To continue progress toward ending the HIV epidemic, Congress annually appropriates funds to Departments and agencies across the federal government that are designated to address HIV prevention, care, treatment, and research priorities. Federal HIV funding supports essential programs, and funds work in every state across the U.S. to prevent new infections, provide access to vital treatment and prevention medicines, and ultimately save lives.
There have been encouraging trends in the fight against HIV. According to the Centers for Disease Control and Prevention (CDC), between 1984 and 2022, the number of new HIV infections (both diagnosed and undiagnosed) decreased by an estimated 76%. More recently, from 2010 to 2022, new infections declined by 19%. In 2022, an estimated 31,800 new HIV infections still occurred in the U.S. and not all populations experienced the same level of decline in infections.
These hard-earned gains could quickly be lost if funding for prevention and treatment programs is reduced or eliminated. A reduction in resources would undermine momentum to end the HIV epidemic, further hollow out an already understaffed workforce, and potentially lead to higher rates of new HIV diagnoses, and additional costs.
The O’Neill Institute notes that in 2022, there were 6,700 fewer new cases of HIV than in 2017, the first year that President Trump was in office. Averting just that number of cases in one year alone saved the health system $2.8 billion in lifetime HIV treatment costs (Based on a 2021 analysis that updated the lifetime cost of treating a single person with HIV at just over more than $420,000, A. Bingham, et al, STD, 2021).
In their 2020 paper, “Estimation of the Incremental Cumulative Cost of HIV Compared with a Non-HIV Population,” Cohen et. al concluded that:
- Avoiding one new HIV infection can result in an average of $850,557 in lifetime healthcare cost savings.
- Average annual and cumulative healthcare costs were up to seven times higher for people living with HIV compared to those without HIV.
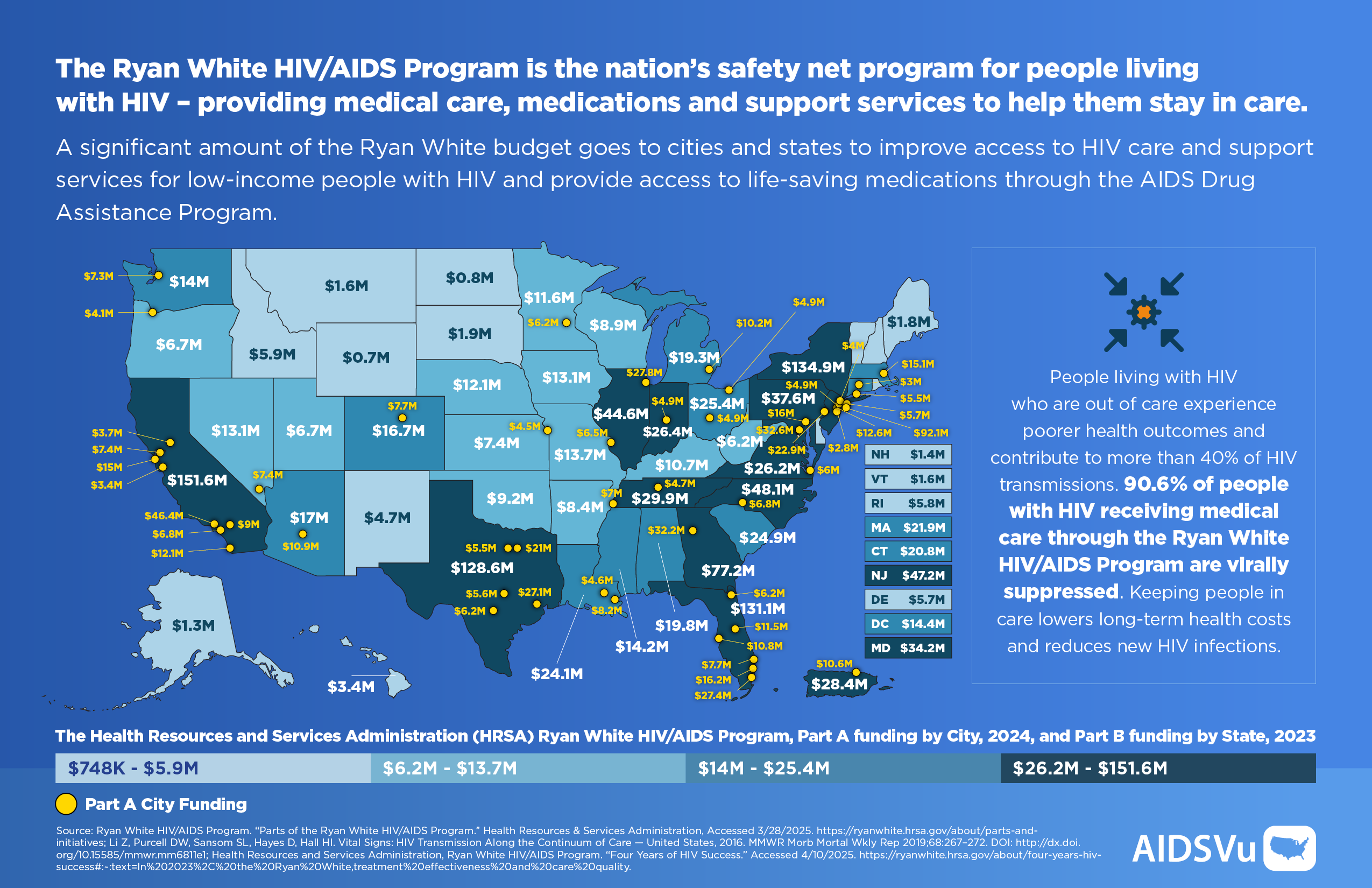
Federal HIV funding directly impacts all 50 states. Federal HIV funding makes up a significant portion of state health department budgets, especially in states like Georgia, Texas, Florida, North Carolina, Illinois, and Ohio that are disproportionately impacted by HIV.
