A Comprehensive Guide to Understanding HIV Care from Diagnosis to Viral Suppression
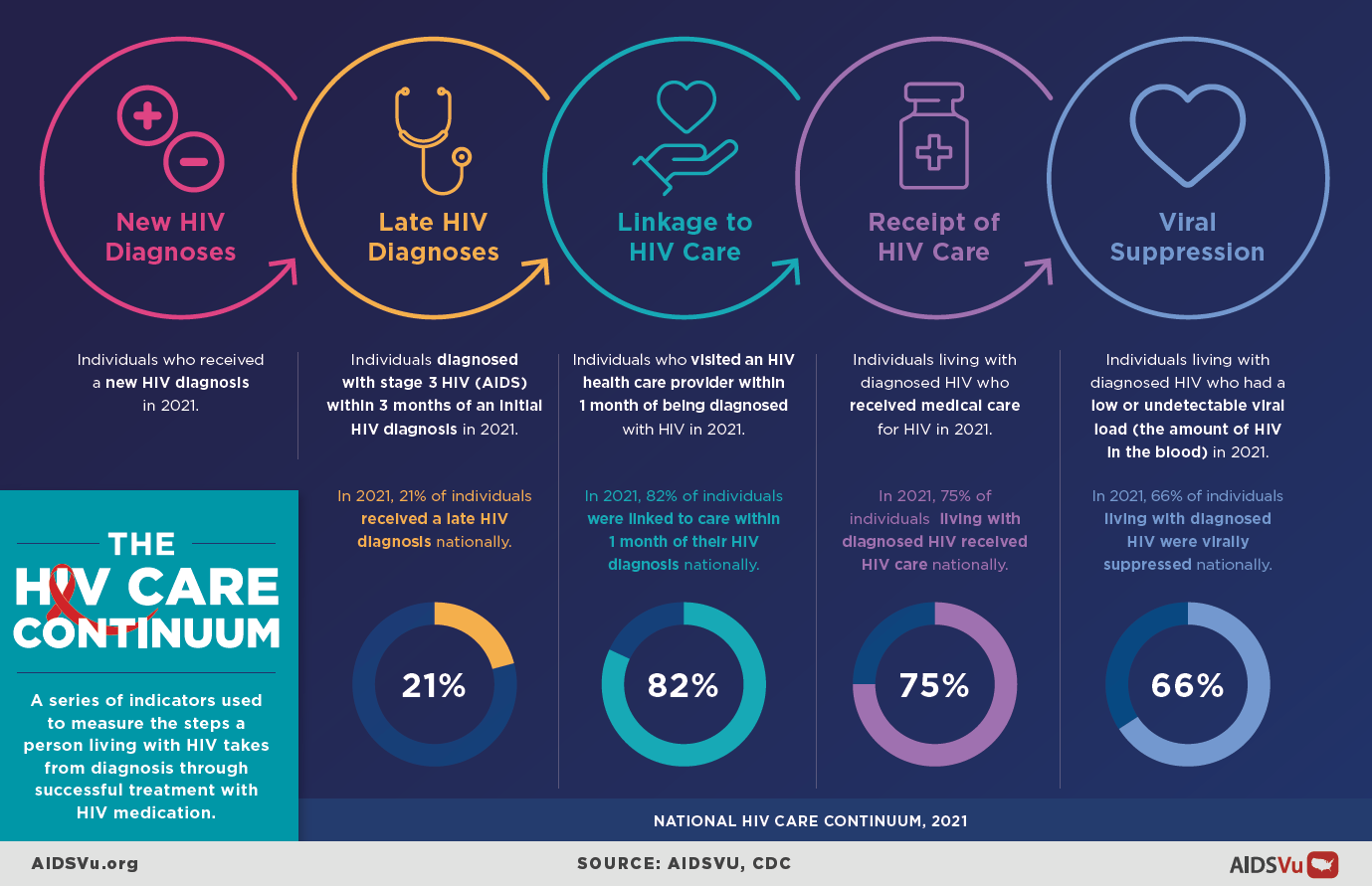
The HIV care continuum is a powerful public health framework that maps the essential journey people living with HIV take from initial diagnosis through achieving and maintaining viral suppression. This model serves as both a roadmap for individual care and a critical tool for assessing population-level progress toward ending the HIV epidemic. By understanding where people succeed and where they face barriers along this continuum, policymakers, healthcare providers, and communities can target resources and interventions where they’re needed most.
Understanding the HIV Care Continuum
The HIV care continuum outlines five sequential steps that guide comprehensive HIV care and treatment. Each step builds upon the previous one, creating a pathway that ultimately leads to optimal health outcomes and prevention benefits. Success at each stage is measured through specific indicators that help track both individual progress and community-wide achievements.
