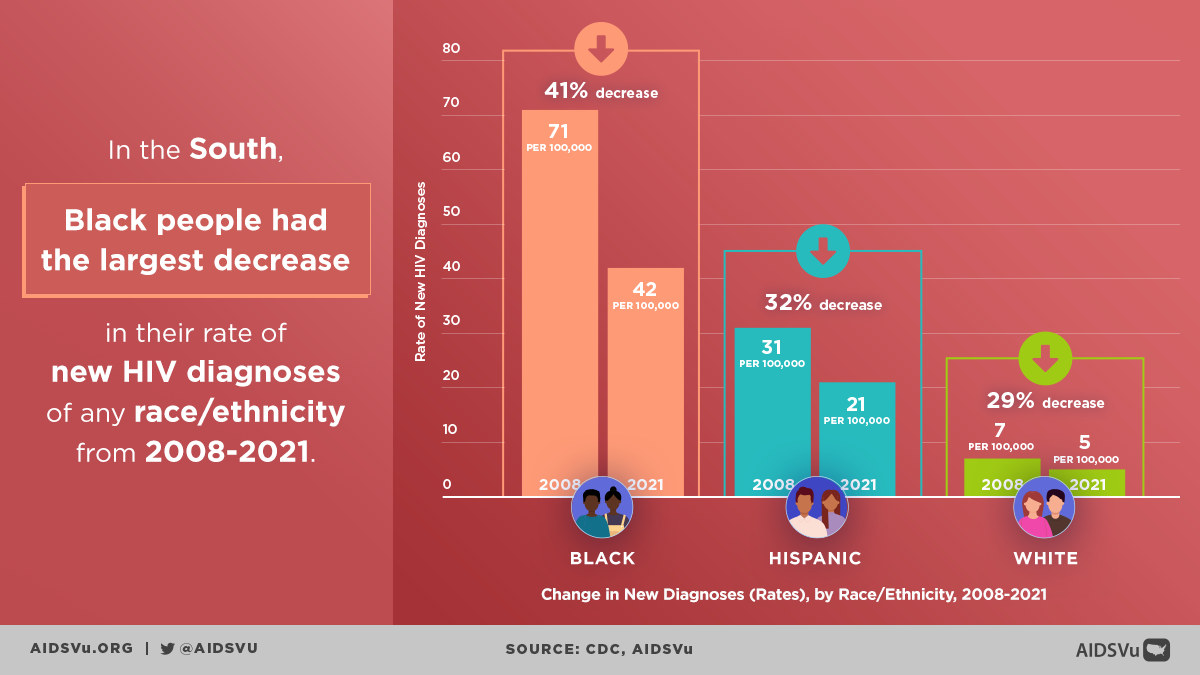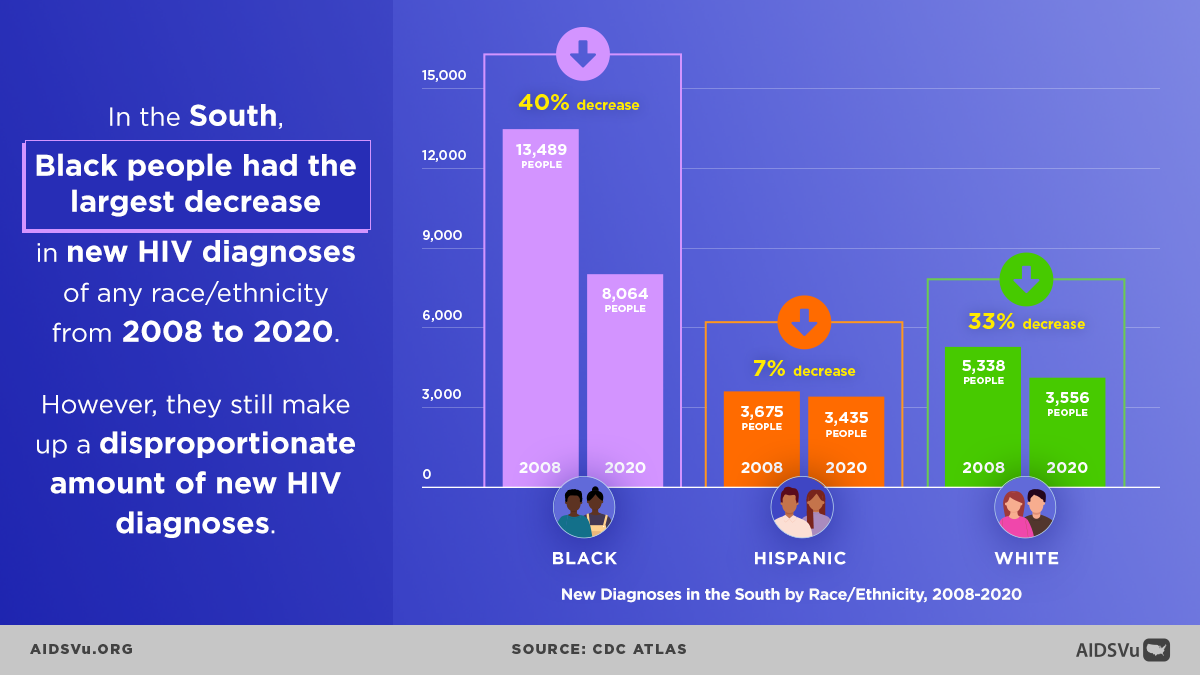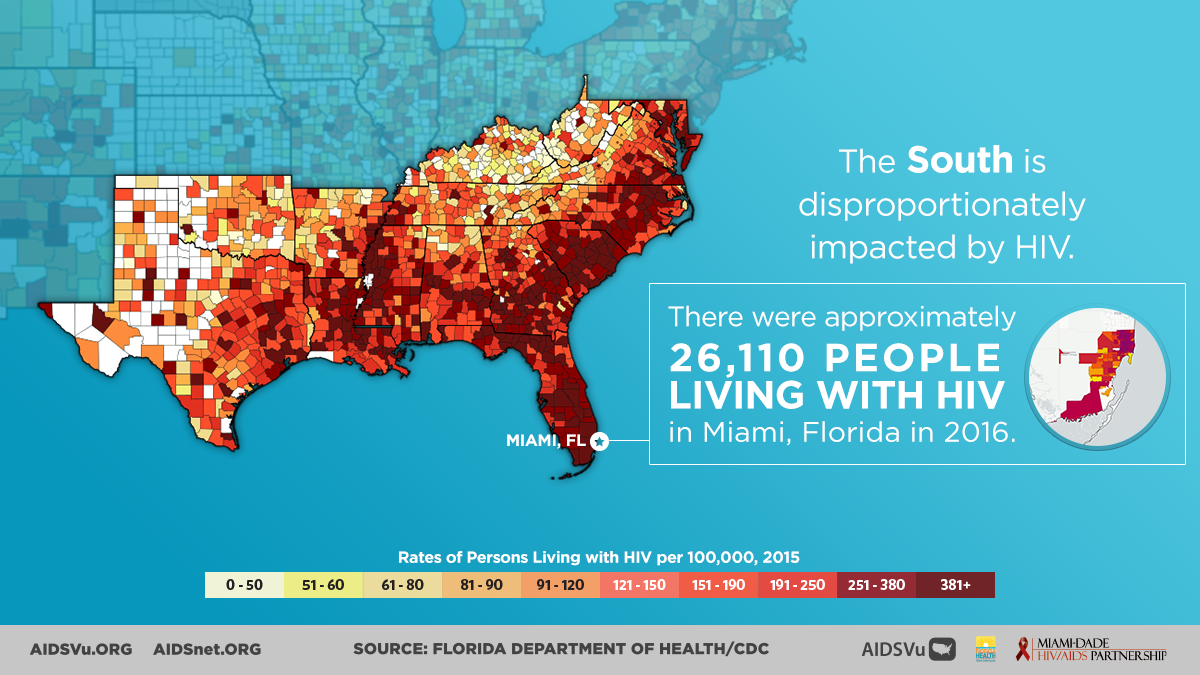
The South experiences a higher burden of HIV compared to other regions across the country, especially among communities of color.
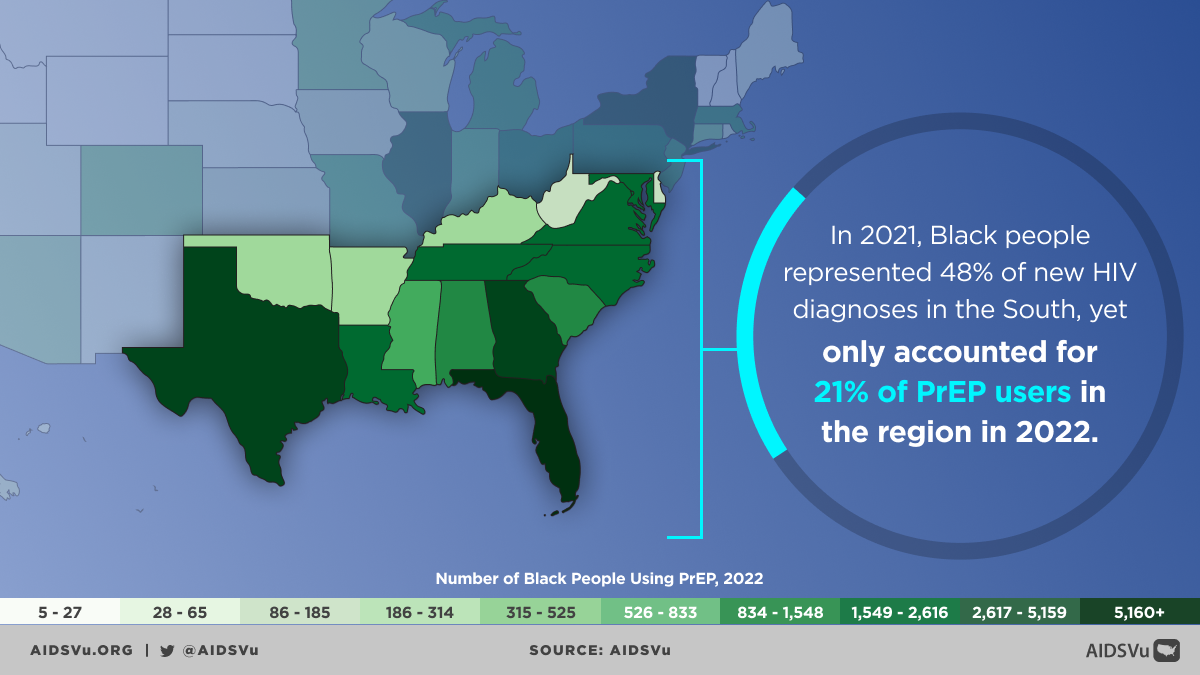
Black Americans in the South represented half of all new HIV diagnoses in the region in 2022, despite comprising only 19% of the Southern population. Additionally, Black people only accounted for 21% of PrEP users in the South in 2023.