Funded Agencies and Departments:
The U.S. Department of Health and Human Services (HHS) is the largest federal grant-making agency in the United States. The agencies and offices within HHS provide grant support for HIV prevention, testing, care and treatment, and research.
- Congress funds domestic discretionary spending on HIV services and research including funding to the CDC, The Health Resources and Services Administration (HRSA) Ryan White HIV/AIDS Program, HRSA Health Centers Program, The National Institutes of Health (NIH) – AIDS research, Substance Abuse and Mental Health Services Administration (SAMHSA) HHS Minority HIV/AIDS Fund, and Housing Opportunities for Persons With AIDS (HOPWA).
- Additionally, mandatory spending programs support HIV services including Medicaid, Medicare, Social Security Disability Insurance (SSDI), Supplemental Security Income (SSI), and others.
- A comprehensive response to HIV also addresses the set of linked health conditions, including viral hepatitis, sexually transmitted infections (STIs), and alcohol and substance use and mental health disorders that are part of a syndemic. Federal agencies involved in funding work related to these syndemic conditions include:
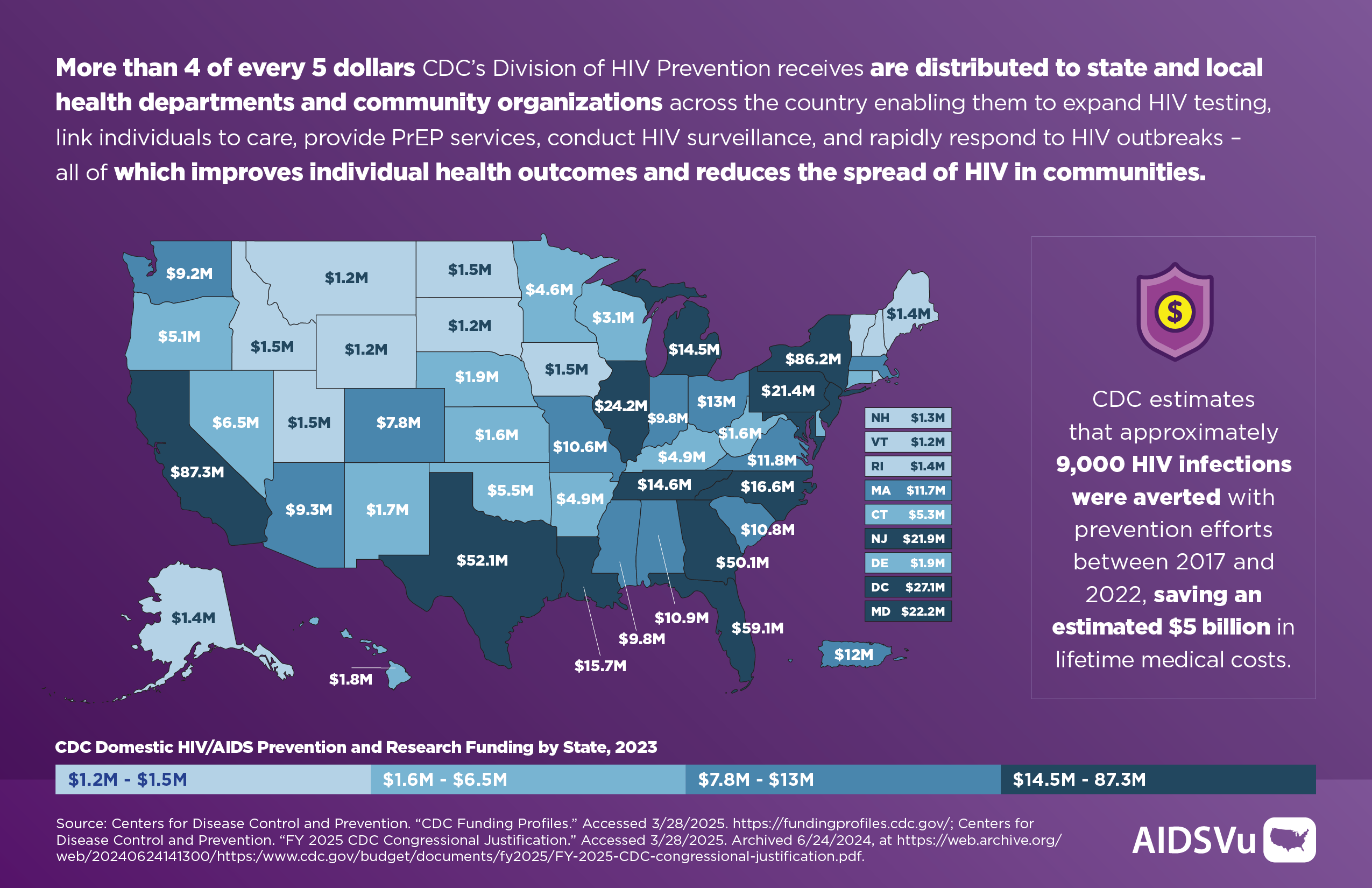
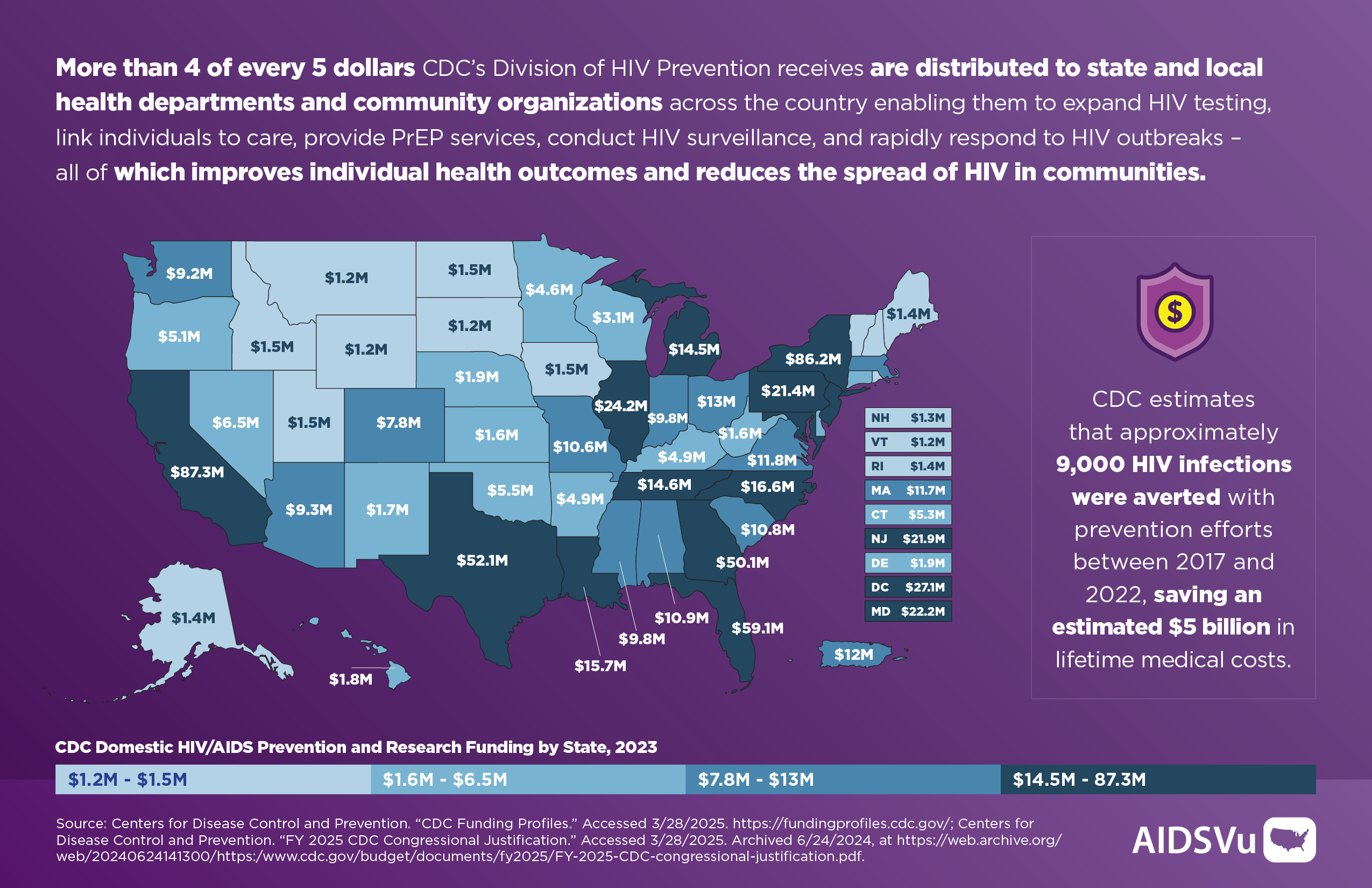