The ultimate goal: Help every person living with HIV achieve and maintain viral suppression, which not only preserves their health but also eliminates the risk of sexual HIV transmission to others.
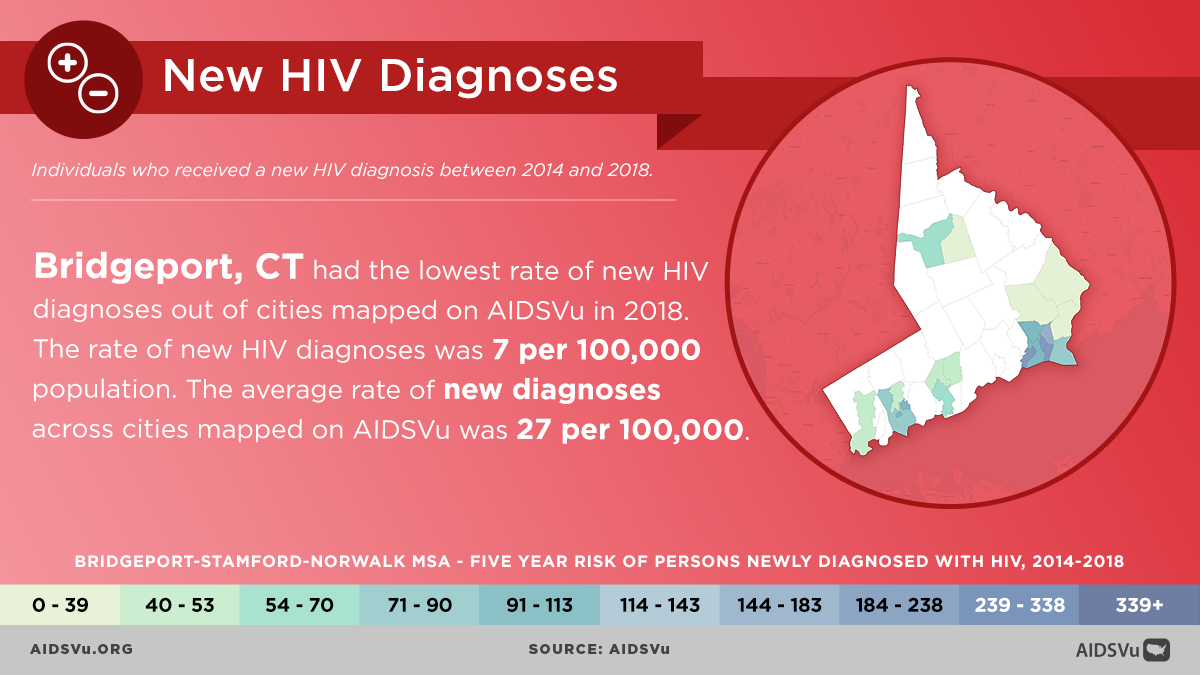
Step 1: HIV Diagnosis
Definition: Receiving a positive HIV test confirmed by a healthcare provider and becoming aware of one’s HIV status.
Why This Step Matters
Early diagnosis is the gateway to all HIV care and treatment. According to CDC data, 87% of people living with HIV in the United States knew their HIV status in 2024, but significant gaps remain. People who don’t know their status cannot access treatment, and a CDC analysis shows that nearly 80% of new HIV infections in the U.S. in 2016 came from the nearly 40% of people who either did not know they had HIV or who received a diagnosis but were not receiving HIV care and treatment.