Factors Driving the HIV Epidemic in the South
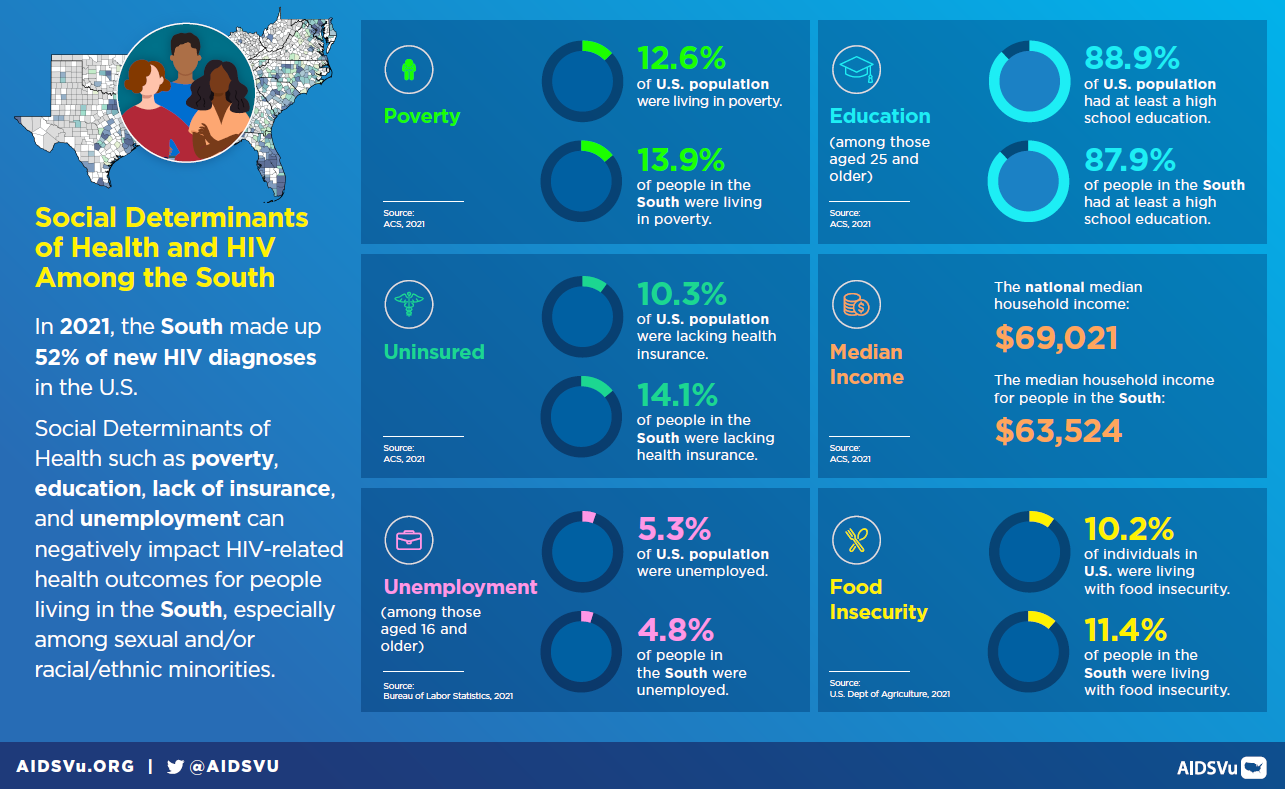
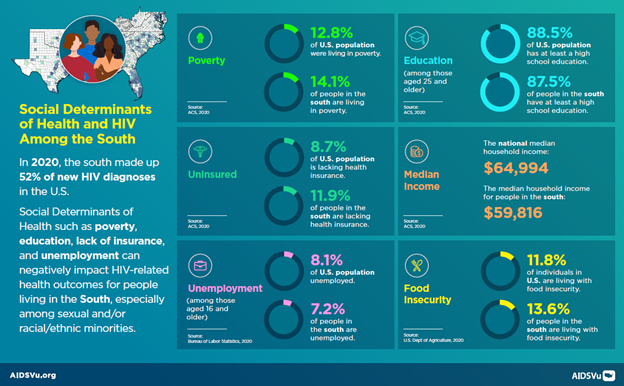
The heavy burden of HIV in the South, especially in those states considered the “Deep South” (defined as Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas), is driven in part by socioeconomic factors like poverty and unemployment.
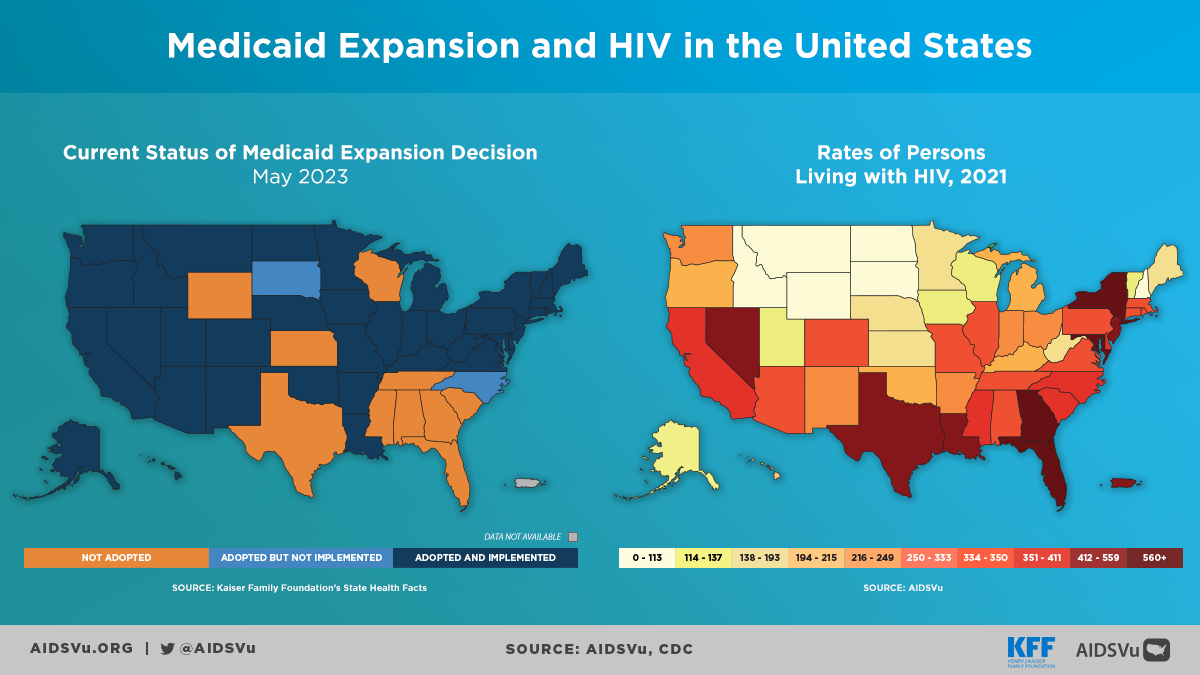
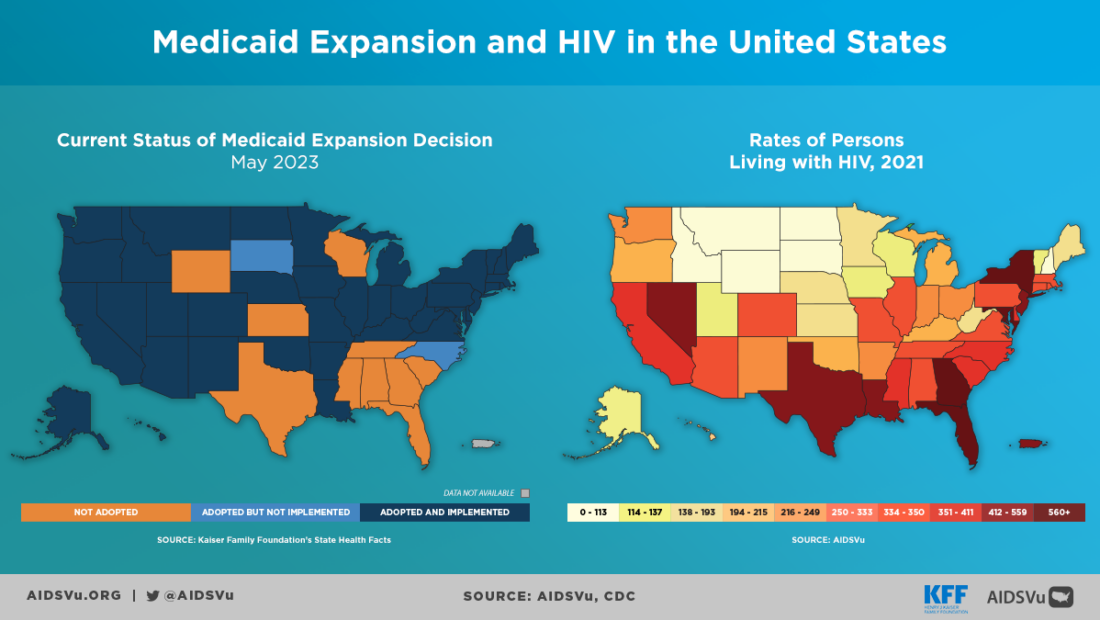
The South has the highest poverty rate and lowest median household income compared to other regions of the U.S. Both factors are associated with poorer health outcomes and may contribute to a higher concentration of HIV and other chronic diseases like diabetes in the region. People in the South face several access barriers that can prevent them from receiving adequate HIV and other health care services. Nearly half of all Americans without health insurance live in the South. Medicaid is the largest source of coverage for people with HIV in the U.S., but as of 2023, nine of 17 states in the South have not expanded Medicaid.