CDC Division of HIV Prevention
CDC’s Division of HIV Prevention supports national, state, and community-based high impact HIV prevention activities to prevent new HIV infections, improve health outcomes for persons with HIV, and reduce HIV-related disparities and health inequities. They collaborate with community, state, and national leaders to support the public, especially groups at higher risk of HIV infection, illness, and death. CDC has unique and important roles in conducting HIV surveillance, developing guidelines, educating providers and consumers, and assisting health departments with outbreak response.
CDC is the primary source of federal funding for HIV prevention in the U.S. and was the very first government agency funded to address the emerging HIV epidemic in the early 1980s. While CDC is the cornerstone of domestic HIV prevention efforts, representing 91% of all federal funding for HIV prevention, prevention funding represents a small share (3% in FY 2022) of what the federal government spends on HIV and a minuscule share of the federal budget overall. The FY24 appropriation for HIV prevention at the CDC totaled about $1 billion.
CDC estimates that approximately 9,000 HIV infections were averted with prevention efforts between 2017 and 2022, saving an estimated $5 billion in lifetime medical costs.
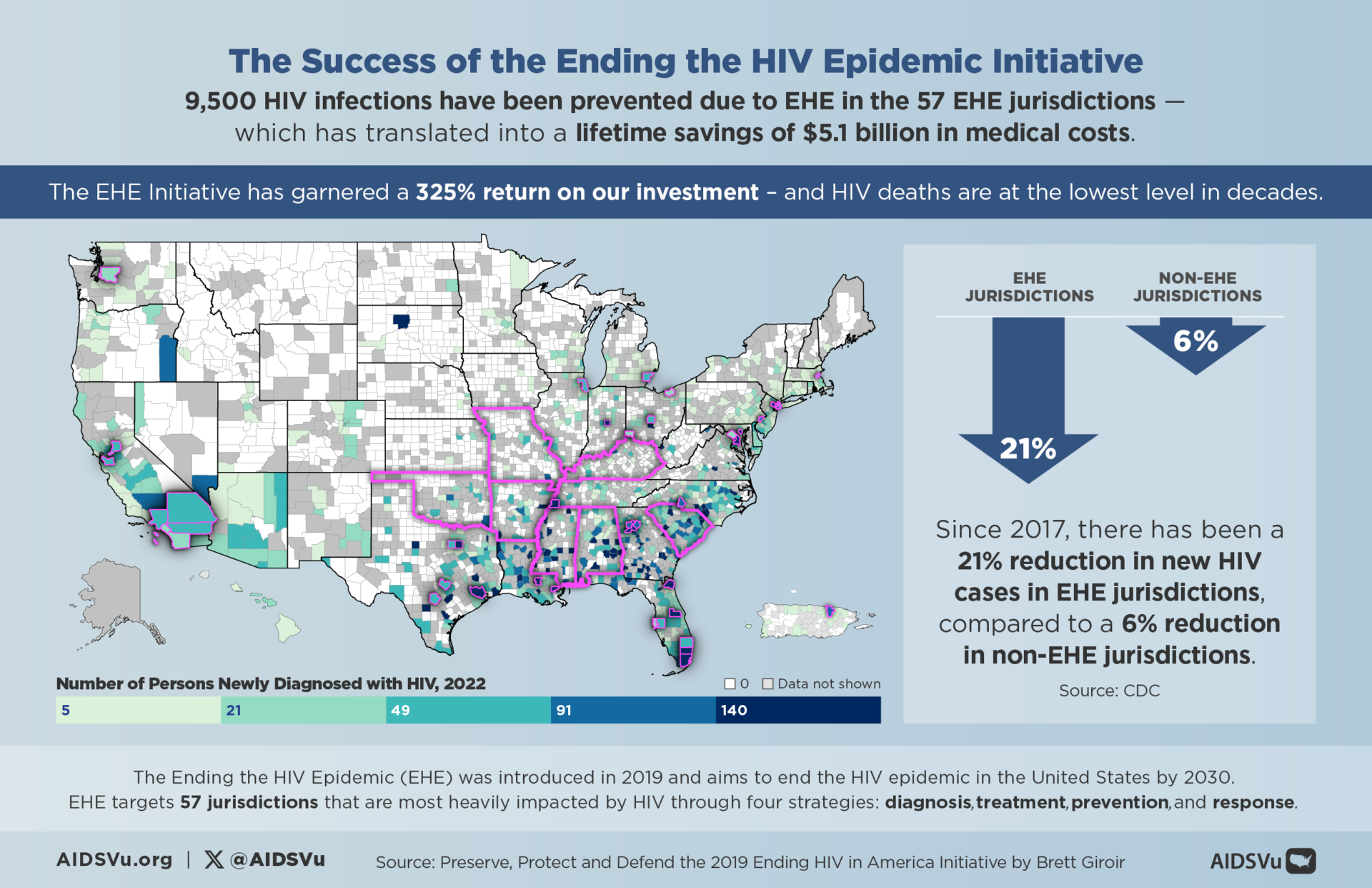
Between 2019 and 2021 alone, approximately 2,020 HIV infections have been prevented in EHE jurisdictions, which saved an estimated $1 billion in medical costs.
On March 18th, reports began to emerge that the Trump administration is exploring cuts to the CDC, including in the HIV prevention budget. Diminished prevention efforts would likely lead to an increase in new HIV diagnoses, with negative implications for individual well-being, public health, and health costs.
Crucially, the long-term costs of cutting federal HIV prevention would be fiscally irresponsible. Research shows that preventing a single HIV infection saves nearly $230,000 in medical costs. The average lifetime cost of treating a person with HIV is $500,000. It would only take only 40 more new HIV infections per state each year to surpass the $1 billion saved by cutting funding to the CDC Division of HIV Prevention. Without essential federal public health infrastructure for HIV prevention, new cases could quickly exceed this estimate.

The Local Impact
4 of every 5 dollars that CDC’s Division of HIV Prevention receives is distributed to state and local jurisdictions, enabling them to carry out health surveillance and effectively target at-risk communities. In addition, grants to state and local health departments, as well as national and community-based organizations (CBOs) support HIV testing, prevention efforts, and linking individuals to care, which ultimately improves both individual and public health outcomes. In their recent brief, Kaiser Family Foundation notes that in 2022, nearly 2 million HIV tests were conducted by 60 CDC-funded state and local health departments and 119 CBOs, leading to about 8,000 new HIV diagnoses – that is ¼ of all HIV diagnoses in the U.S.
In the same brief, KFF states that while state and local governments could theoretically compensate for federal cuts in HIV prevention funding, many are facing their own budget challenges and cuts to other critical programs, including Medicaid and residual COVID funding. In this situation, states will likely make different decisions based on their available funds and policy priorities, which could lead to inconsistent access to HIV prevention resources across the country. This could create disparities in care, with some regions having better access to services than others. This will also lead to job loss across the country as universities, local health departments, and community organizations cut staff in response to a lack of funds.
