Implementation Challenges and Successes
The implementation of the EHE initiative has revealed both the potential and the limitations of large-scale public health interventions. On the success side, the initiative has demonstrably expanded HIV prevention and care services in priority jurisdictions. CDC data indicate that EHE-funded programs have increased HIV testing, improved linkage to care rates, and expanded PrEP access in targeted areas. HRSA-funded health centers serving EHE priority areas have conducted 1.7 million HIV tests annually and serve nearly 9 million patients, of whom 79% are racial and ethnic minorities.
However, implementation has also faced significant challenges that highlight the complexity of ending an epidemic rooted in structural inequities. Workforce shortages represent a critical barrier, with an estimated 80% of counties in 14 Southern states having no experienced HIV clinicians. This shortage is particularly acute in rural areas, where geographic barriers compound workforce limitations. The proposed Bio-Preparedness Workforce Pilot Program, which would train and deploy HIV and infectious disease specialists to underserved areas, has faced political resistance and funding challenges despite broad support from medical and public health organizations.
Stigma and discrimination continue to pose formidable barriers to the initiative’s success, particularly for key populations most affected by HIV. Despite scientific advances and policy changes, many people continue to face rejection, judgment, and discrimination when seeking HIV-related services. This is particularly challenging for gay and bisexual men, transgender individuals, people who use drugs, and sex workers, who may avoid healthcare settings where they fear mistreatment.
