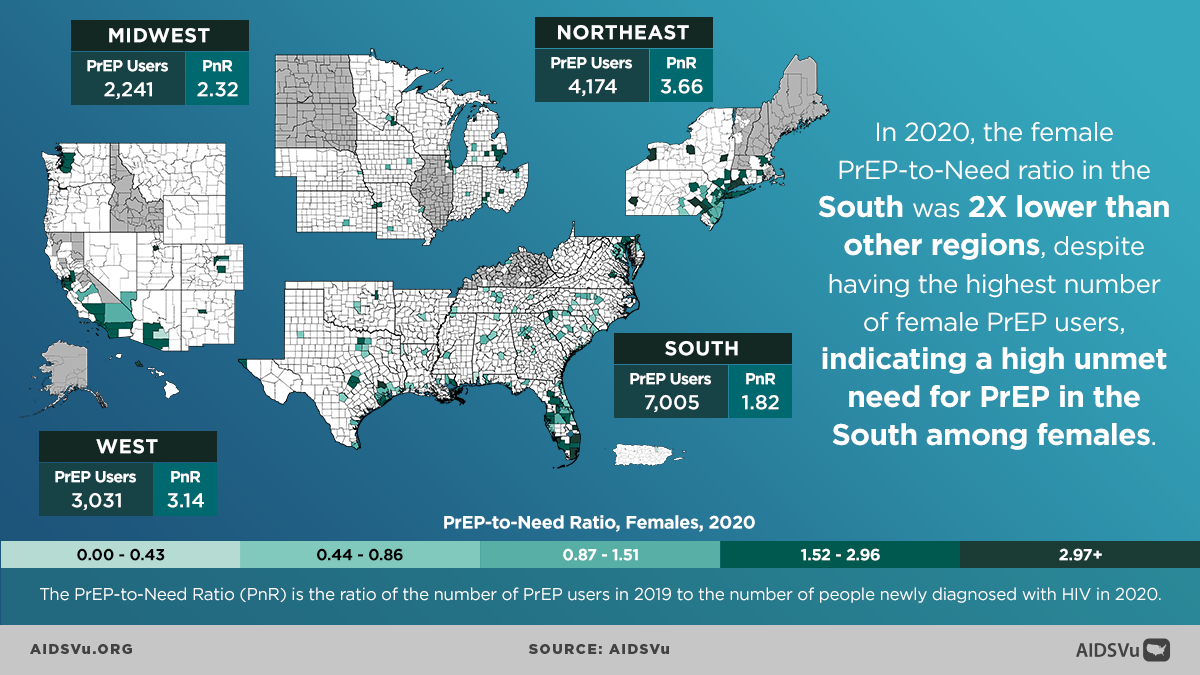
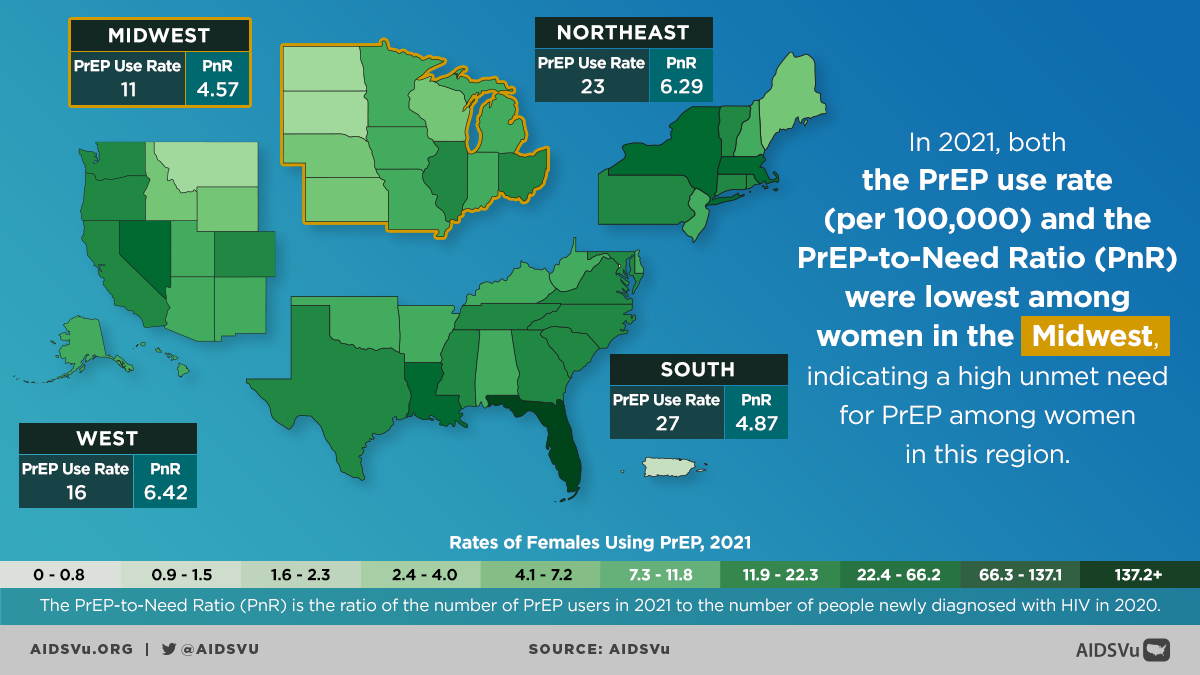
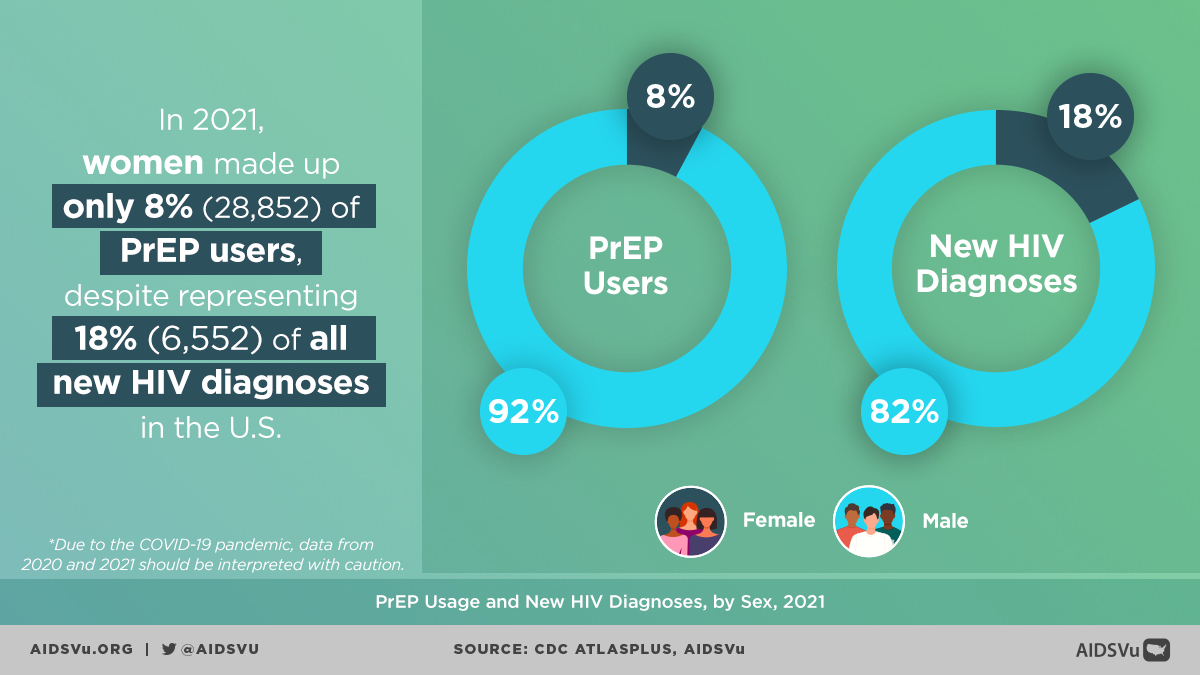
The Prevention Gap: PrEP Utilization Among Women
One of the most significant challenges in HIV prevention for women is the dramatic underutilization of pre-exposure prophylaxis (PrEP) relative to both need and awareness. The gap between PrEP availability and utilization among women represents a critical missed opportunity in HIV prevention.