Current Statistics from AIDSVu Data
- National Progress: The U.S. has made substantial improvements in HIV testing and diagnosis over recent years
- Geographic Variations: Most HIV cases occur in metropolitan areas with 500,000 or more people. The South has the highest number of people with HIV, but if population size is taken into account, the Northeast has the highest rate of people with HIV
- Demographic Disparities: Testing rates and diagnosis timing vary significantly across racial, ethnic, age, and risk groups
Barriers to Diagnosis
- Stigma surrounding HIV testing
- Limited access to healthcare services
- Lack of awareness about HIV risk
- Fear of discrimination
- Geographic barriers in rural areas
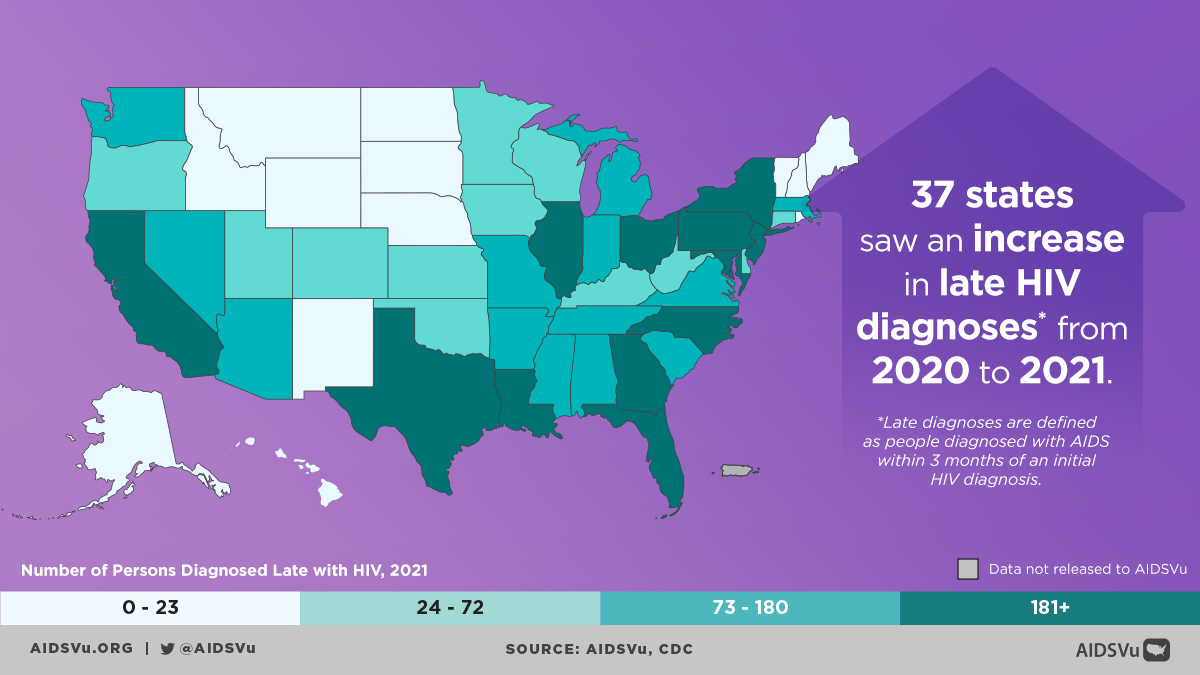
Step 2: Late HIV Diagnosis
Definition: Individuals diagnosed with stage 3 HIV (AIDS) within three months of an initial HIV diagnosis.
The Challenge of Late Diagnosis
Late diagnosis represents a critical missed opportunity for early intervention. When people receive their HIV diagnosis after the virus has already progressed to AIDS, they face more complex health challenges and have had more opportunities to unknowingly transmit the virus.
Key Statistics