In 2023, states that had expanded Medicaid programs had an average PrEP use rate that was 1.4X higher compared with states that did not have expanded Medicaid.
In rural areas, people with or at risk for HIV face challenges in accessing consistent HIV prevention and treatment services, like lack of public transportation, longer travel time to receive care, and reduced availability of medical and social services compared to non-rural areas. These places may also experience health care provider shortages and have fewer providers with expertise in treating HIV. Cultural factors may also play a key role in driving the southern HIV epidemic.
HIV stigma is pervasive in the South and is often associated with stigma around sexual orientation, substance abuse disorder, poverty, and sex work, and may limit people’s willingness to disclose their HIV status or seek testing, care, or prevention services. Stigma has been associated with lower or delayed access to care due to perceived discrimination from healthcare providers.
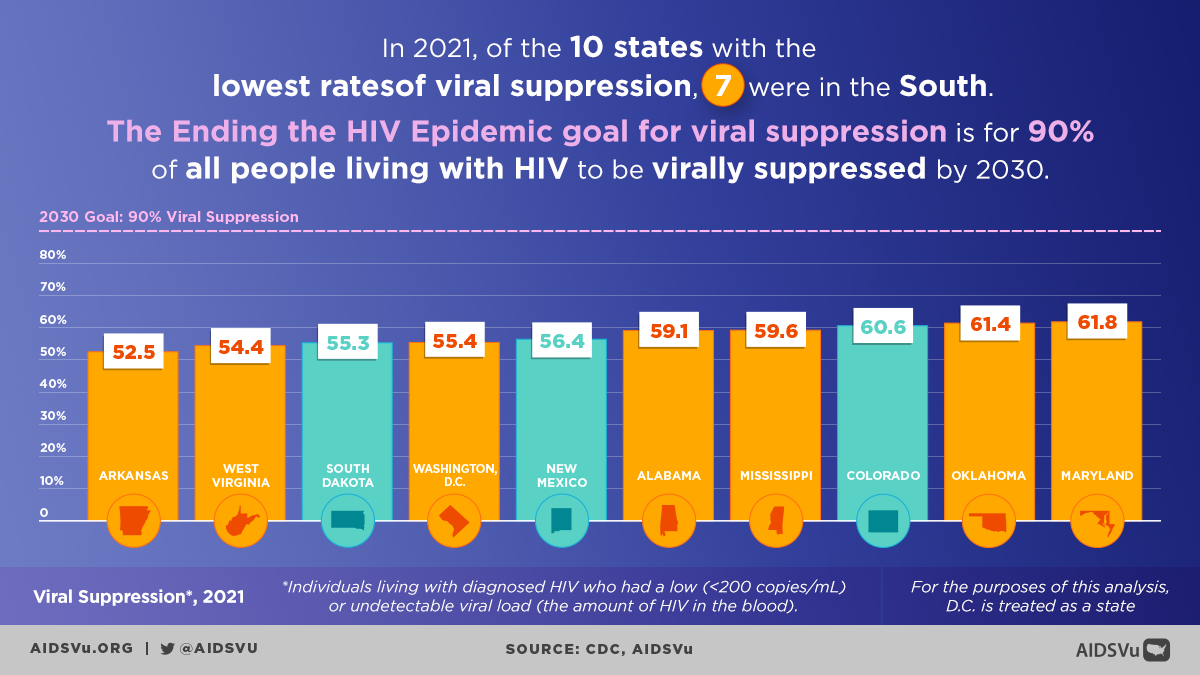
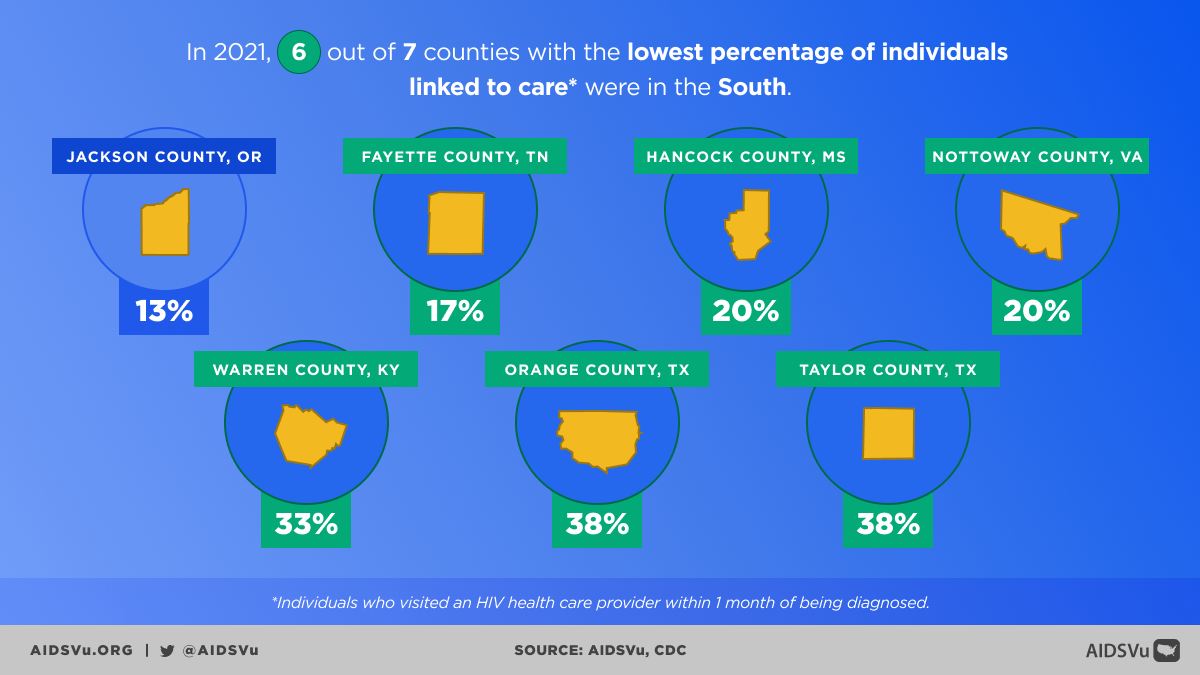
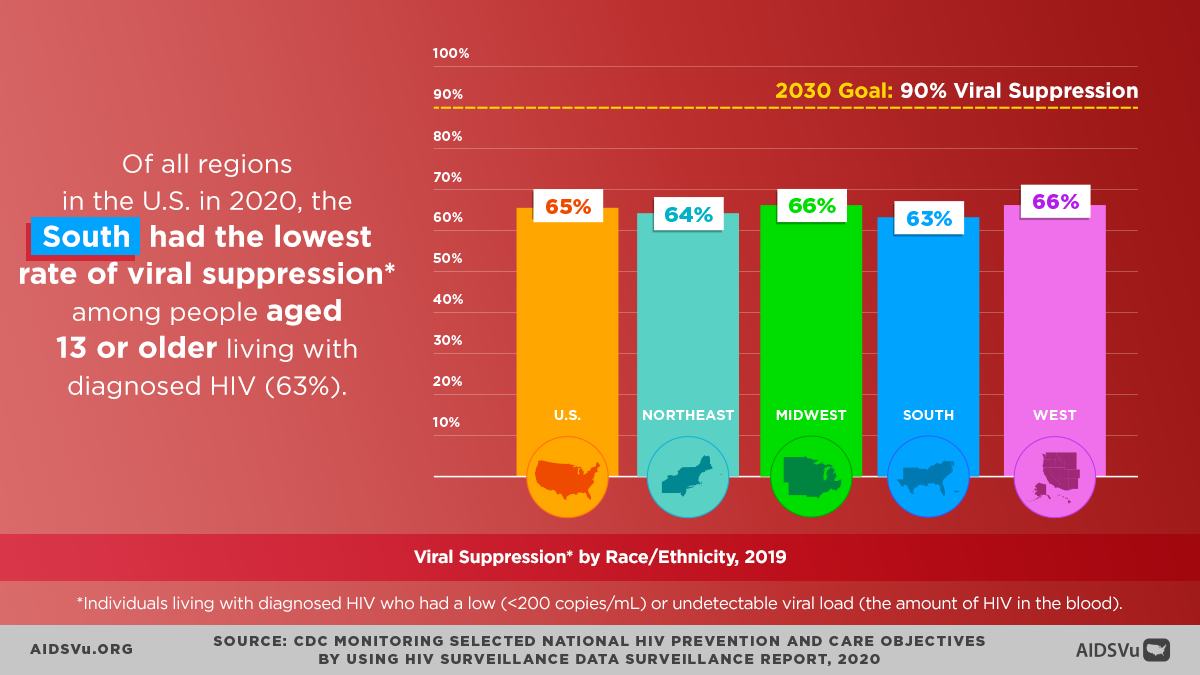
Southern states generally lag behind other regions in key prevention and care outcomes like knowledge of HIV status, linkage to care and viral suppression. One factor may be failure to apply key technologies. For example, southern states have not yet widely adopted new HIV prevention advances, such as antigen/antibody combination HIV tests. These new tests can detect HIV in its early stages, when it is most easily transmitted. Being able to diagnose HIV early is critical to ensure people with HIV get treatment to protect their health and prevent transmitting HIV to their partners.