The Numbers Tell the Story
The disparity in PrEP use by gender is stark and concerning. While women comprised 19% of new HIV diagnoses in 2023, they represent a much smaller proportion of PrEP users. This prevention inequity reflects multiple barriers that prevent women from accessing this highly effective prevention tool.
Barriers to PrEP Access for Women
- Provider Knowledge and Bias: Many healthcare providers lack training in HIV prevention for women and may not routinely discuss PrEP with female patients, particularly heterosexual women.
- Misperceptions of Risk: Both providers and women themselves may underestimate HIV risk among women, particularly those in seemingly stable relationships.
- Healthcare Access: Women may lack regular access to healthcare providers who are knowledgeable about and comfortable prescribing PrEP.
- Insurance: Coverage limitations can make PrEP inaccessible, particularly for women experiencing economic instability.
- Stigma and Disclosure Concerns: Women may be concerned about stigma associated with taking HIV prevention medication or may worry about having to disclose PrEP use to partners.
- Side Effect Concerns: Real or perceived concerns about side effects, particularly those that might affect reproductive health, can deter women from starting or continuing PrEP.
- Complex Lives: Women often juggle multiple responsibilities as caregivers, workers, and community members, making it challenging to maintain regular healthcare appointments and medication schedules required for PrEP.
- Addressing the PrEP Gap
Closing the PrEP utilization gap among women requires comprehensive approaches that address both individual and structural barriers:
- Provider Education: Healthcare providers need training on identifying HIV risk among women, discussing PrEP appropriately, and addressing women’s specific concerns and questions.
- Community-Based Services: PrEP programs that meet women where they are—in community health centers, reproductive health clinics, and community-based organizations—can improve access.
- Integrated Care: Incorporating PrEP services into routine reproductive health care, family planning services, and other healthcare encounters can normalize HIV prevention for women.
- Addressing Stigma: Community education and messaging that destigmatizes HIV prevention and positions PrEP as a tool for sexual health empowerment rather than risk compensation.
- Economic Support: Programs that address cost barriers through insurance navigation, patient assistance programs, and free or low-cost services.
Transgender Women: Extraordinary Vulnerability
Transgender women face some of the highest rates of HIV infection of any population group in the United States, with particularly acute disparities among transgender women of color. However, transgender women are often invisible in discussions of HIV among women due to data limitations and systematic exclusion from women’s health programs and research.
The Data Challenge
Because most medical providers don’t systematically collect information on both sex assigned at birth and current gender identity, HIV surveillance data systematically undercount HIV cases among transgender women. This invisibility in data translates to invisibility in program planning, resource allocation, and policy development.
Available data, while limited, reveals extraordinarily high HIV prevalence among transgender women. In studies conducted in major cities, HIV prevalence among transgender women has been found to be as high as 42% overall, with even higher rates among Black transgender women (62% in some studies).
Unique Risk Factors for Transgender Women
Transgender women face a unique constellation of risk factors that create extraordinary vulnerability to HIV:
Discrimination and Marginalization: Systematic discrimination in employment, housing, healthcare, and education pushes many transgender women into economic survival situations that may increase HIV risk.
- Healthcare Barriers: Transgender women often experience discrimination, harassment, and inadequate care in healthcare settings, leading many to avoid healthcare entirely.
- Hormone Use: Some transgender women may obtain hormones through informal channels or share injection equipment, creating potential HIV transmission risk.
- Sex Work: Economic marginalization may push some transgender women into sex work, often in situations where they have limited power to negotiate safer practices.