The Achievements of the Ending the Epidemic Plan
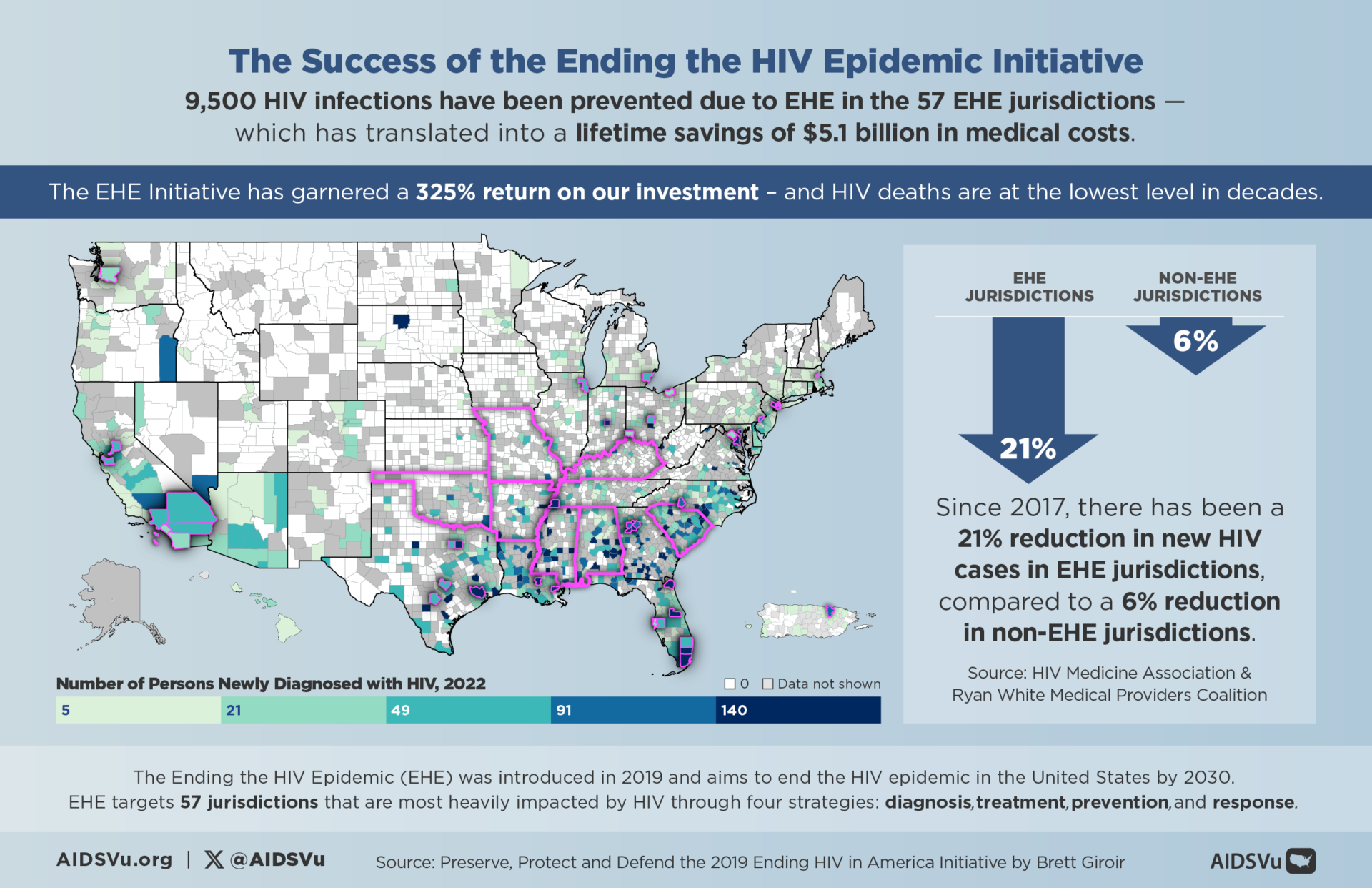
In 2019, President Trump made a historic commitment to ending the HIV epidemic in the United States by 2030, setting an ambitious goal to reduce new HIV infections and improve health outcomes for those living with the virus.
The national plan, Ending the HIV Epidemic: A Plan for America (EHE), is a ten-year federal initiative from the United States Department of Health & Human Services (HHS) with the goal of reducing new HIV infections to less than 3,000 per year by 2030. The initiative aims to reduce new HIV infections by 75% by 2025 and by at least 90% by 2030.
This initiative provided targeted support to specific “EHE” jurisdictions, boosting HIV efforts across the federal government with additional funding. As a result, there has been a 12% national decline in new HIV infections from 2018 to 2022, and a 21% decline in EHE jurisdictions from 2017 to 2022. CDC attributes these declines to factors such as increased prescriptions for pre-exposure prophylaxis (PrEP), improved viral suppression, and expanded HIV testing—efforts that CDC plays a central role in supporting. Without continued funding, these positive trends could be at risk.
Cutting funding for HIV prevention at this critical juncture would directly undermine this commitment, reversing the progress we have made and delaying the realization of a future where HIV is no longer a public health crisis.
The Bigger Picture
The HIV response plays a crucial role in strengthening public health systems – Efforts to prevent and treat HIV have not only saved countless lives but also helped to build more resilient public health infrastructures. Programs designed to combat HIV have improved surveillance, testing, and care systems that benefit the overall healthcare system, allowing for more efficient responses to a range of infectious diseases. By cutting HIV prevention funding, the U.S. risks undermining the progress made in strengthening these public health systems, weakening our capacity to respond to other infectious diseases.