Predominantly in non-urban areas of the South, the nation’s opioid crisis has increased risk for acquiring HIV and Hepatitis C. According to a 2016 estimate, nearly seven in 10 (68%) counties vulnerable to an HIV or Hepatitis C outbreak among people who inject drugs are in the South.
Ending the HIV Epidemic in the South
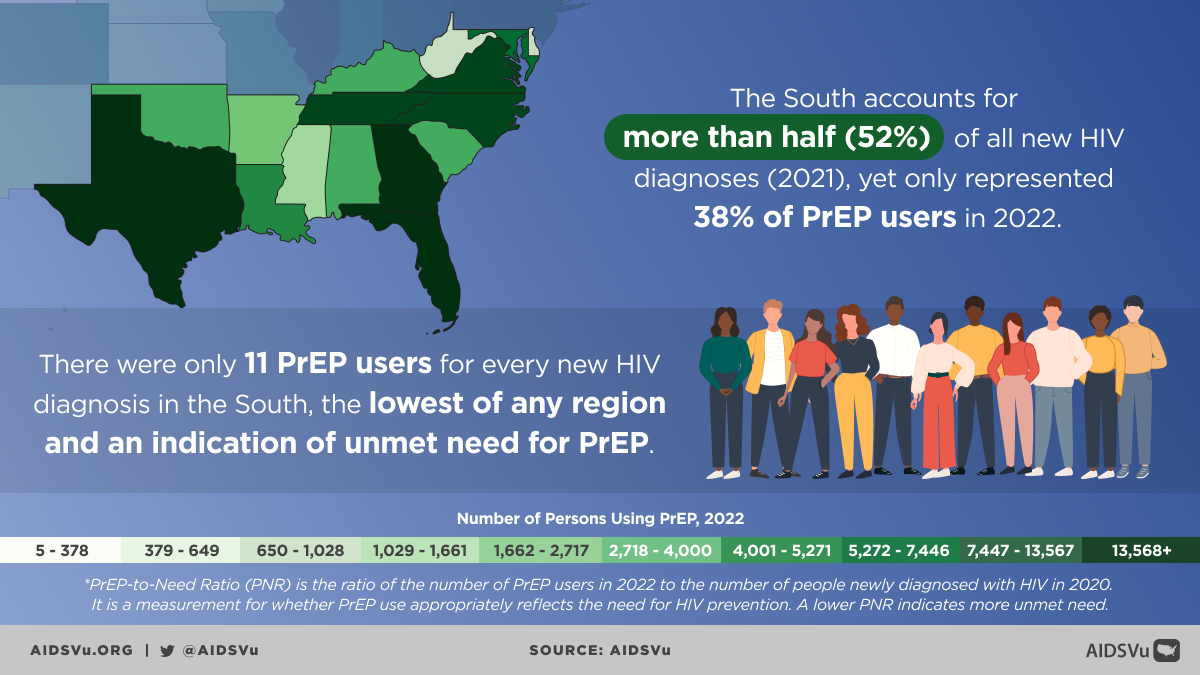