According to a 2024 CDC report, 33% of people aged 55 to 64 in the U.S. who received a new HIV diagnosis in 2022 already had late-stage HIV infection (AIDS) when they were diagnosed, indicating a need for routinized HIV screening in this population.
Impact on Communities
- Higher healthcare costs due to advanced disease
- Increased mortality risk
- Greater transmission risk during undiagnosed period
- More complex treatment requirements
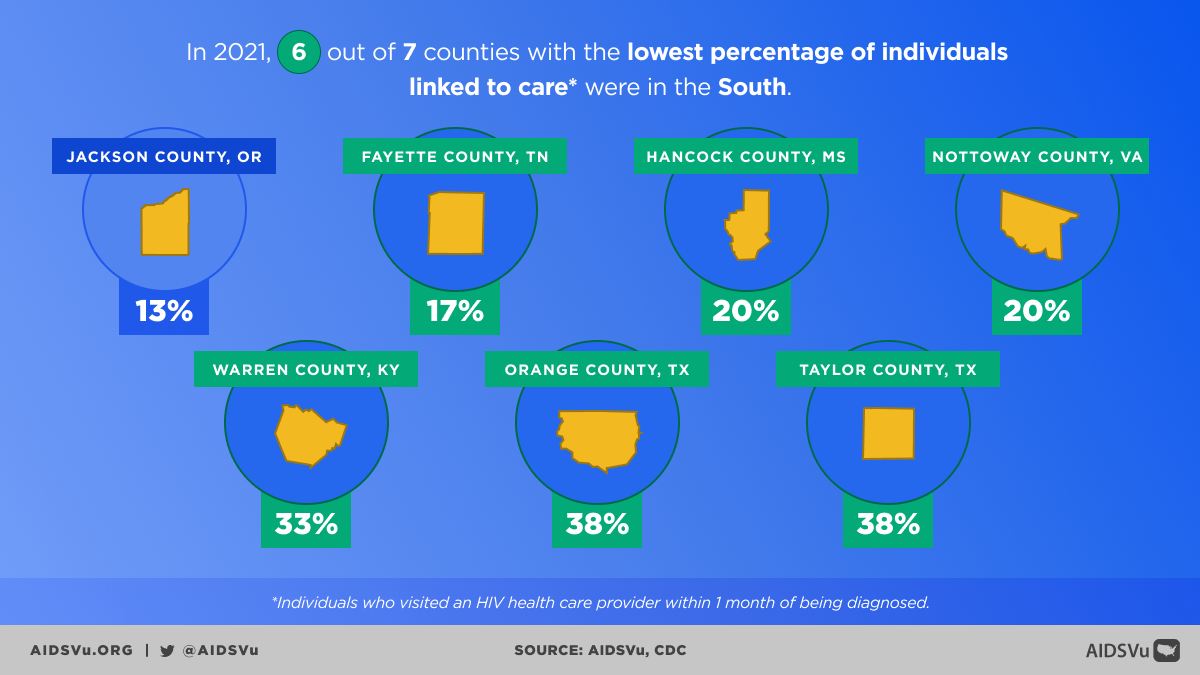
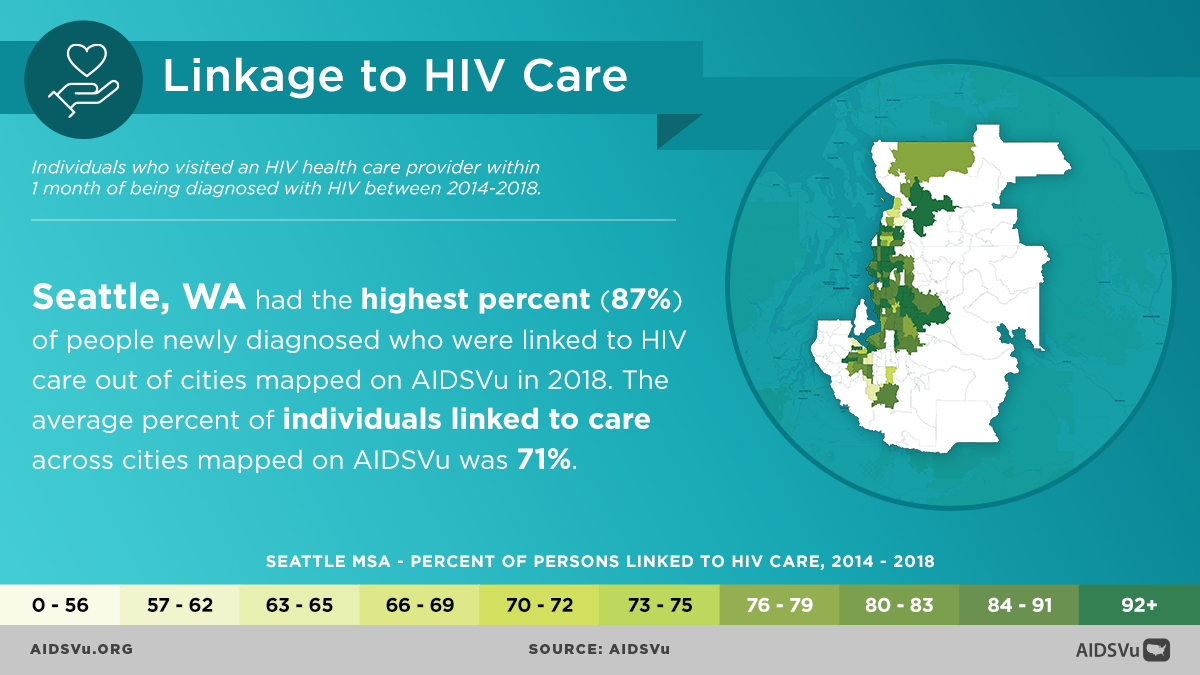
Step 3: Linkage to Care
Definition: Having at least one documented CD4 or viral load test within 30 days of HIV diagnosis.
The Critical First Month
The period immediately following HIV diagnosis is crucial. Research shows that people who are linked to care quickly are more likely to remain engaged in treatment and achieve viral suppression. The goal is to connect everyone who tests positive for HIV to medical care within one month of their diagnosis.
Current Performance
Among persons who received diagnoses of HIV infection during 2022, 82% were linked to care within one month of diagnosis. Asian persons had the highest percentage of linkage to care within one month (88%), and Native Hawaiian/other Pacific Islander persons (74%), American Indian/Alaska Native persons (78%), Black persons (78%), and women (80%) had the lowest percentages.