- Intimate Partner Violence: Transgender women experience high rates of intimate partner violence, which can increase HIV risk through multiple pathways.
- Mental Health Challenges: High rates of depression, anxiety, and substance use among transgender women, often resulting from minority stress and discrimination, can increase HIV vulnerability.
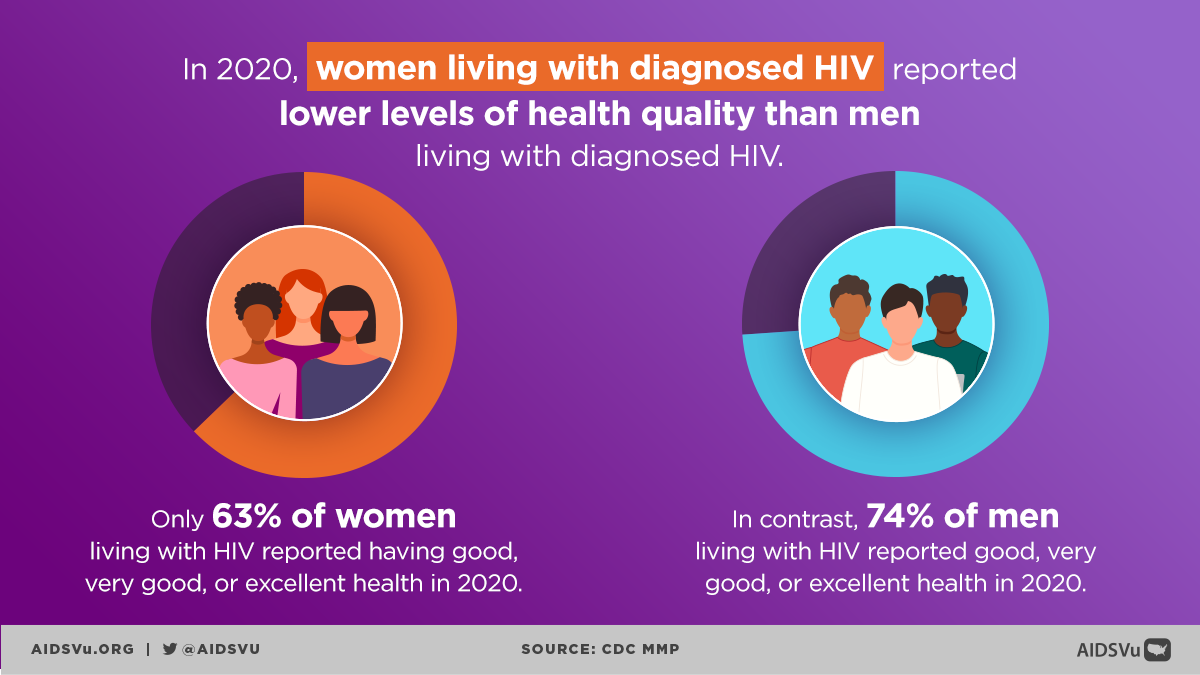
Health Disparities and Structural Determinants
HIV among women cannot be understood without examining the broader context of health disparities that affect women’s health outcomes across multiple domains. Women with HIV face intersecting challenges that extend far beyond HIV itself.
Economic Vulnerability
Many women living with HIV face significant economic challenges. The financial burden of HIV care, combined with employment discrimination and the stigma associated with HIV, often leads to loss of income and financial instability. This economic vulnerability creates cascading effects:
- Healthcare Access: Economic instability can limit access to consistent, high-quality HIV care and treatment.
- Housing Stability: Financial challenges can lead to housing instability or homelessness, which directly affects health outcomes and treatment adherence.
- Food Security: Economic hardship can lead to food insecurity, which can interfere with medication adherence and overall health.
- Competing Priorities: Women facing economic hardship may need to prioritize immediate survival needs over long-term health management.
Geographic Disparities
Living in low-income areas significantly impacts HIV risk and outcomes for women. These areas often have:
- Limited Healthcare Infrastructure: Fewer HIV specialists, limited clinic hours, and long waiting times for appointments.