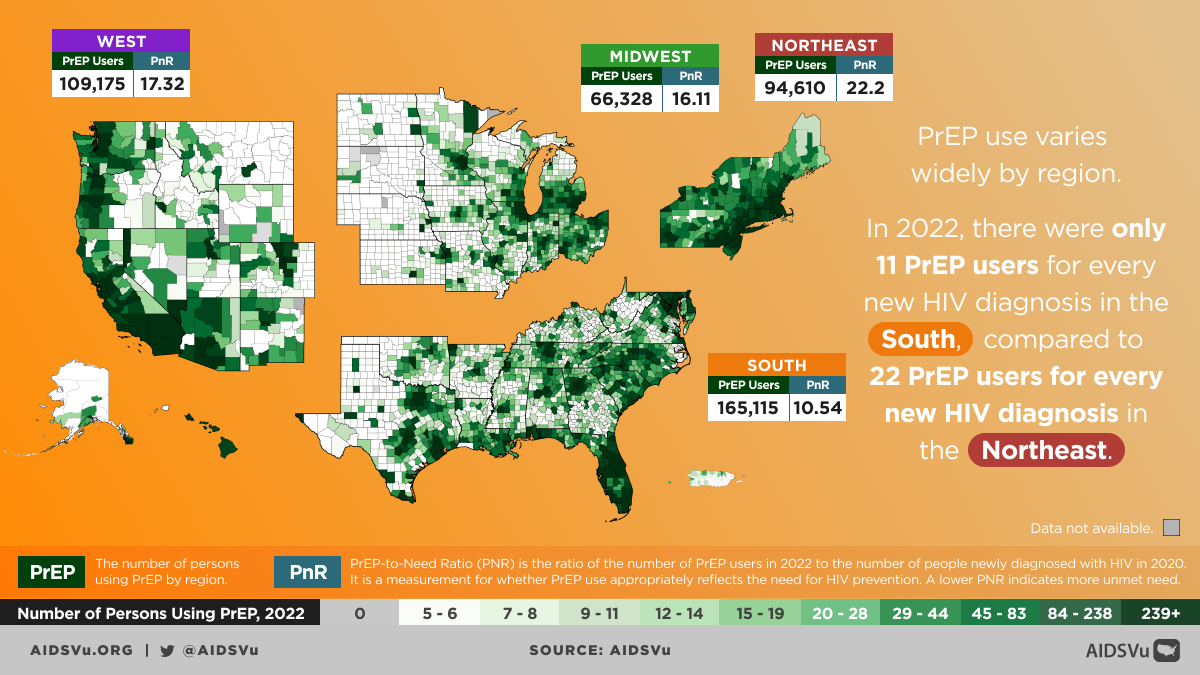
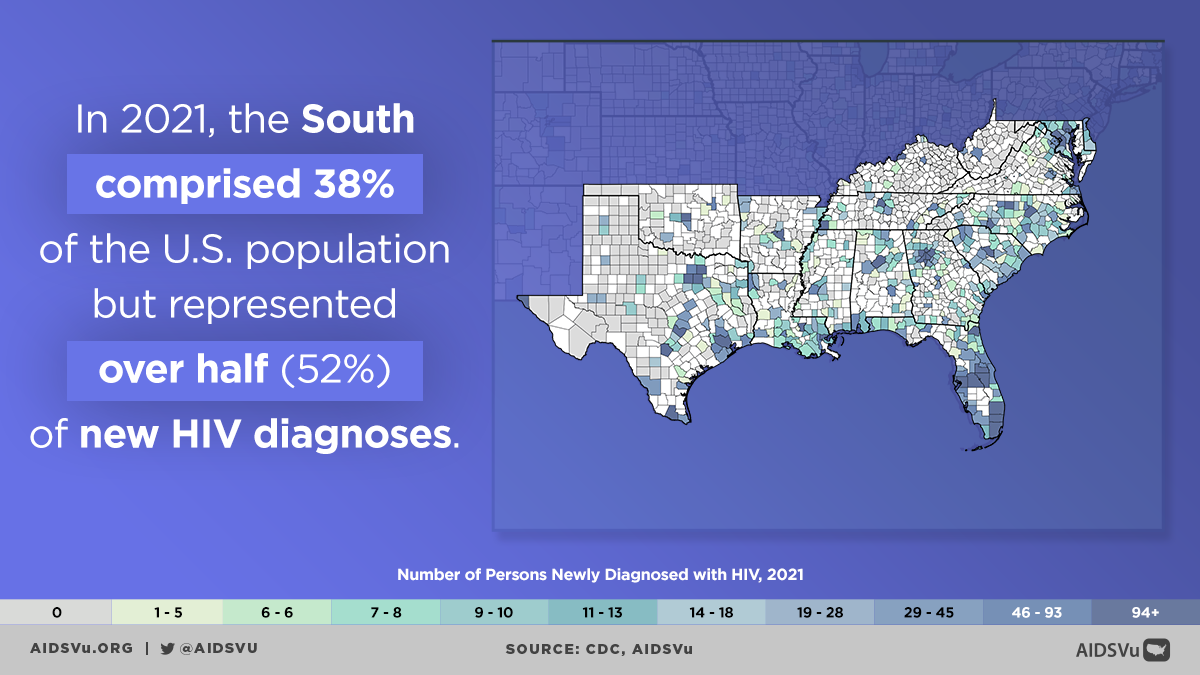
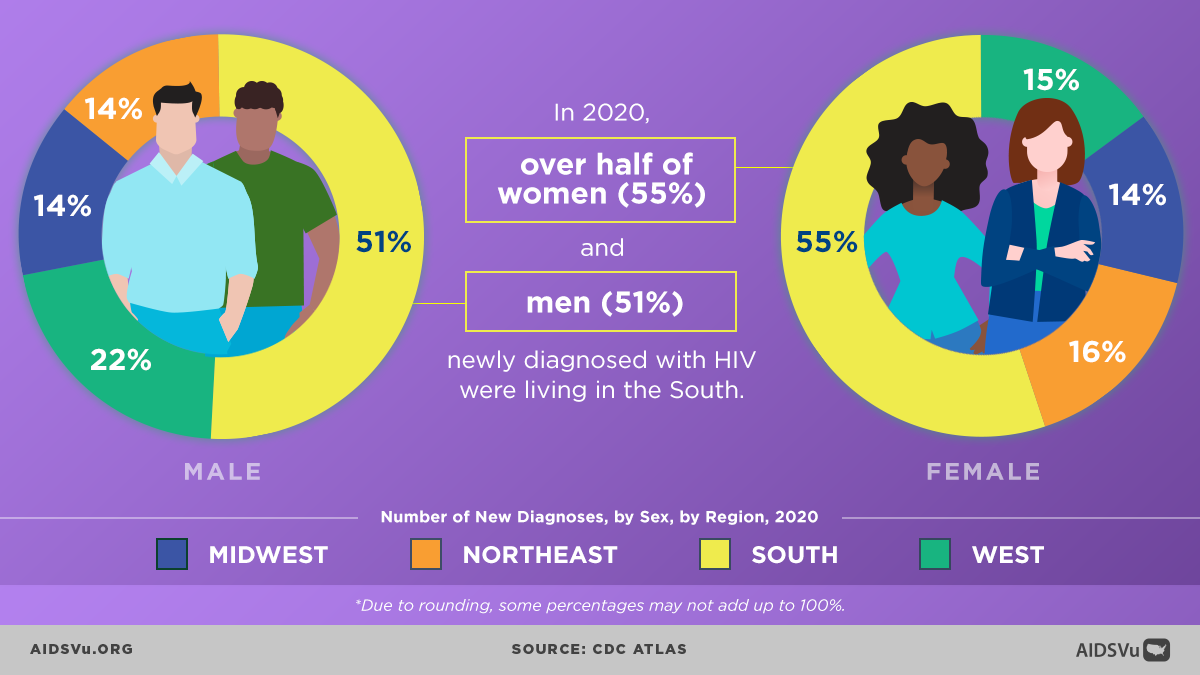
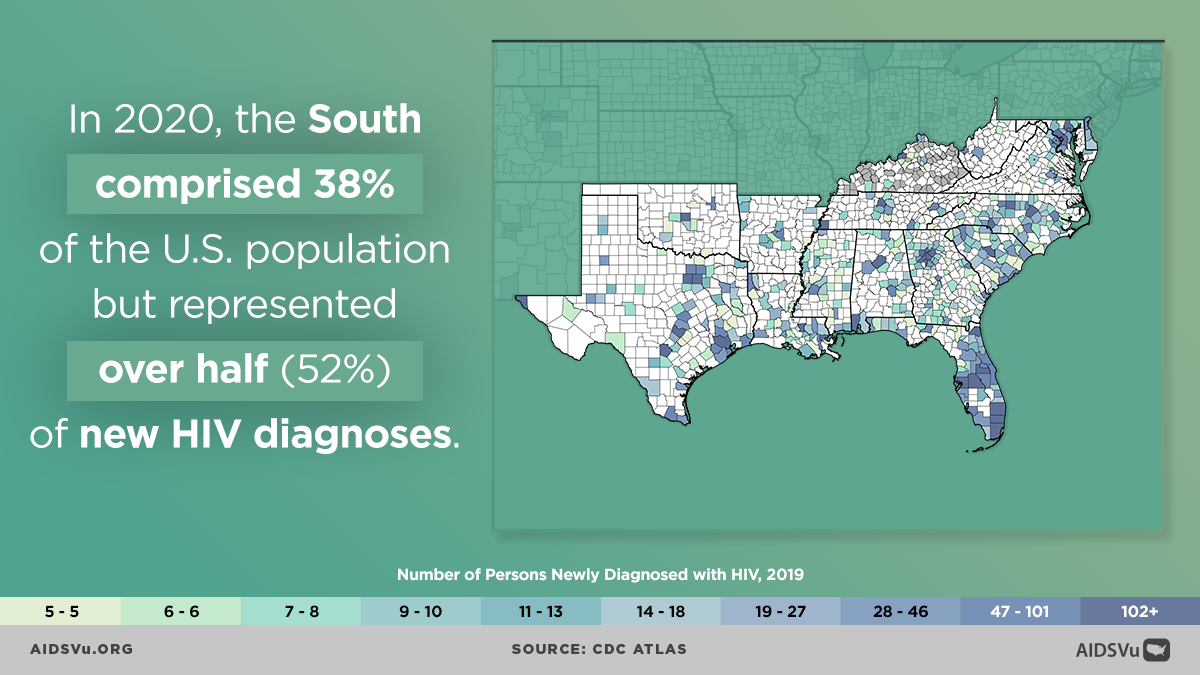
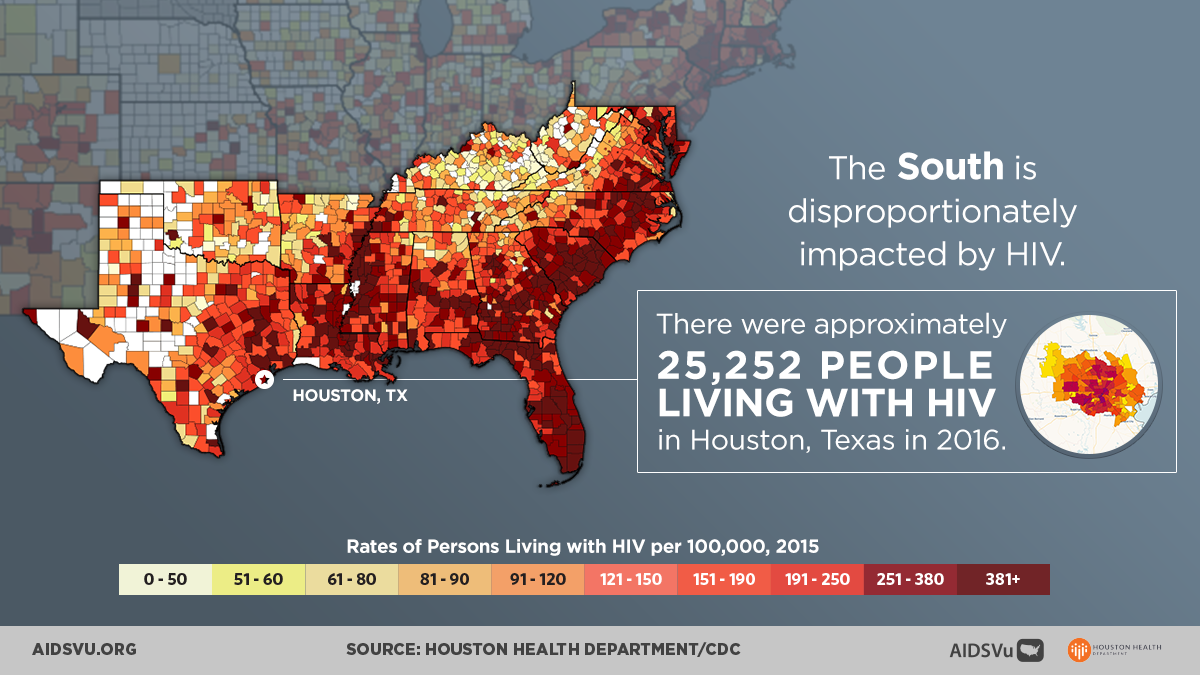
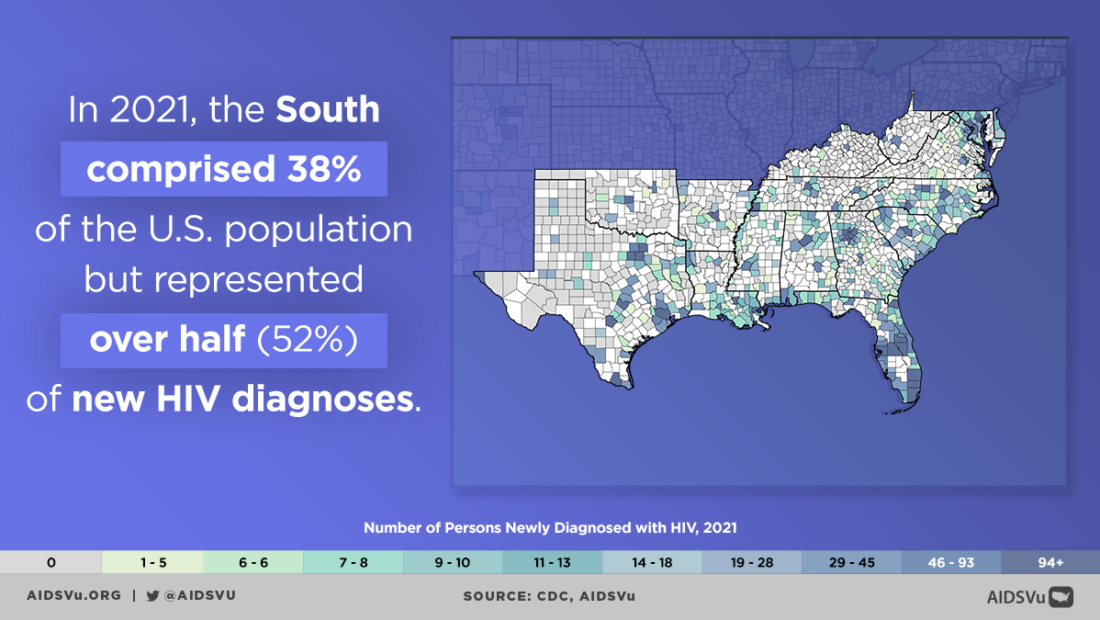
The Southern U.S. accounts for approximately 38% of the U.S. population but represented more than half (52%) of all new HIV diagnoses in 2022.