Factors Affecting Linkage
- Healthcare Access: Insurance coverage, proximity to HIV specialty care
- Social Support: Family acceptance, peer support networks
- System Factors: Care coordination, navigator programs
- Individual Factors: Mental health, substance use, competing priorities
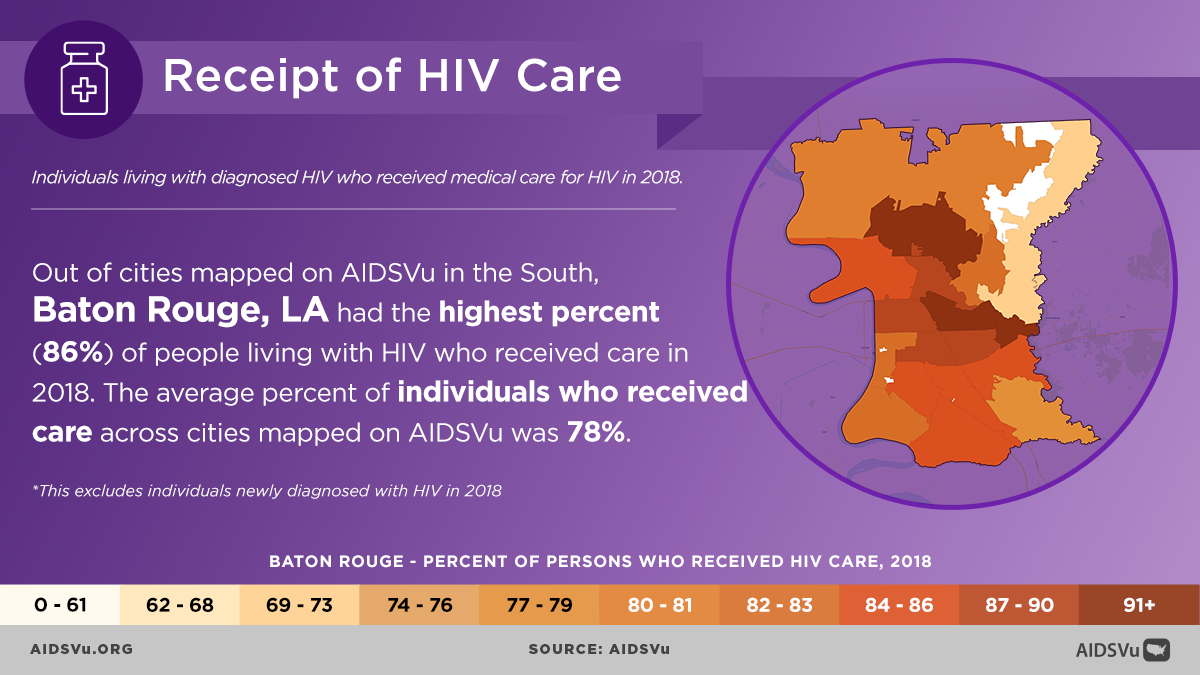
Step 4: Receipt of Care
Definition: Having had at least one CD4 or viral load test performed by a healthcare professional, demonstrating ongoing engagement with HIV medical care.
Sustained Engagement Challenges
While initial linkage to care is important, sustained engagement presents ongoing challenges. According to CDC data, for every 100 people with diagnosed HIV in 2022, about 76% received some HIV care, 54% were retained in care, and 65% were virally suppressed.