- Higher HIV Prevalence: Community-level factors that increase the likelihood of HIV exposure.
- Fewer Economic Opportunities: Limited employment options and educational resources that could improve economic stability.
- Social Determinants: Higher rates of poverty, housing instability, and other social factors that increase HIV vulnerability.
Research and Representation Gaps
Much of the existing HIV research in the United States has historically focused on men, particularly gay and bisexual men, leading to significant knowledge gaps about HIV in women. This research bias has several consequences:
- Limited Understanding: Insufficient knowledge about the biological, behavioral, and social factors that specifically affect HIV risk and outcomes in women.
- Treatment Protocols: HIV treatment guidelines and protocols that may not adequately address women’s specific needs and concerns.
- Prevention Strategies: Prevention approaches that may not be optimally designed for women’s experiences and contexts.
- Clinical Trials: Underrepresentation of women in HIV clinical trials, limiting the evidence base for treatment recommendations.
HIV Stigma and Women’s Experiences
Women living with HIV often experience unique forms of stigma that intersect with gender-based discrimination and social expectations about women’s roles and sexuality. HIV-related stigma varies by gender, with women and transgender individuals reporting higher levels of stigma than men.
Gender-Specific Stigma
Women with HIV may face particular stigma related to:
- Sexuality and Morality: Judgmental attitudes about women’s sexual behavior and assumptions about how they acquired HIV.
- Motherhood and Reproduction: Stigma related to pregnancy, childbearing, and parenting among women with HIV.
- Caregiver Roles: Challenges in fulfilling expected roles as caregivers and family nurturers while managing HIV.
- Beauty and Femininity Standards: Concerns about physical changes related to HIV or treatment that may affect appearance.
Impact on Health Outcomes
HIV-related stigma has direct consequences for women’s health outcomes:
- Delayed Testing: Fear of stigma may prevent women from seeking HIV testing.
- Treatment Adherence: Stigma can interfere with medication adherence and engagement in care.
- Disclosure Decisions: Complex decisions about when, how, and to whom to disclose HIV status.
- Mental Health: Increased risk of depression, anxiety, and social isolation.
The HIV Care Continuum for Women
Women’s experiences along the HIV care continuum—from testing through viral suppression—are shaped by the multiple structural and social factors that affect their lives.
Testing and Diagnosis
Many women living with HIV are diagnosed later in the course of infection compared to men, often because:
- Limited Risk Perception: Both women and their healthcare providers may not recognize HIV risk factors.
- Healthcare Access: Irregular healthcare access can delay testing and diagnosis.
- Testing Practices: HIV testing may not be routinely offered in healthcare settings that women typically access.
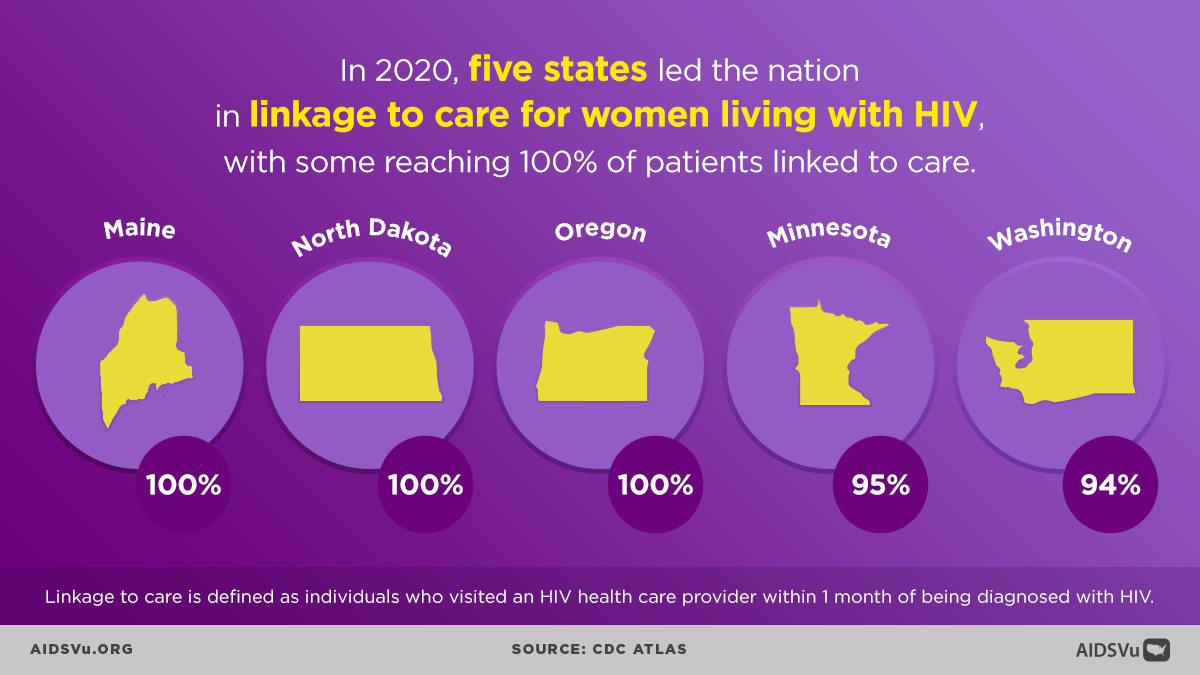
Engagement and Retention in Care