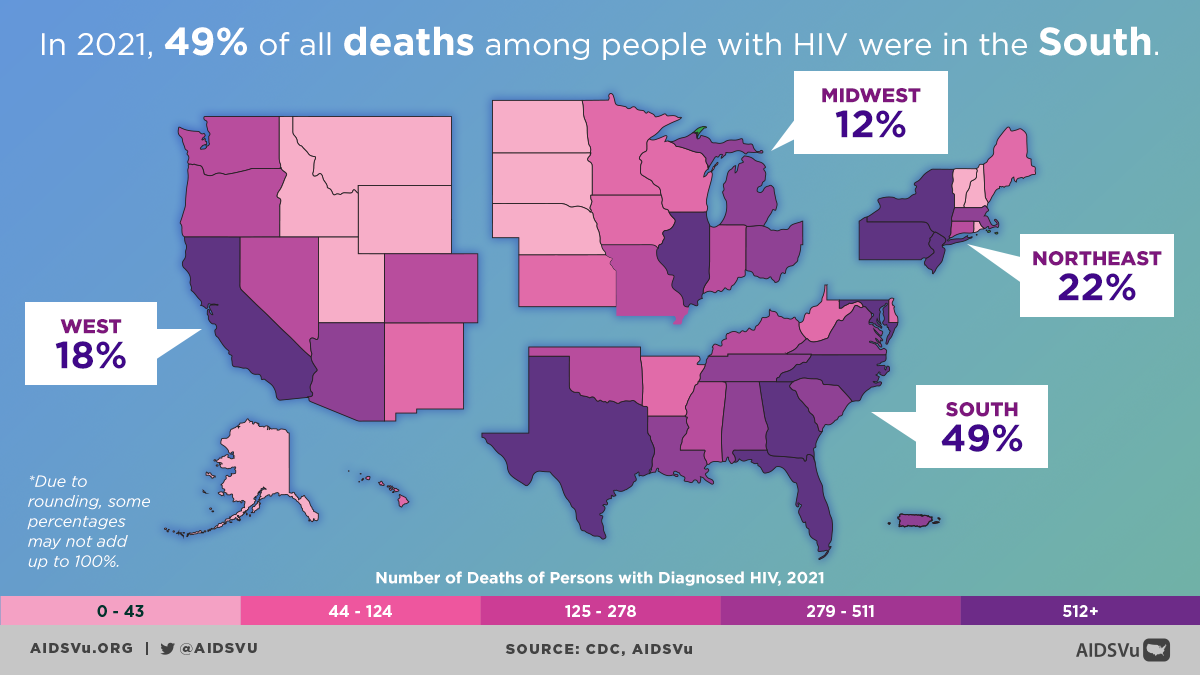
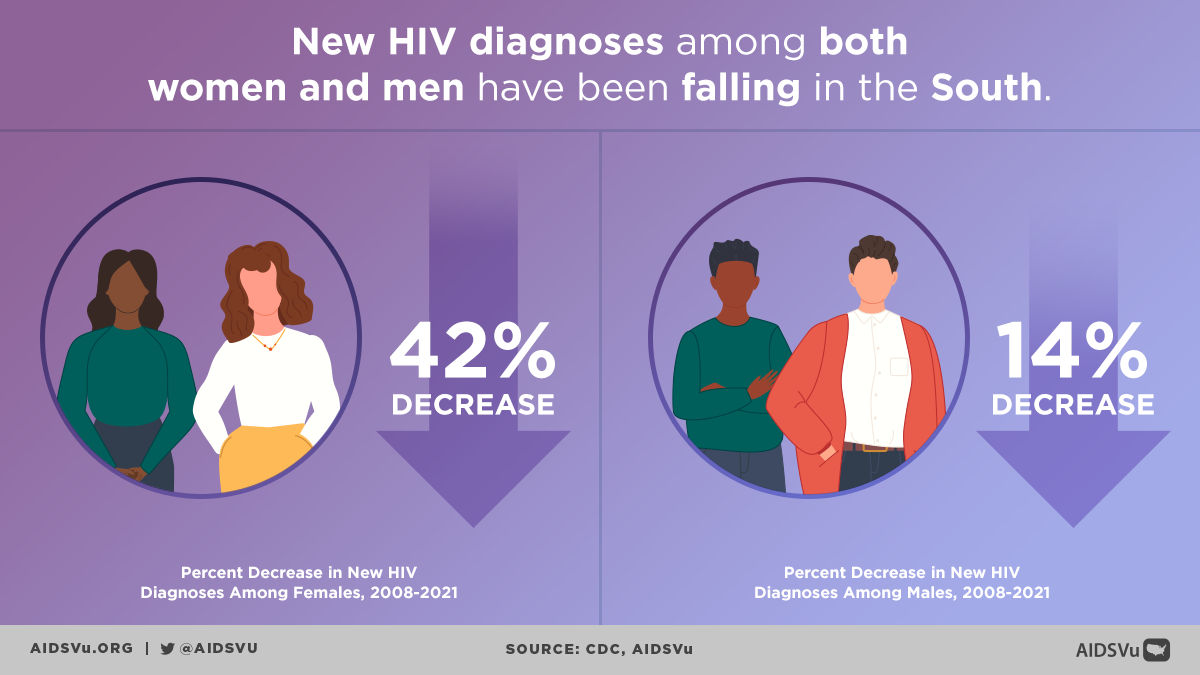
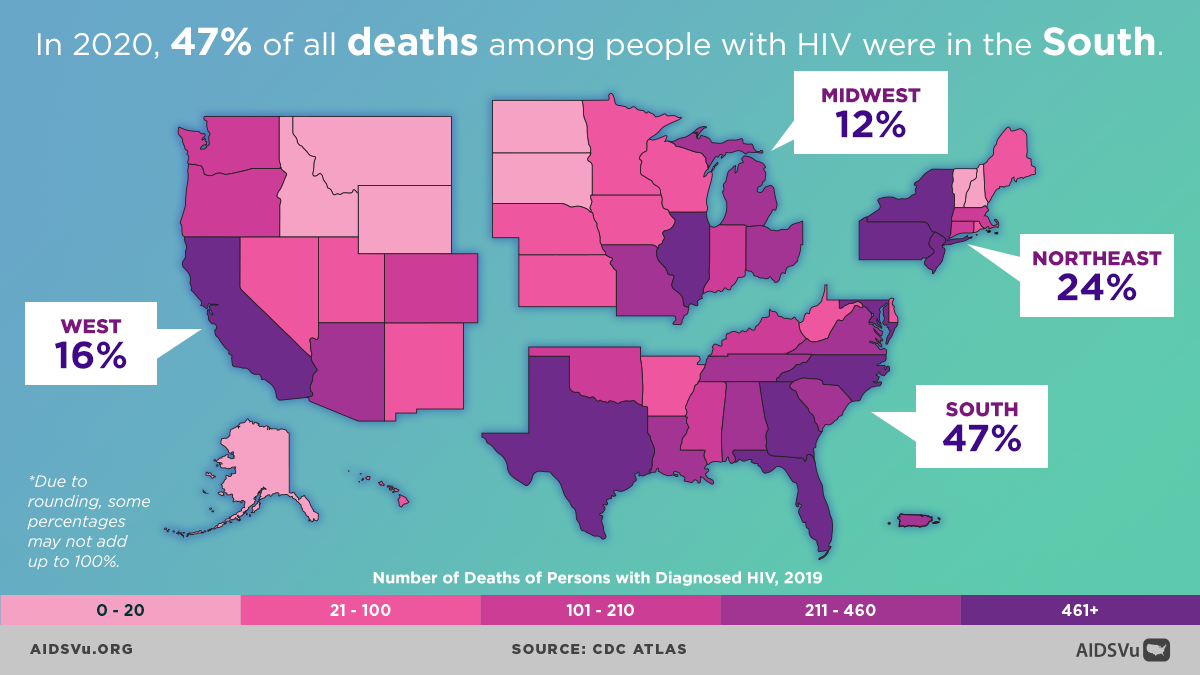
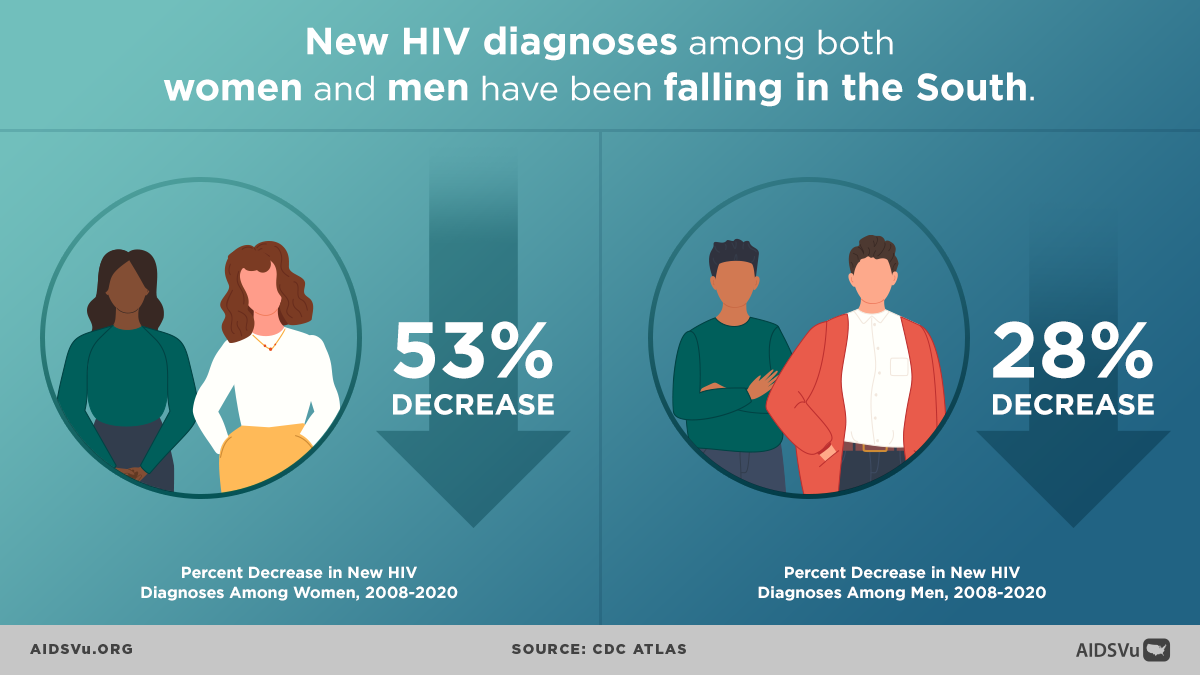
Despite significant advances in diagnosis, care, and prevention, HIV/AIDS continues to be a public health crisis in the United States. The situation is most acute in the Southern U.S., which experiences the greatest burden of new HIV infection, illness, and deaths of any U.S. region.