Supporting Retention in Care
- Comprehensive Services: Integrating HIV care with other health services
- Patient-Centered Approach: Flexible scheduling, cultural competency
- Address Social Determinants: Some challenges with achieving and maintaining viral suppression include HIV stigma, physical health, mental health, and structural issues—such as food insecurity, unemployment, and unstable housing or homelessness
- Technology Integration: Telemedicine, mobile health applications
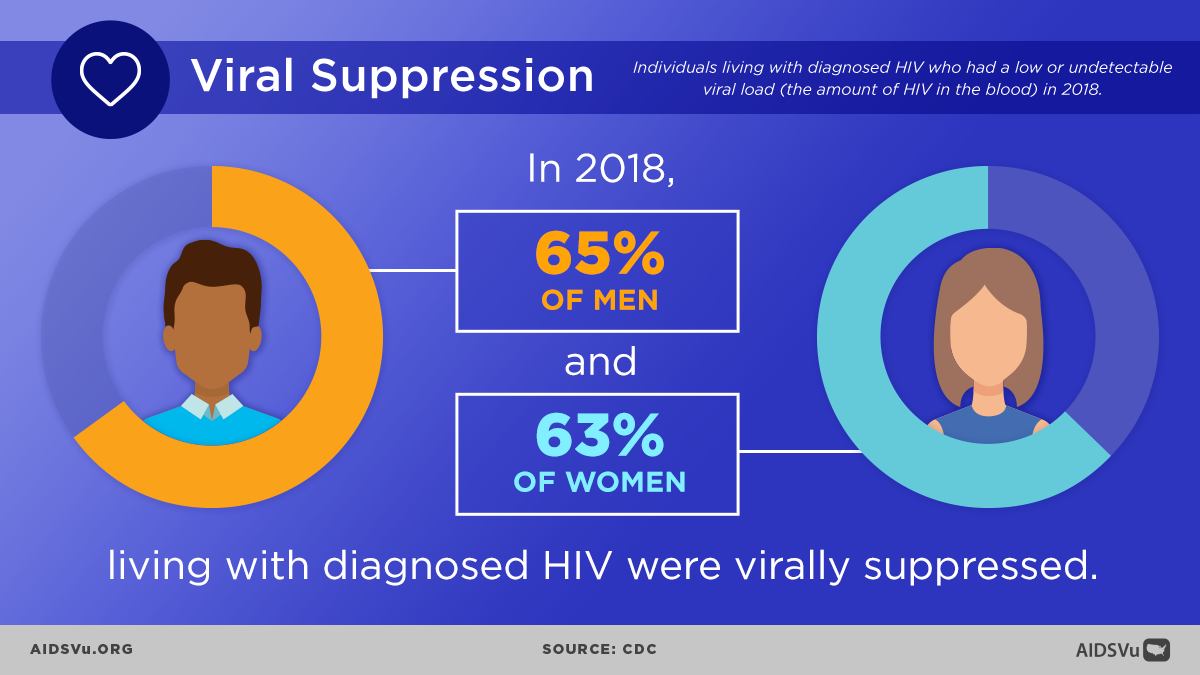
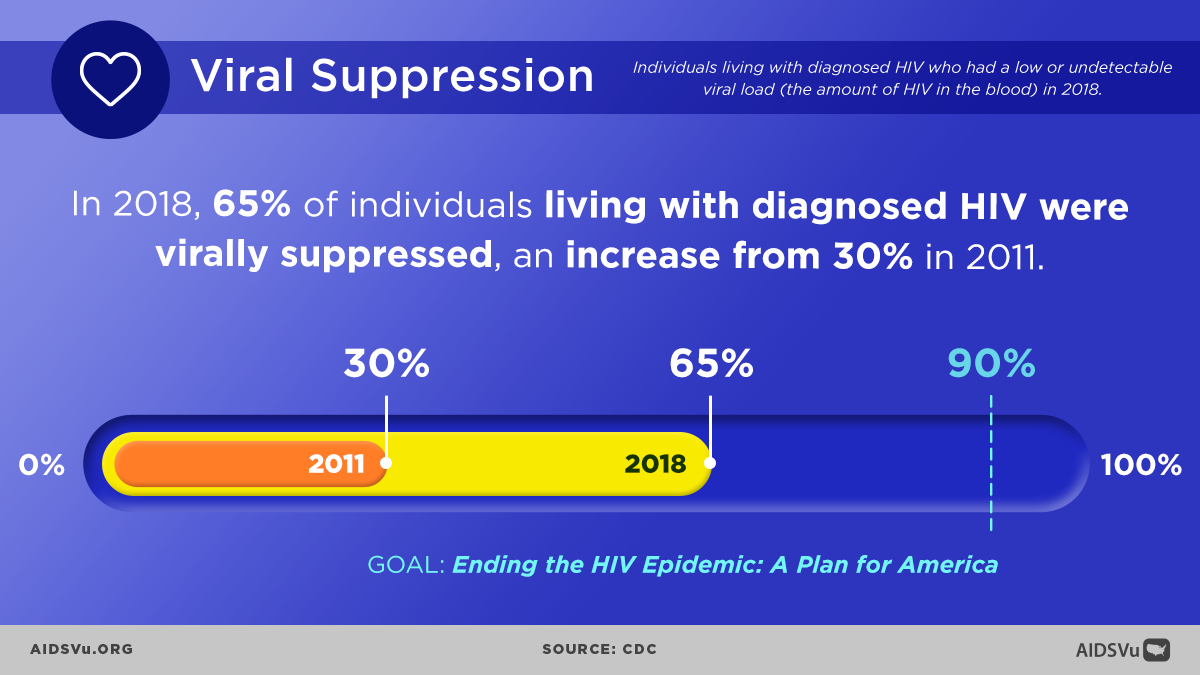
Step 5: Viral Suppression
Definition: Having a viral load test result of less than 200 copies/mL at the most recent test.