The COVID-19 pandemic created additional implementation challenges by disrupting healthcare delivery, redirecting public health resources, and creating new barriers to accessing services. However, it also accelerated some innovations, including expanded use of telehealth, at-home testing, and flexible service delivery models that have been incorporated into ongoing EHE programming.
The Science Behind the Strategy
The EHE initiative is grounded in robust scientific evidence about effective HIV prevention and treatment interventions. The strategy leverages decades of research demonstrating that combination prevention approaches—using multiple, complementary interventions simultaneously—can achieve greater impact than any single intervention alone.
The “treatment as prevention” paradigm forms a cornerstone of the EHE strategy, based on definitive evidence that people with HIV who achieve and maintain undetectable viral loads cannot transmit the virus sexually. This scientific breakthrough transformed HIV treatment from a purely individual health intervention to a powerful prevention tool. The initiative emphasizes rapid initiation of antiretroviral therapy (ART) and comprehensive support services to help people achieve and maintain viral suppression.
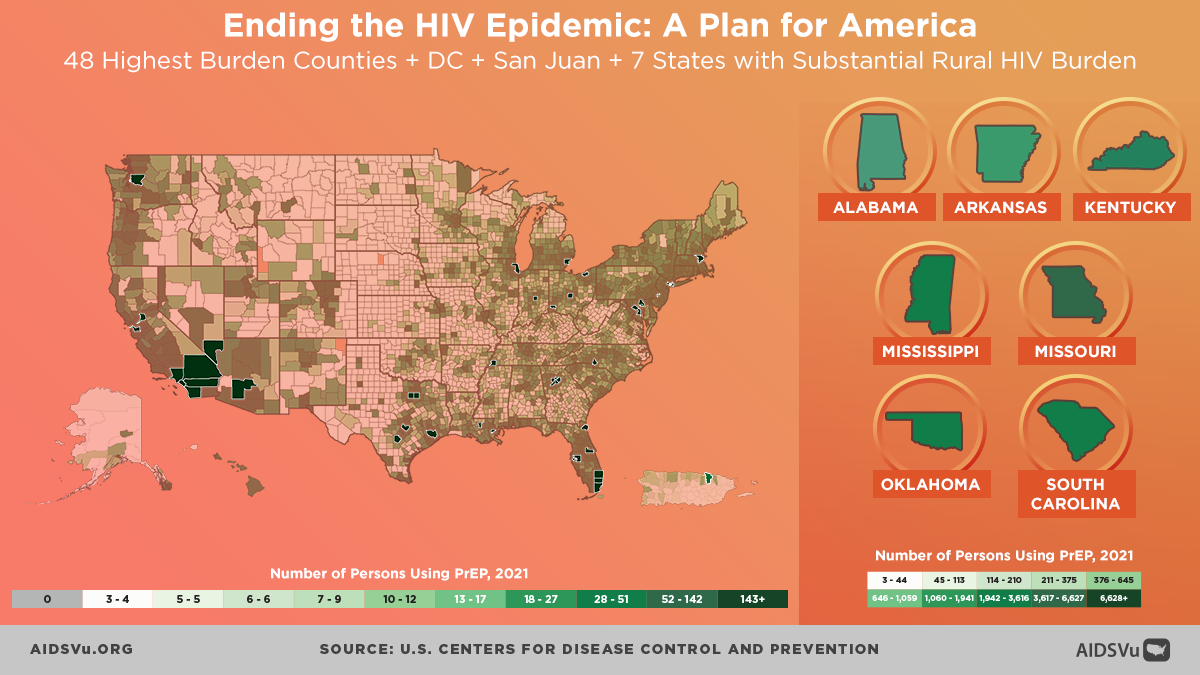
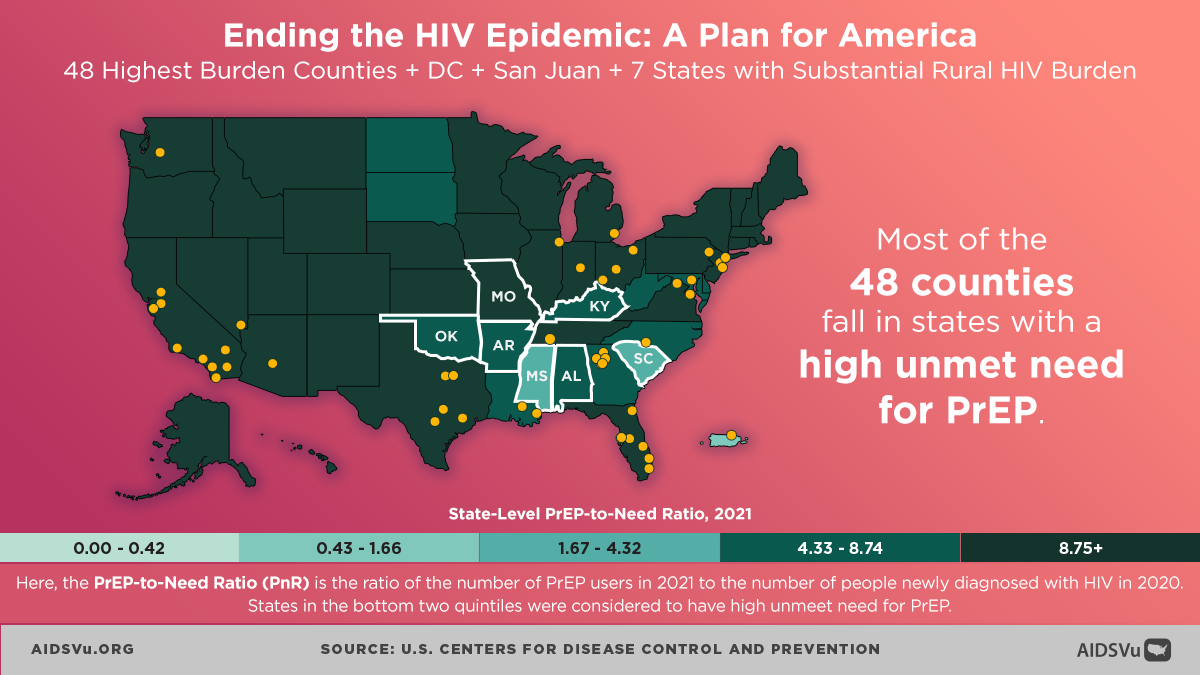
Pre-exposure prophylaxis (PrEP) represents another scientific pillar of the initiative, with clinical trials demonstrating more than 99% effectiveness at preventing HIV acquisition when taken consistently. The initiative has focused on expanding PrEP access, particularly among populations at highest risk, while addressing barriers including cost, stigma, and provider knowledge. However, PrEP uptake has remained lower than optimal, particularly among women and communities of color, requiring ongoing attention to access and equity issues.