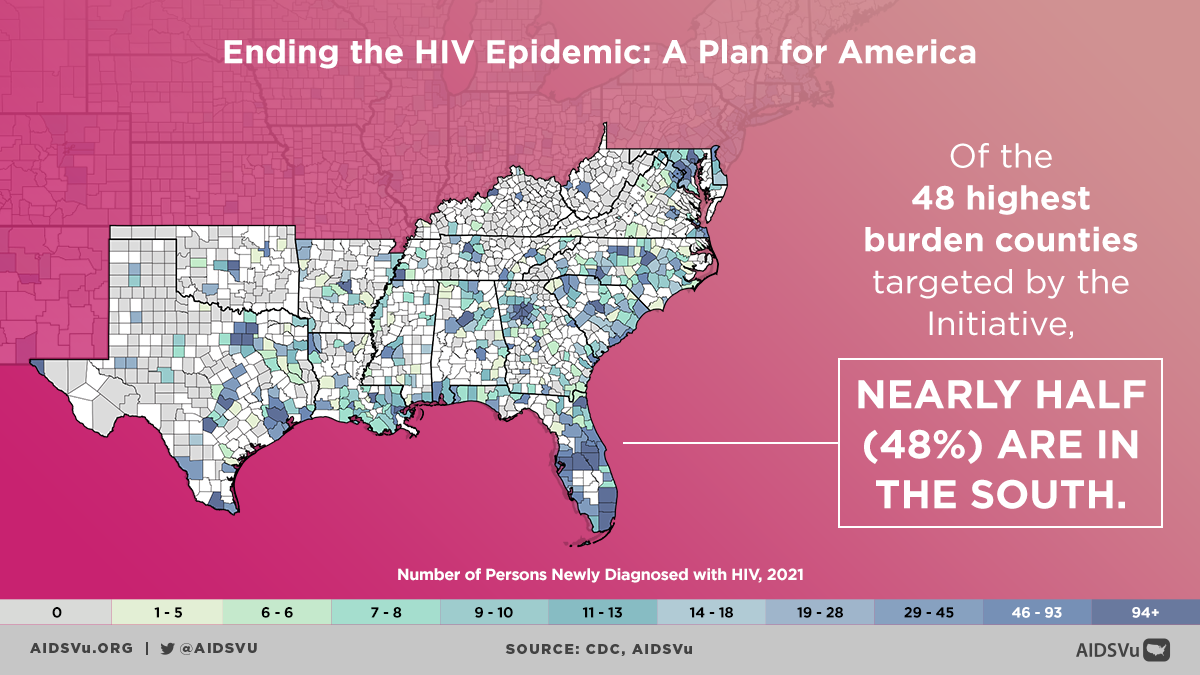
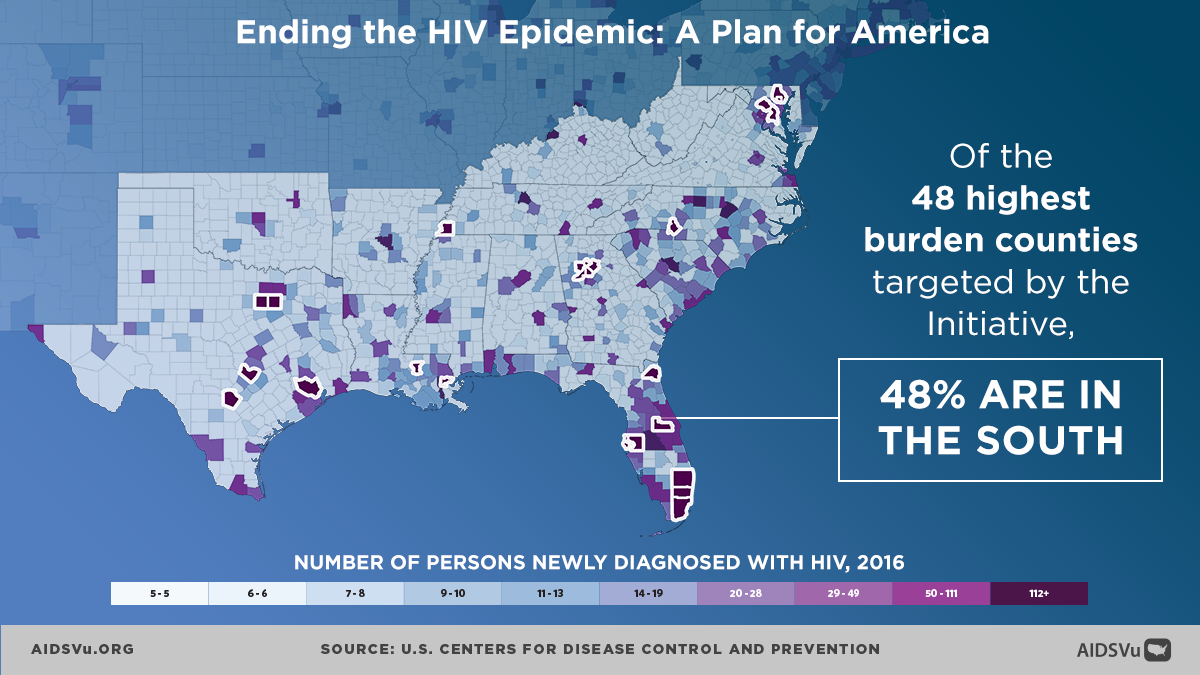
In early 2019, President Trump introduced the Ending the HIV Epidemic: A Plan for America initiative, which seeks to end HIV in the United States by 2030. Funding was distributed to 48 counties with the highest burden of new HIV diagnoses along with San Juan, Puerto Rico and Washington, D.C. and seven states (Alabama, Arkansas, Kentucky, Mississippi, Missouri, Oklahoma, and South Carolina) with a substantial rural HIV burden.
Of the 48 highest burden counties targeted by the Initiative, 48% are in the South.
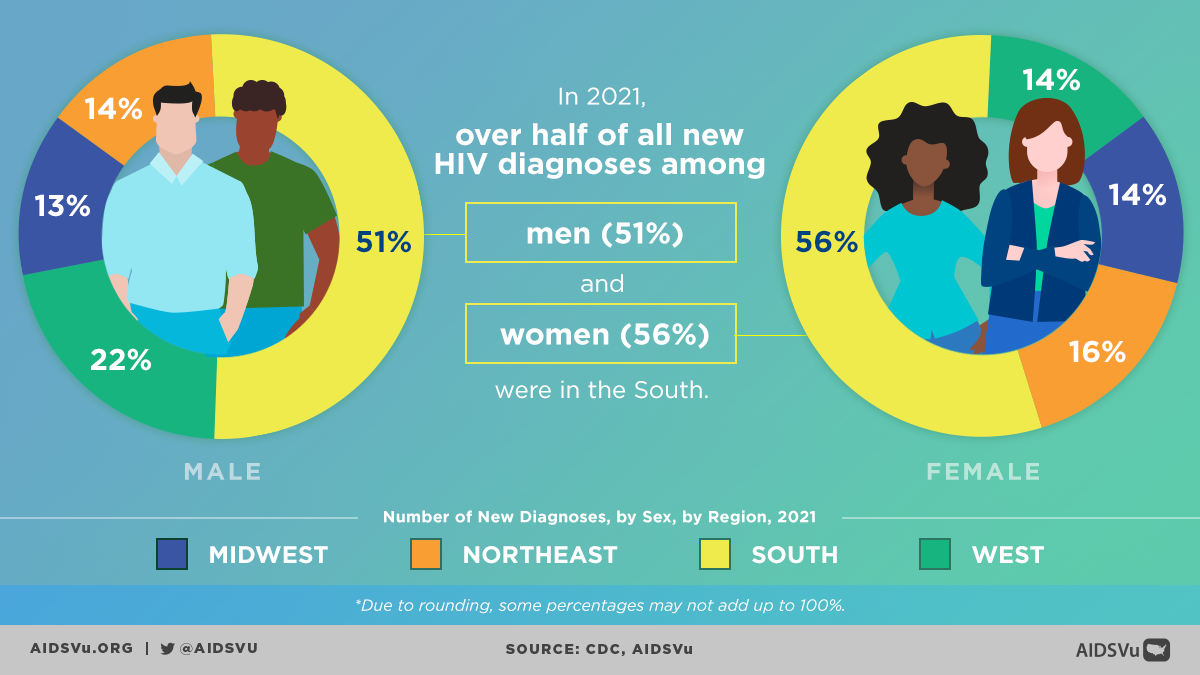
The Southern U.S. accounts for approximately 45% of all people living with an HIV diagnosis in the U.S. and over half of all new HIV diagnoses in 2021. This is despite the region only making up one-third (38%) of the U.S. population.