The Ultimate Goal
Viral suppression represents the pinnacle of HIV care success. When achieved and maintained, it provides tremendous benefits for both individual health and public health prevention efforts.
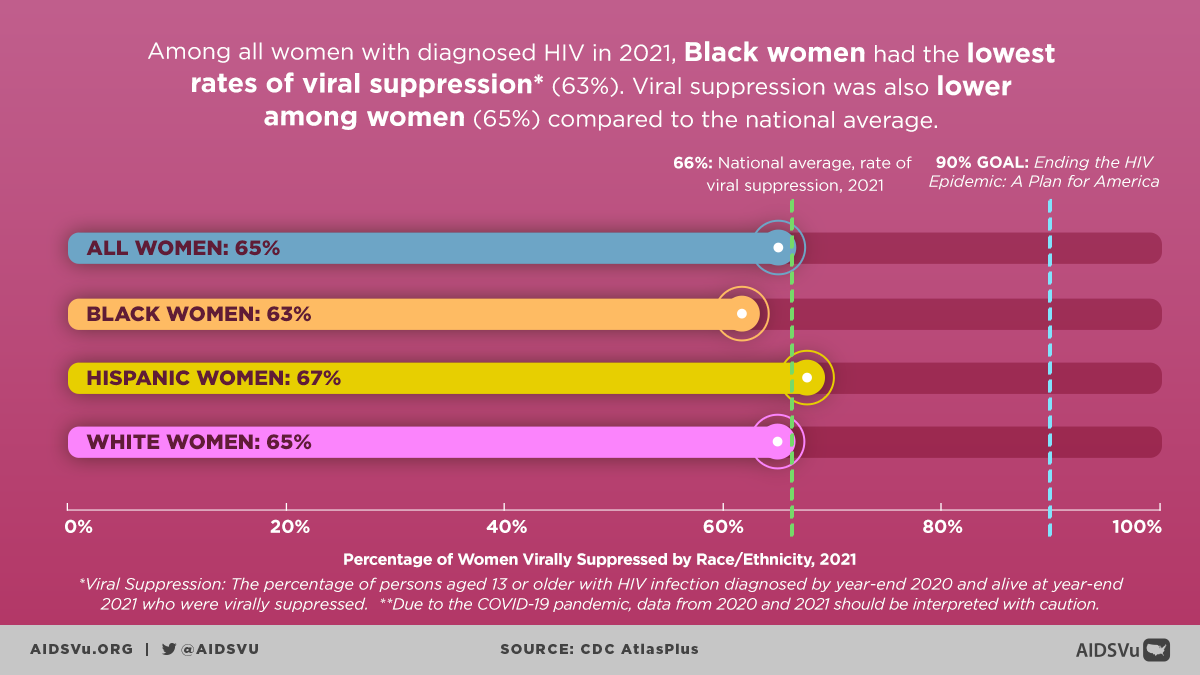
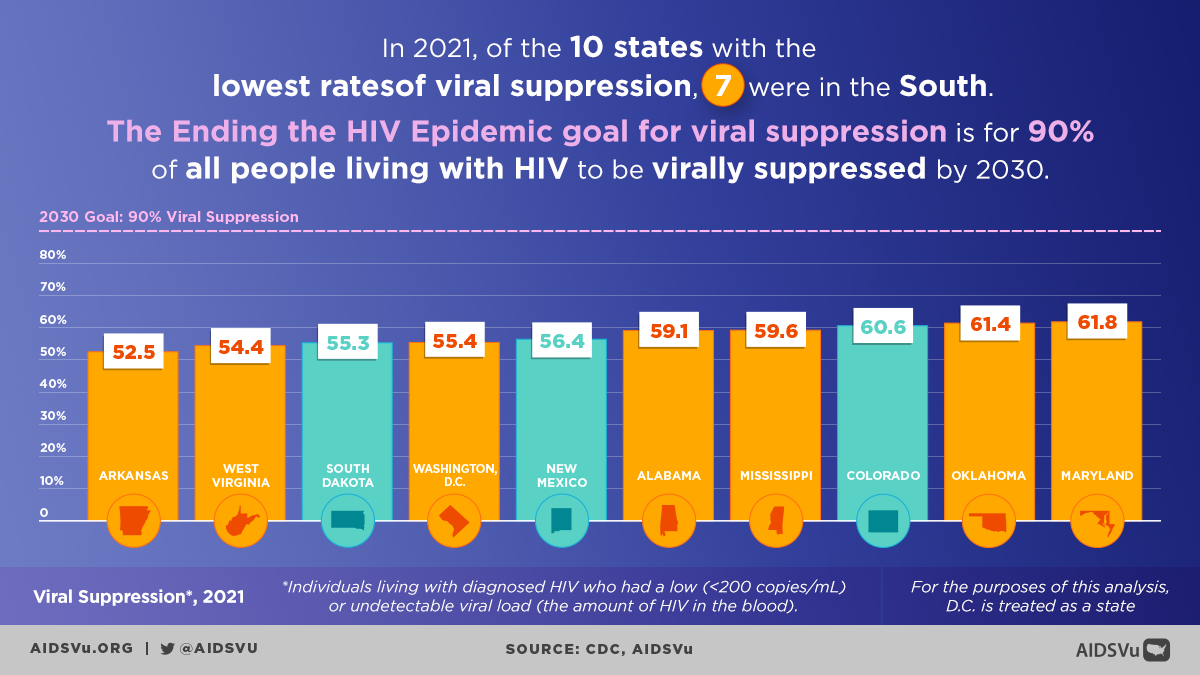
Current National Statistics
Among persons with diagnosed HIV and alive at year-end 2022, 65% were virally suppressed at the most recent viral load test. The lowest percentages of viral suppression were among Black persons (61%) and women overall (64%).