Cuts to CDC funding would also further hollow out a public health workforce that has experienced challenges since the COVID-19 pandemic. Our healthcare systems are already under strain. Public health clinics, as well as state and local health departments, are currently overwhelmed with the demands of managing and treating a wide range of health issues. Many community-based HIV prevention services, which are crucial in reaching at-risk populations, would be forced to shut down, leaving gaps in care and increasing the burden on hospitals and other healthcare providers. Cuts to federal funding for HIV programs not only jeopardize public health efforts but exacerbate healthcare challenges for Americans and cost the U.S. more in health care costs.
Resources
- O’Neill Institute One-Pager, “Sustaining and Improving HIV Prevention in the United States”
- This resource outlines the importance of federal HIV prevention funding in reducing new HIV infections, improving health outcomes, and lowering national health care spending.
- O’Neill Institute One-Pager, “The Ryan White HIV/AIDS Program (RWHAP): The Program’s Parts Work Together to Make It Effective”
- “The Ryan White HIV/AIDS Program (RWHAP): The Program’s Parts Work Together to Make It Effective” highlights the successes of the program; specifically, that 91% of people in the RWHAP have achieved viral suppression compared to an estimated 65% of viral suppression overall in the U.S. The quick take also highlights the critical nature of all parts of the RWHAP, including Part F, which is being proposed for elimination, and how they all work together to provide a safety net for low-income PLWH.
- O’Neill Institute One-Pager, “Our Interconnected HIV Care Financing System is Under Threat”
-
“Our Interconnected HIV Care Financing System is Under Threat,” describes our progress at expanding insurance coverage and improving HIV outcomes with these insurance programs and the Ryan White HIV/AIDS Program working together and describes potential threats (Medicaid work requirements, reduced federal match for Medicaid expansion, and reductions or elimination of enhanced premium tax cuts) to these programs as part of the FY 2026 budget process.
-
- KFF
- The KFF Quick Take article explores the potential consequences of cuts to HIV prevention funding at the CDC, as proposed by the Trump administration. CDC currently provides the majority of federal funding for HIV prevention efforts across the U.S. The article highlights the risks associated with reducing this funding, such as a potential rise in HIV infections, which could negatively impact public health and lead to increased medical costs. It also discusses the role of state and local governments in continuing prevention efforts and the challenges they may face due to their own budget constraints. Additionally, the article touches on the implications for the Ending the HIV Epidemic initiative and the possible shift of HIV prevention funds to other agencies, though no formal proposal has been made.
- The KFF fact sheet provides an overview of the HIV/AIDS epidemic in the United States, highlighting key statistics and trends. As of 2022, there are over 1.2 million people living with HIV, with 31,800 new infections estimated annually. The sheet discusses the importance of early HIV diagnosis and treatment, including the benefits of antiretroviral therapy (ART), which helps achieve viral suppression and prevent transmission. It also addresses disparities in HIV impact, particularly among communities of color and certain groups such as gay and bisexual men. The document emphasizes the need for continued efforts in prevention, care, and support services to address the ongoing epidemic.
- The KFF Ending the HIV Epidemic (EHE) Funding Tracker provides detailed data on federal funding for the EHE initiative, which aims to reduce new HIV infections in the U.S. by 90% over the next decade. The tracker includes funding levels by year, agency, and grant mechanism, highlighting the allocation of funds to key areas such as the CDC, HRSA, and NIH. It also compares budget requests to actual appropriations, showing trends in federal support for the initiative. The document updates the public on how funds are distributed across high-burden jurisdictions and various agencies involved in HIV prevention and care efforts.
- The KFF fact sheet on U.S. federal funding for HIV/AIDS outlines trends in federal support for HIV initiatives over time, with a focus on fiscal years 2018 to 2022. It highlights that federal spending on HIV has grown significantly, reaching $43 billion in 2022, driven primarily by mandatory spending on Medicaid and Medicare. Domestic care and treatment programs account for the largest portion of the budget, while prevention, research, and global HIV efforts receive smaller allocations. The document also distinguishes between mandatory and discretionary funding, noting that mandatory spending now makes up a larger share of the total HIV budget. The fact sheet provides a detailed breakdown of funding categories, including care, prevention, and housing assistance.
- Funders Concerned About AIDS
- On April 10, 2025, FCAA released the 22nd edition of Philanthropy’s Response to HIV and AIDS. The latest issue explores 2023 grantmaking data from 6,285 grants, 706 funders, and roughly 2,900 grantee organizations, representing the most comprehensive study of philanthropy’s response to HIV and AIDS. Read the new report.