Once diagnosed, women face various challenges in engaging and remaining in HIV care:
Competing Priorities: Women’s roles as caregivers for children, elderly parents, and others may interfere with their own healthcare.
Transportation and Childcare: Practical barriers such as lack of transportation or childcare can prevent regular clinic attendance.
Provider Relationships: The quality of relationships with healthcare providers significantly affects women’s engagement in care.
Mental Health: Depression, anxiety, and trauma can interfere with care engagement.
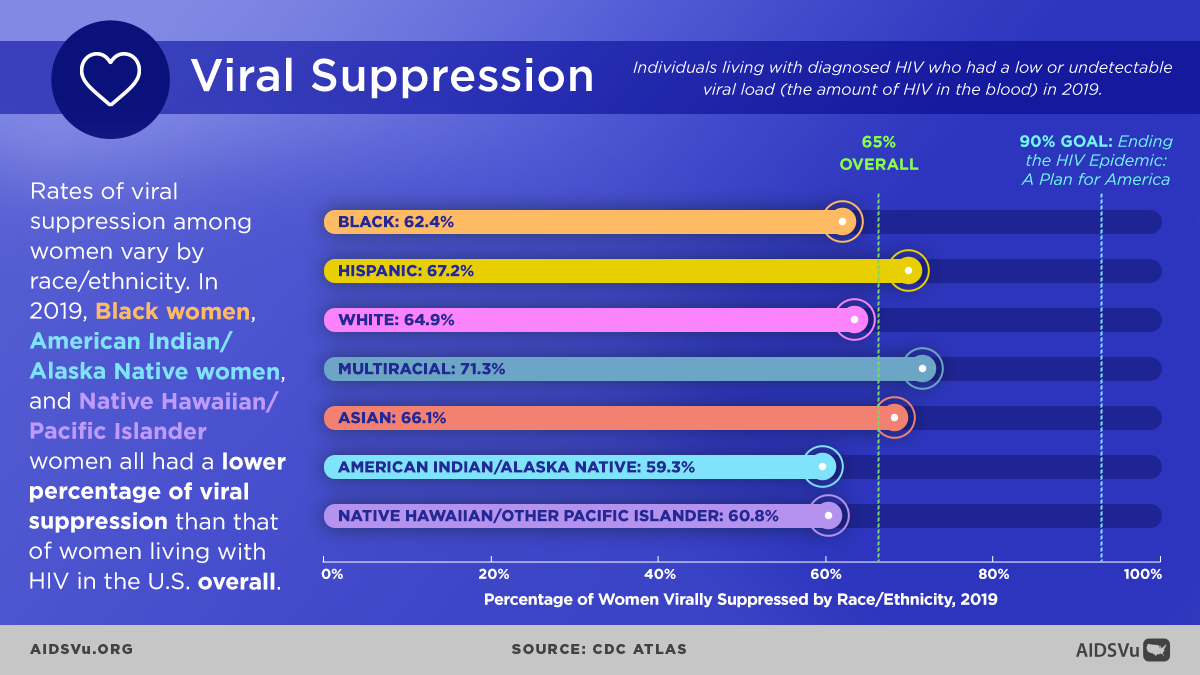
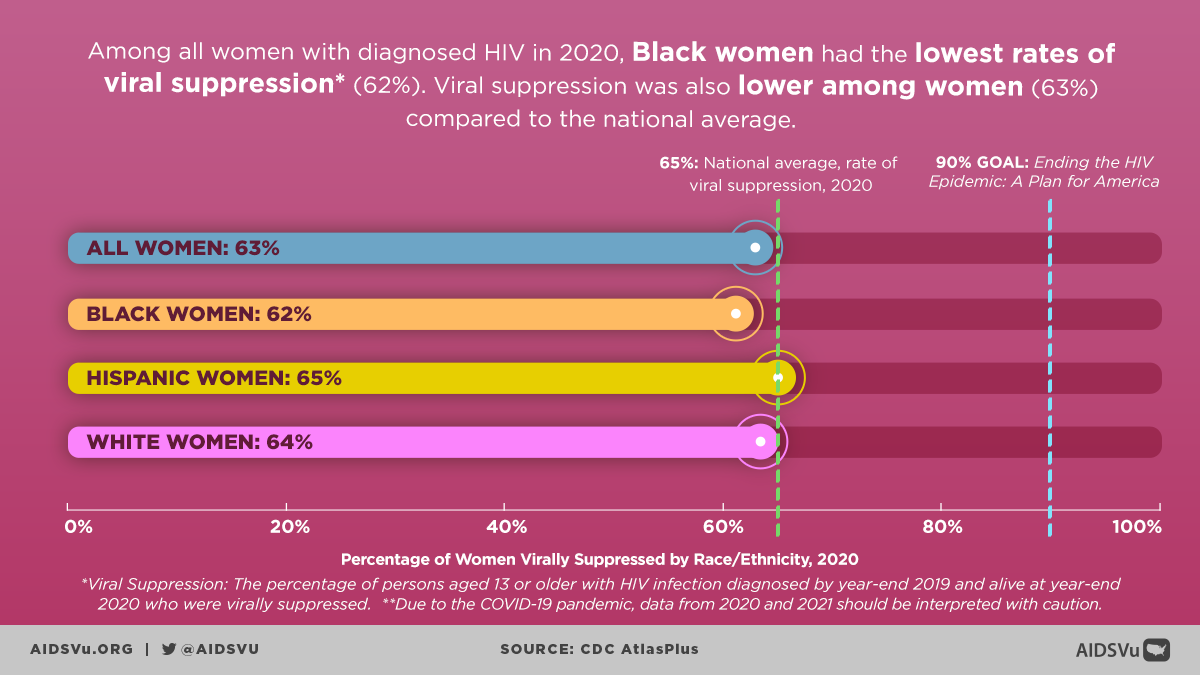
Viral Suppression Outcomes
While many women achieve viral suppression with appropriate treatment, disparities persist across racial and ethnic groups. Factors affecting viral suppression include:
- Treatment Adherence: Multiple factors can interfere with consistent medication taking.
- Side Effects: Concerns about medication side effects, particularly those affecting appearance or reproductive health.
- Social Support: The availability of supportive relationships affects treatment success.
- Economic Stability: Financial resources affect ability to maintain consistent care and treatment.
Perinatal HIV Transmission: A Public Health Success Story
One of the greatest public health successes in the HIV epidemic has been the dramatic reduction in perinatal HIV transmission. Advances in HIV research, prevention, and treatment have made it possible for people with HIV to give birth to babies who are HIV-free.