The initiative also draws on implementation science research that provides insights into how to effectively translate proven interventions into real-world settings. This includes research on community engagement strategies, cultural adaptation of interventions, integration of services across different providers and settings, and approaches to addressing structural barriers that affect intervention uptake and effectiveness.
Community Engagement and Health Equity
Central to the EHE initiative’s design is recognition that ending the HIV epidemic requires meaningful engagement with communities most affected by HIV, particularly communities that have historically faced marginalization and discrimination. The initiative explicitly emphasizes community engagement as both a strategy and a value, recognizing that sustainable change must be driven by and accountable to the people it aims to serve.
HRSA has developed a comprehensive community engagement framework with five guiding principles for EHE work: meaningful community involvement, cultural responsiveness, addressing structural barriers, building community capacity, and ensuring accountability to communities. This framework acknowledges that effective HIV programming cannot be imposed from outside but must emerge from partnerships with communities that bring lived experience, cultural knowledge, and existing trust relationships.
The focus on health equity represents both a goal and a strategy within the EHE initiative. The initiative recognizes that HIV disparities are not accidental but result from structural inequities including racism, homophobia, transphobia, poverty, and other forms of systematic oppression. Addressing these disparities requires not only expanding access to HIV services but also confronting the underlying social and economic conditions that create vulnerability to HIV.
This equity focus has led to targeted investments in organizations serving communities of color, LGBTQ+ communities, and other marginalized populations. It has also influenced the types of interventions supported, with increased emphasis on structural interventions such as housing support, transportation assistance, and economic empowerment programs that address social determinants of HIV vulnerability.
Integration with Broader Health and Social Systems
The EHE initiative operates within a broader ecosystem of health and social services, requiring coordination and integration across multiple systems and sectors. This includes integration with existing HIV programs such as the Ryan White HIV/AIDS Program, coordination with broader public health initiatives, and alignment with social services that address determinants of health.
The relationship between EHE and the Ryan White Program illustrates both opportunities and challenges in system integration. Ryan White funding provides essential HIV care and support services that complement EHE prevention and early intervention efforts. However, the programs operate under different funding mechanisms, regulations, and reporting requirements, creating coordination challenges for local implementers.
Integration with substance abuse treatment, mental health services, and criminal justice systems represents another critical area for EHE implementation. Many people at risk for or living with HIV also interact with these systems, creating opportunities for coordinated interventions. However, these systems often operate independently, with different priorities, cultures, and approaches that can create barriers to integration.
The initiative has increasingly recognized the importance of addressing social determinants of health, including housing, employment, education, and food security. While EHE funding cannot directly address all these issues, the initiative has supported innovations such as housing support for people with HIV, transportation assistance for accessing care, and coordination with other social services that affect HIV outcomes.