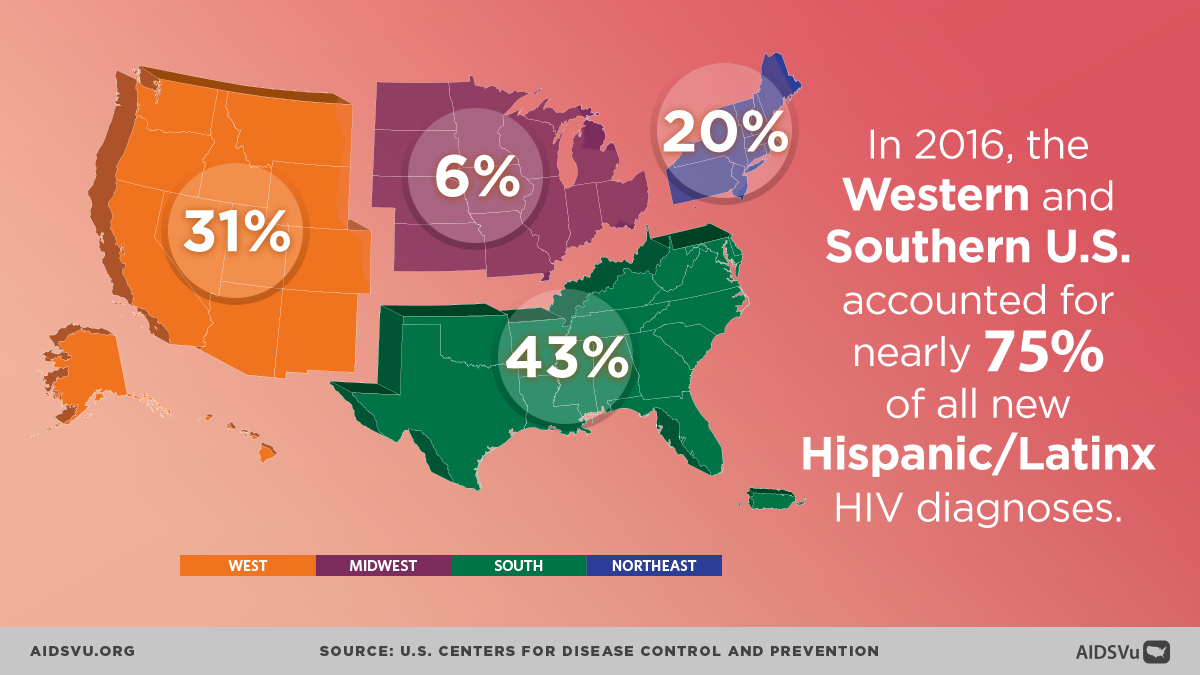
However, some communities in the South, such as Black and Latino gay and bisexual men, are disproportionately impacted by HIV and are seeing increased rates of new infection – a chilling reminder that the HIV epidemic is far from a thing of the past.
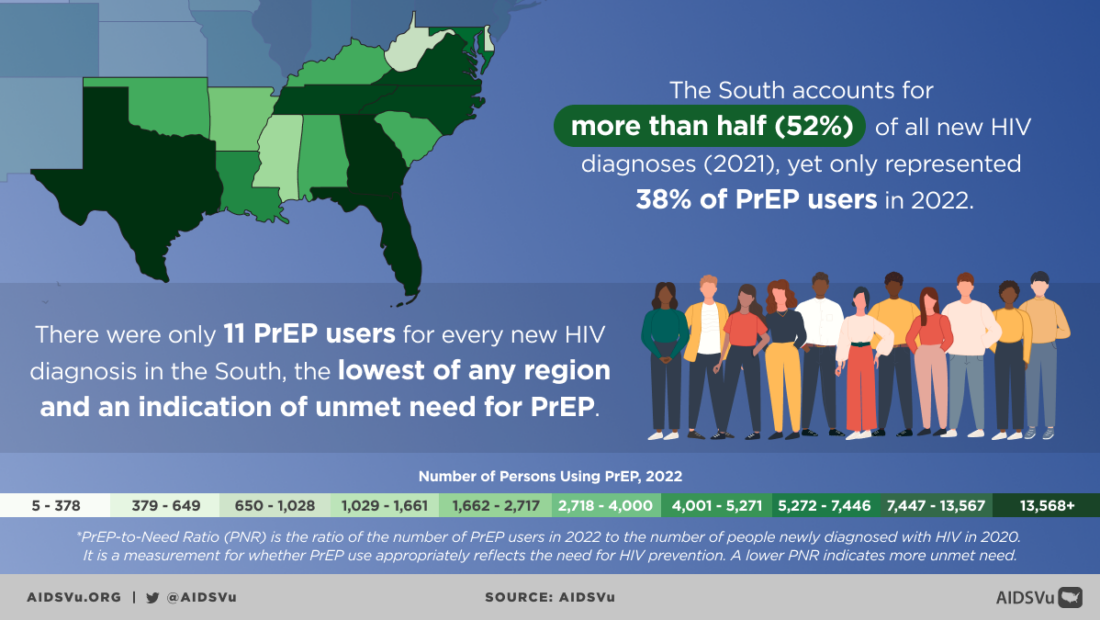
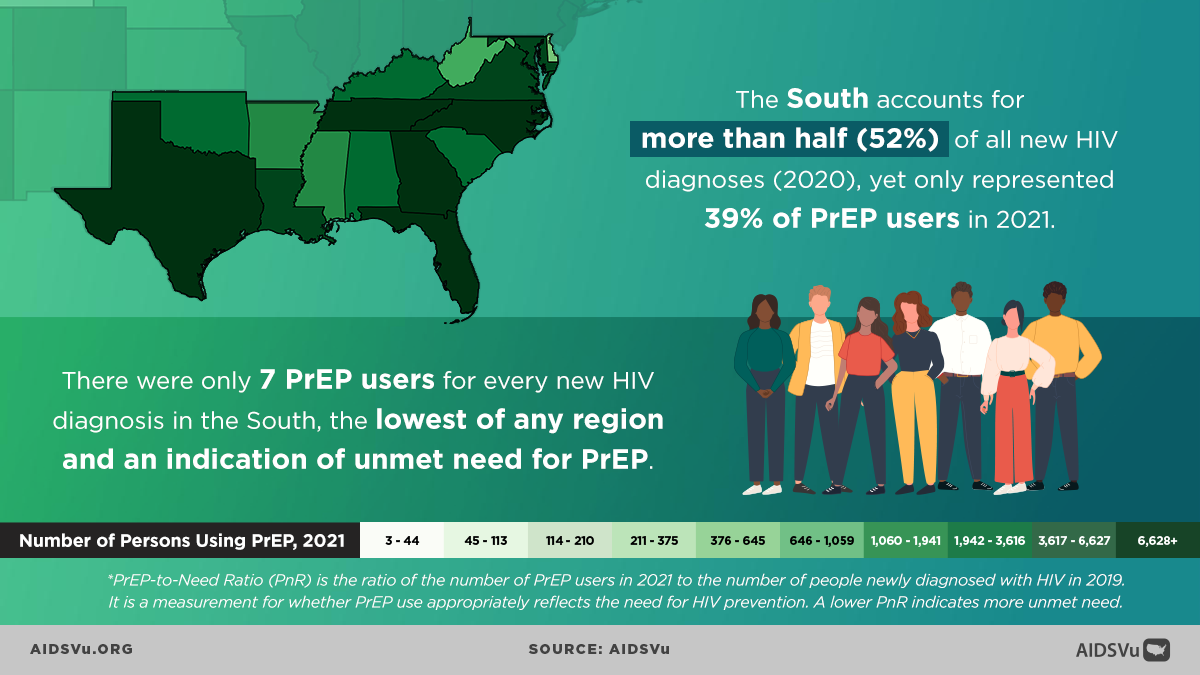
PrEP Use in the South
As of 2022, the South accounted for over half of new HIV diagnoses but only accounted for 38% of PrEP users in 2023. Black people made up 48% of new HIV diagnoses in the South, but only 21% of PrEP users in the South.
Of the 5 states with the greatest unmet need for PrEP, all 5 were in the Southern region of the United States (West Virginia, Alabama, Puerto Rico, Mississippi, South Carolina).
* PrEP-to-Need Ratio (PNR) is the ratio of the number of PrEP users in 2022 to the number of people newly diagnosed with HIV in 2020. It is a measurement for whether PrEP use appropriately reflects the need for HIV prevention. A lower PNR indicates more unmet need.
5 Ways to Use AIDSVu
Explore Maps
Explore the interactive map, customize your view, and easily print for presentations, grant applications, or other materials.
Learn MoreView Local Statistics
View local statistics for your city or state, and download high-impact data visualizations for your work
Learn MoreDownload Data
Download the datasets that inform AIDSVu’s visualizations for your own research and analysis
Learn MoreLocate Services
Visit our service locators to find and share HIV prevention, testing, and Ryan White care services across the South. Our service locator also includes service location sites in the Deep South for stigma reduction, overdose prevention/reversal, harm reduction, and trauma-informed care.
Learn MoreInteractive Maps
Explore AIDSVu’s interactive maps that visualize HIV prevalence, new diagnoses and mortality in the Southern U.S. Filter by race/ethnicity, sex, age, and transmission category to see how HIV impacts certain groups.
Beyond the Map
AIDSVu offers tools and resources beyond the HIV map that provide users with a deeper understanding of the HIV epidemic, its socioeconomic-driving factors, and services available at the community level.
Social Determinants of Health
See how HIV prevalence is related to poverty, high school education, median household income, etc.
Learn MoreFind Services
Use the testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services locators to find critical HIV/AIDS services near you.
Learn MoreLocal Data
View city and state profiles with local HIV/AIDS statistics, national comparison charts, and local resources.
Learn MoreFor More Information
Learn more about the impact of HIV in the Southern U.S. with the following additional resources.