The Transformation
The annual number of diagnoses of perinatal HIV in the United States and dependent areas has declined by more than 95% since the early 1990s. This remarkable achievement results from:
- Universal Testing: Routine HIV testing for pregnant women has become standard of care.
- Antiretroviral Therapy: The use of HIV medicines (ART) during pregnancy, delivery, and for the newborn has dramatically reduced transmission risk.
- Cesarean Delivery: When appropriate, planned cesarean delivery can further reduce transmission risk.
- Feeding Recommendations: In the United States, formula feeding is recommended for women with HIV to eliminate transmission risk through breastfeeding.
Current Outcomes
The use of HIV medicines and other prevention strategies have lowered the rate of perinatal transmission of HIV to 1% or less in the United States and Europe. This achievement demonstrates what is possible when comprehensive, evidence-based interventions are systematically implemented.
Remaining Challenges
Despite these successes, challenges remain:
- Late Entry to Care: Some women still enter prenatal care late in pregnancy, limiting opportunities for intervention.
- Substance Use: Substance use during pregnancy can complicate HIV treatment and prevention efforts.
- Mental Health: Depression and other mental health challenges can affect treatment adherence during pregnancy.
- Social Determinants: Poverty, housing instability, and other social factors can interfere with consistent prenatal care.
Looking Forward: Comprehensive Approaches to HIV Prevention and Care for Women
Addressing HIV among women requires comprehensive approaches that recognize the complex intersection of biological, behavioral, social, and structural factors that shape women’s HIV risk and outcomes.
Essential Elements of Effective Programs
- Gender-Responsive Services: HIV prevention and care programs designed with women’s specific needs, experiences, and constraints in mind.
- Integrated Care: Services that address HIV alongside other health needs, including reproductive health, mental health, and substance use treatment.
- Economic Empowerment: Programs that address the economic factors that increase HIV vulnerability and interfere with care engagement.
- Community-Centered Approaches: Programs designed by and for the communities they serve, with meaningful involvement of women living with HIV.
- Structural Interventions: Policies and programs that address the root causes of HIV vulnerability, including poverty, discrimination, and healthcare access barriers.
- Priority Populations
Special attention must be paid to women who face the greatest HIV burden:
- Black Women: Comprehensive programs that address the intersection of racism and sexism in HIV prevention and care.
- Transgender Women: Services that are specifically designed for and affirming of transgender women’s identities and experiences.
- Women with Multiple Vulnerabilities: Integrated services for women experiencing homelessness, substance use, mental health challenges, and involvement with the criminal justice system.
- Young Women: Age-appropriate prevention and care services that recognize the unique needs and development stages of adolescent and young adult women.
The fight against HIV among women is ultimately about gender equity, racial justice, and health equity more broadly. Effective responses require not only biomedical interventions but also fundamental changes to the social and economic conditions that create vulnerability to HIV. Only through such comprehensive approaches can we hope to achieve outcomes for women that reflect their inherent worth and dignity.
Beyond the Map
AIDSVu offers tools and resources beyond the HIV map that provide users with a deeper understanding of the HIV epidemic, its socioeconomic-driving factors, and services available at the community level.
Social Determinants of Health
See how HIV prevalence is related to poverty, high school education, median household income, etc.
Learn MoreFind Services
Use the testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services locators to find critical HIV/AIDS services near you.
Learn MoreLocal Data
View city and state profiles with local HIV/AIDS statistics, national comparison charts, and local resources.
Learn More5 Ways to Use AIDSVu
Explore Maps
Explore the interactive map, customize your view, and easily print for presentations, grant applications, or other materials.
Learn MoreView Local Statistics
View local statistics for your city or state, and download high-impact data visualizations for your work
Learn MoreDownload Data
Download the datasets that inform AIDSVu’s visualizations for your own research and analysis
Learn MoreLocate Services
Use AIDSVu’s service locators to find HIV testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services near you
Learn MoreFor More Information
Learn more about the impact of HIV in Black communities with the following additional resources.