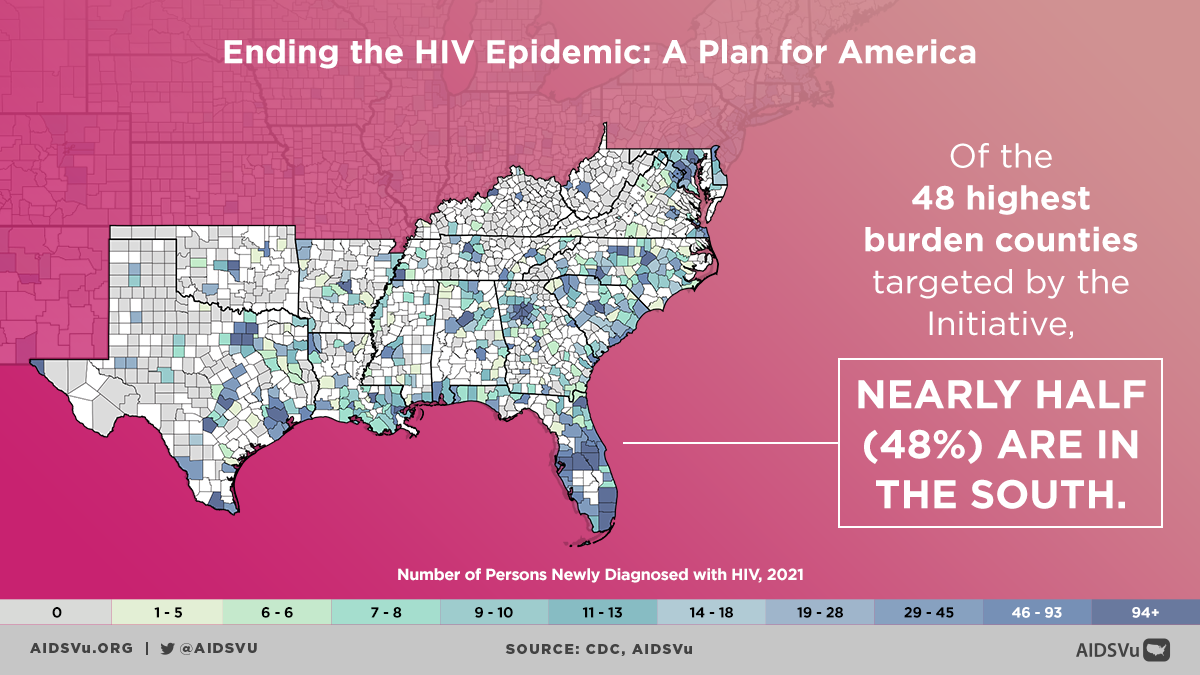
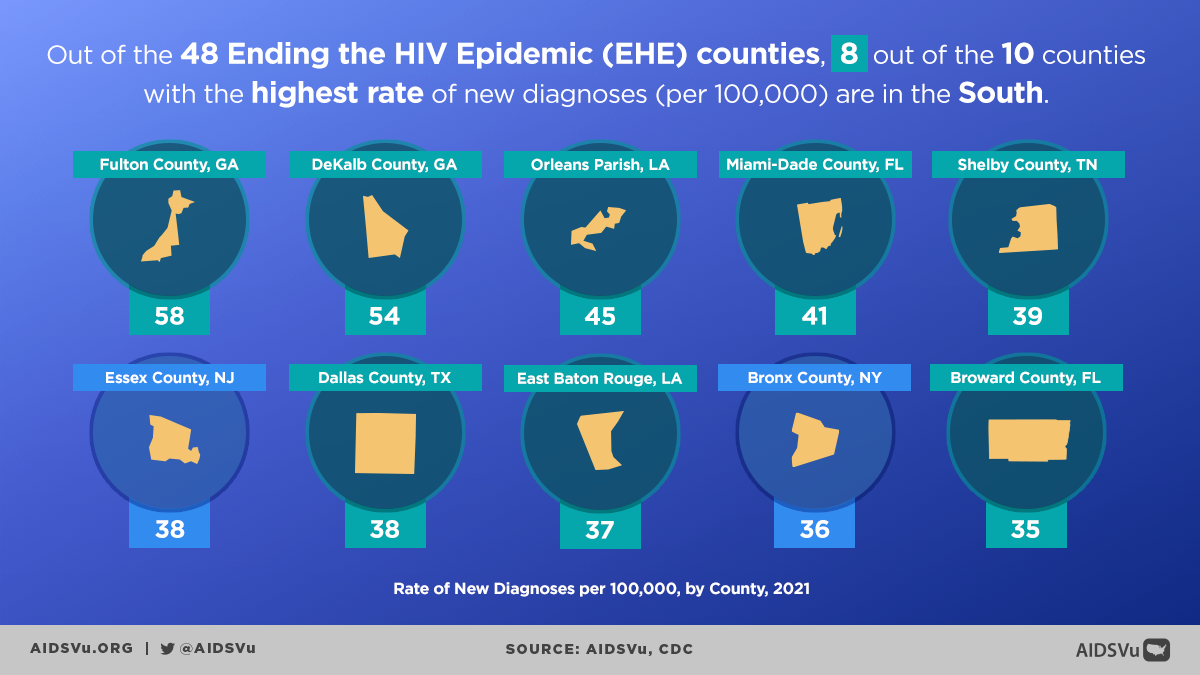
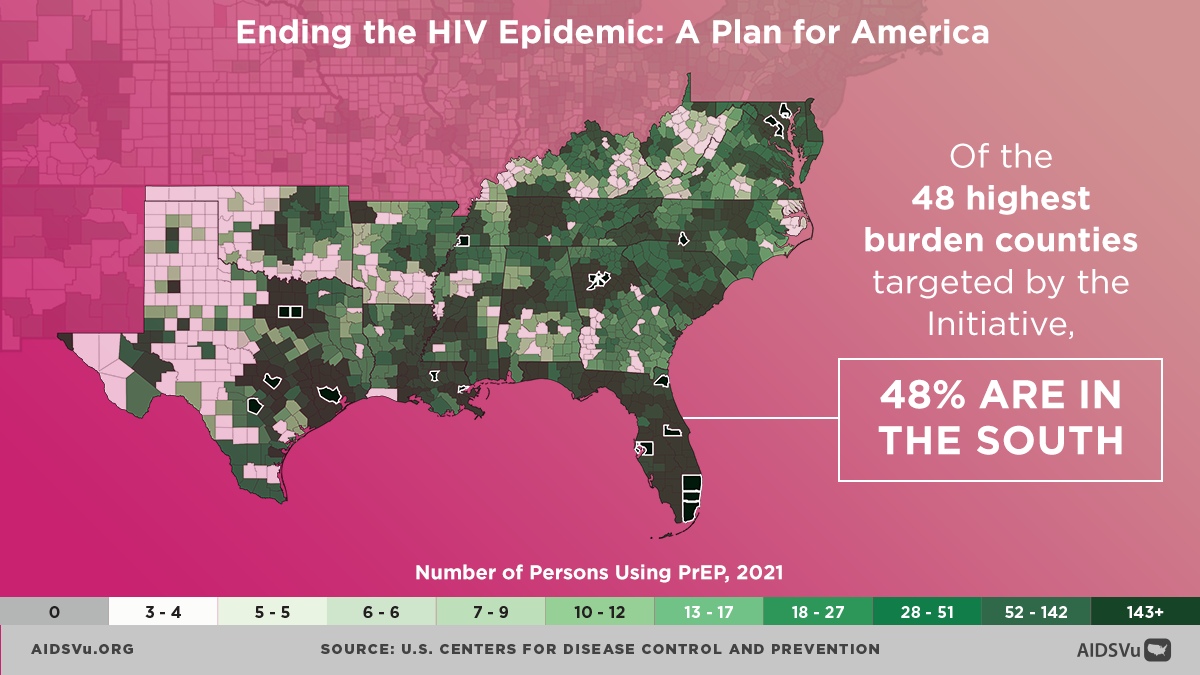