The U=U Revolution
Undetectable = Untransmittable (U = U), which means that once an individual is virally suppressed to the point where HIV cannot be detected in their blood, they effectively have no risk of sexually transmitting HIV to HIV-negative partners.
Addressing Disparities Across the Continuum
Racial and Ethnic Disparities
AIDSVu data consistently reveals significant disparities across racial and ethnic groups at each step of the continuum. These disparities reflect broader social and economic inequities that impact healthcare access and outcomes.
Geographic Variations
AIDSVu’s continuum maps allow viewers to look at city-level HIV surveillance data by race/ethnicity, sex, and age. In Fulton County (one of the two counties that make up metro Atlanta), approximately 60% of individuals living with HIV are virally suppressed.
Age-Related Challenges
People aged 55 to 64 accounted for 8% of the 37,966 new HIV diagnoses in 2022, and older adults face unique challenges including higher rates of late diagnosis and specific health complications.
The HIV Status-Neutral Approach
Expanding the Framework
There is also a growing movement among those working in HIV for a new kind of continuum that can be applied to everyone regardless of their HIV status. The New York City Department of Health and Mental Hygiene (NYC DOHMH) has been a leader in proposing this type of paradigm, which it refers to as the HIV Status Neutral Prevention and Treatment Cycle.
How It Works
- For HIV-Positive Individuals: Enter the traditional HIV care continuum immediately
- For HIV-Negative Individuals: Move into prevention services including PrEP evaluation
- Continuous Engagement: Regular testing and prevention services for all individuals
Benefits of Status-Neutral Care
- Reduces HIV-related stigma
- Normalizes HIV testing and prevention
- Creates comprehensive prevention and care systems
- Recognizes that HIV care and prevention are lifelong processes
5 Ways to Use AIDSVu
View Local Statistics
National-, state-, county- and city-level profiles with HIV care continuum statistics.
Learn MoreExplore Maps
Interactive maps on each step of the HIV care continuum at the state- and ZIP Code-level.
Learn MoreShare Infographics
Infographics on each step of the HIV care continuum, as well as a set of infographics on viral suppression.
Learn MoreExpert Blogs
Stay up to date with the latest Q&As from experts on the HIV care continuum.
Learn MoreContinuum City Profiles
Explore AIDSVu’s profiles of states and cities with HIV care continuum data by clicking the city dots or states below. To explore HIV continuum data for the 48 counties prioritized for Phase 1 of Ending the HIV Epidemic: A Plan for America, a ten-year initiative to end the HIV epidemic in the U.S., visit our county-level profiles.
Percent of Persons Virally Suppressed, 2021
For More Information
Learn more about the HIV care continuum with these resources.
HRSA
The Health Resources and Services Administration is an agency of the U.S. Department of Health and Human Services and is the primary federal agency for improving access to health care services for people who are uninsured, isolated or medically vulnerable.
Learn MoreCDC
CDC provides leadership for HIV prevention research and surveillance and the development and testing of effective biomedical interventions to reduce the rate of HIV infection in the U.S.
Learn MoreNASTAD
NASTAD is a leading non-partisan non-profit association that represents public health officials who administer HIV and hepatitis programs in the U.S. and around the world.
Learn MoreUNAIDS
The Joint United Nations Programme on HIV and AIDS is the main advocate for accelerated, comprehensive and coordinated global action on the HIV/AIDS pandemic.
Learn More