- CDC Funding Profiles:
- CDC maps HIV grant funding at the state-level across the U.S. This report includes data on grants and cooperative agreements for fiscal year 2023 (FY23), covering the period from October 1, 2022, to September 30, 2023. It focuses on funding that was obligated and awarded to states, the District of Columbia (DC), U.S. Territories, and Freely Associated States from the CDC’s domestic appropriations.
- CDC Fiscal Year 2023 Grant Funding By State
- Federal HIV Funding
- The HIV.gov Federal HIV Budget page provides information on the U.S. government’s funding allocations for HIV programs and services. It includes details on the budget for the Ending the HIV Epidemic initiative, which aims to reduce new HIV infections by 90% by 2030. The page outlines funding levels for various federal agencies involved in HIV prevention, care, and treatment, as well as for research and global efforts. Additionally, it highlights how federal funding supports both domestic and international HIV-related programs.
- Federal HIV Budget
- EHE Funding:
- The HIV.gov page on Ending the HIV Epidemic (EHE) funding outlines the federal investments aimed at reducing new HIV infections by 90% by 2030. It details the funding allocated to support prevention, care, and treatment efforts, focusing on high-burden areas across the U.S. The page explains how the U.S. government supports the EHE initiative through targeted grants and investments in various agencies, including the CDC, HRSA, and NIH. It highlights the role of funding in ensuring resources are available for the communities most affected by HIV, including minority and underserved populations.
- HIV. gov:
- The HIV.gov page on HIV Prevention Activities provides an overview of federal efforts aimed at preventing HIV transmission. It highlights key prevention strategies, such as the use of HIV medications like PrEP (pre-exposure prophylaxis) and PEP (post-exposure prophylaxis), reducing sexual and drug-related risks, and preventing perinatal HIV transmission. The page also discusses ongoing research into future prevention options, including HIV vaccines and long-acting prevention tools. These initiatives are part of the broader federal response to curb the HIV epidemic in the U.S. and globally.
- EHE Funding:
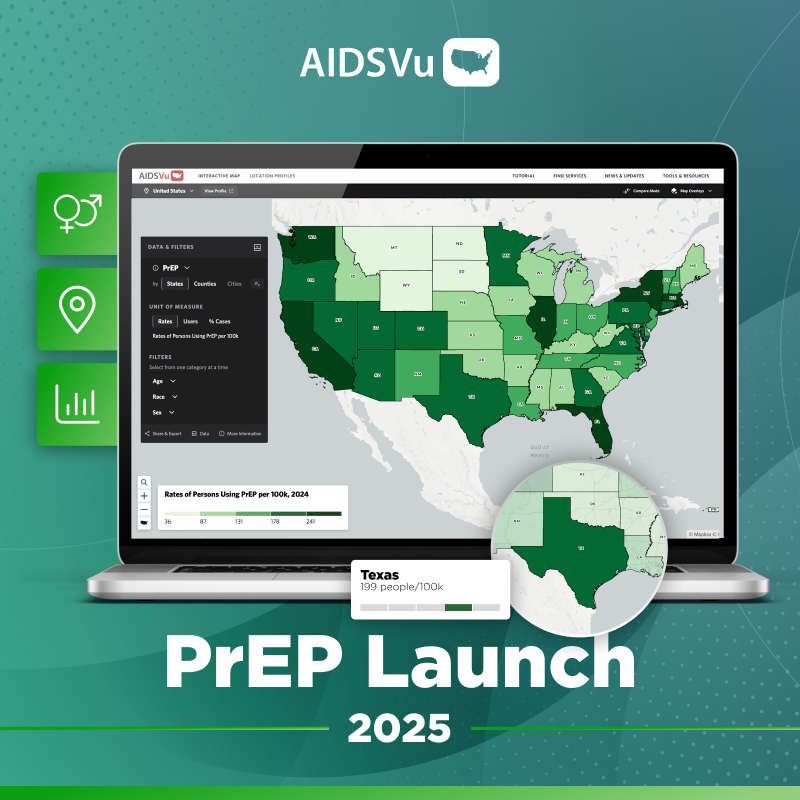
5 Ways to Use AIDSVu
View local statistics
National-, state-, and city-level profiles including data on social determinants of health.
Learn MoreExplore maps
Interactive maps including social determinants of health and other comparison maps.
Learn MoreShare infographics
Infographics presenting insights on the social determinants of health mapped on AIDSVu.
Learn More