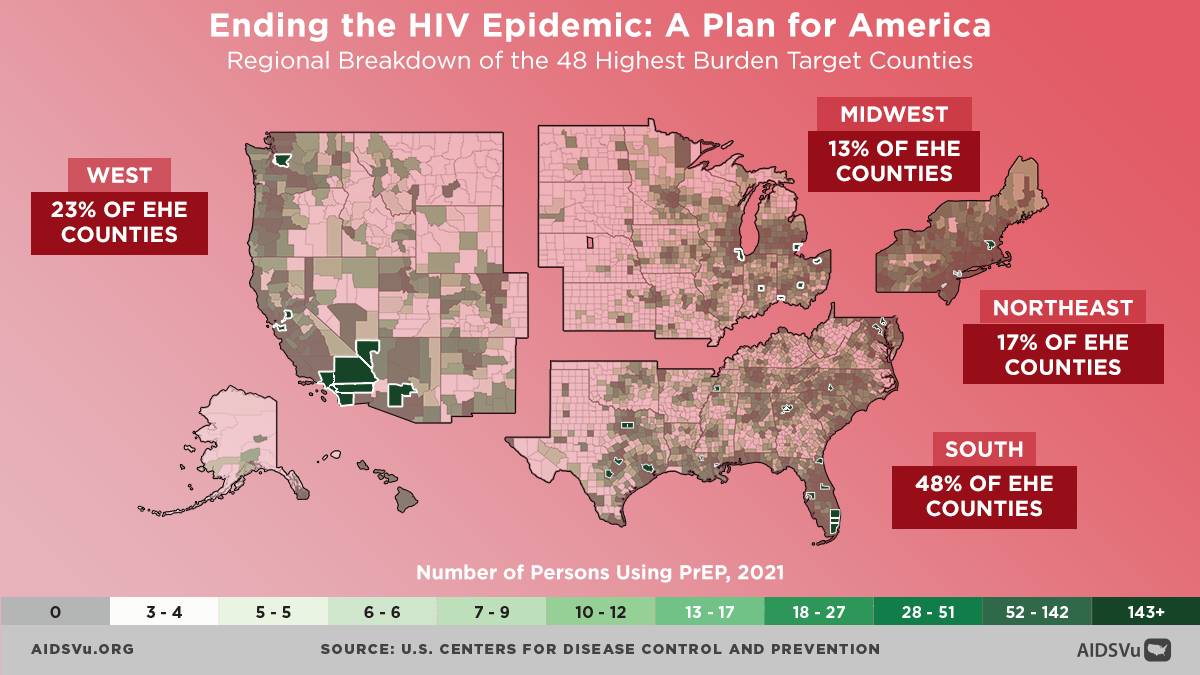
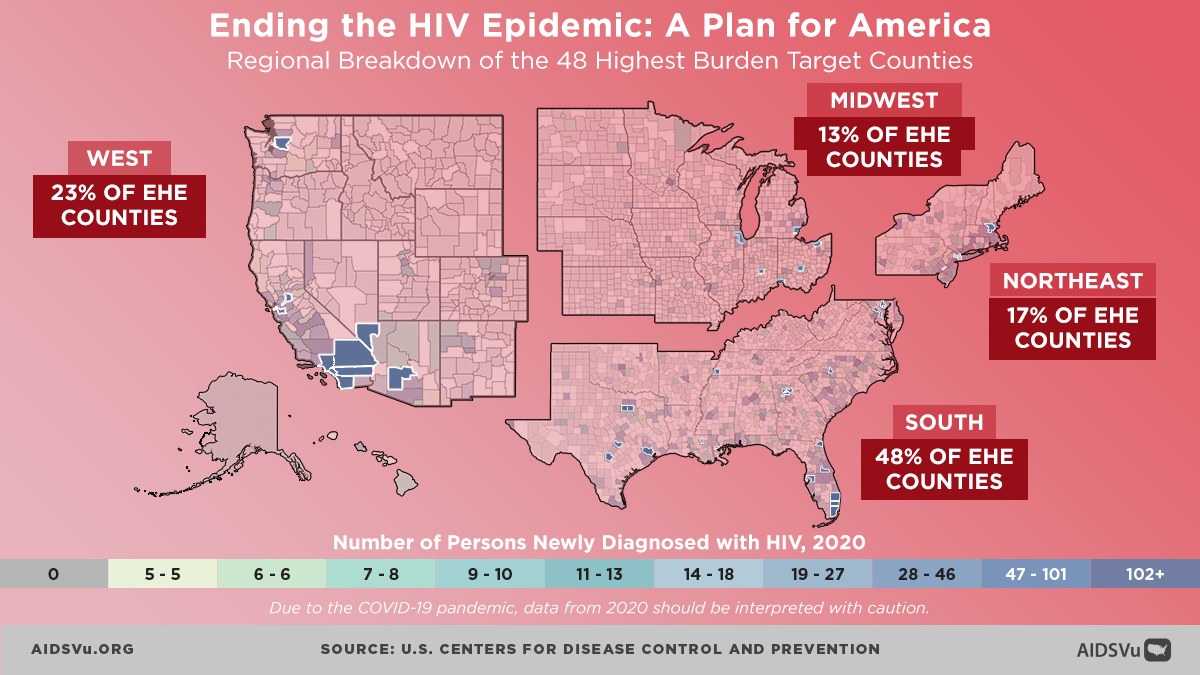
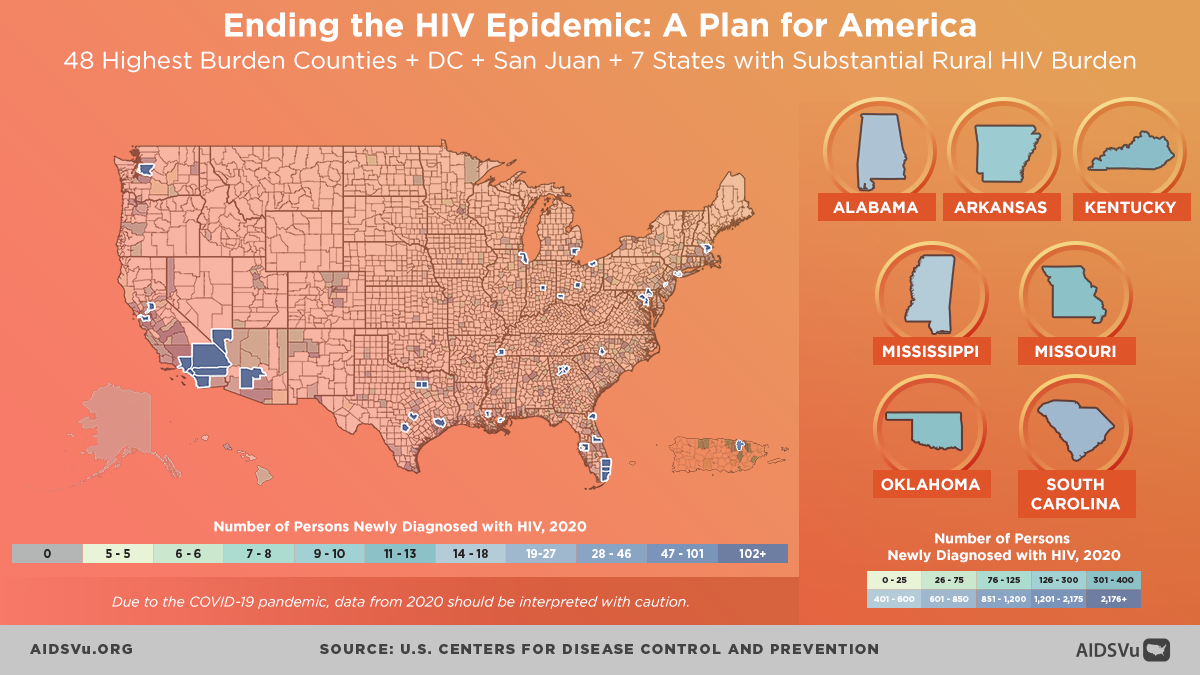
Of the 48 highest burden counties targeted by the initiative, 48% are in the South.
In 63% of the 48 target counties and DC, the percent of people living in poverty is higher than the national average.
Most of the 48 target counties fall in states with a high unmet need for PrEP.