Understanding Identity and Community
The terms Hispanic, Latino, Latinx, and Latine represent different approaches to describing a diverse community that encompasses people with origins in Spanish-speaking countries and Brazil. For the purposes of this analysis, we use “Hispanic/Latinx/Latine” to honor this diversity while recognizing that individuals within these communities may prefer different terms to describe their identity.
This linguistic complexity reflects the broader diversity within Hispanic/Latinx/Latine communities, which encompass dozens of countries of origin, multiple languages, varied immigration histories, different socioeconomic circumstances, and distinct cultural traditions. This diversity means that effective HIV prevention and care approaches must be tailored to specific community needs rather than treating Hispanic/Latinx/Latine populations as a monolithic group.
The Growing Impact: A Community Under Pressure
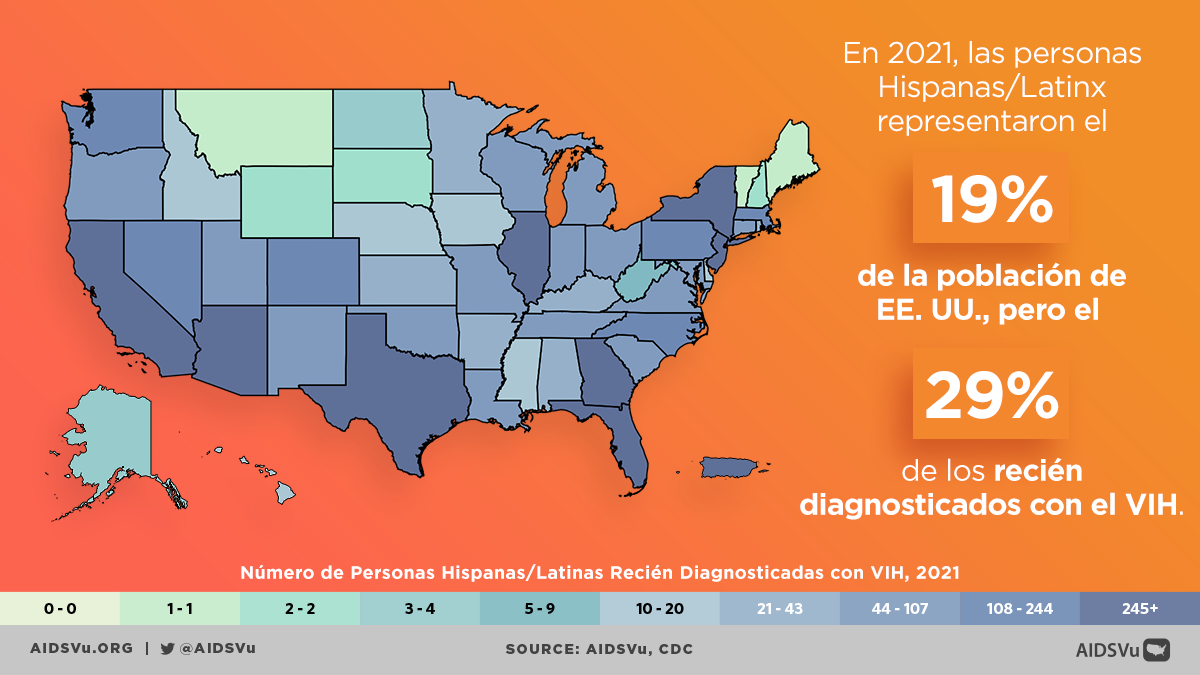
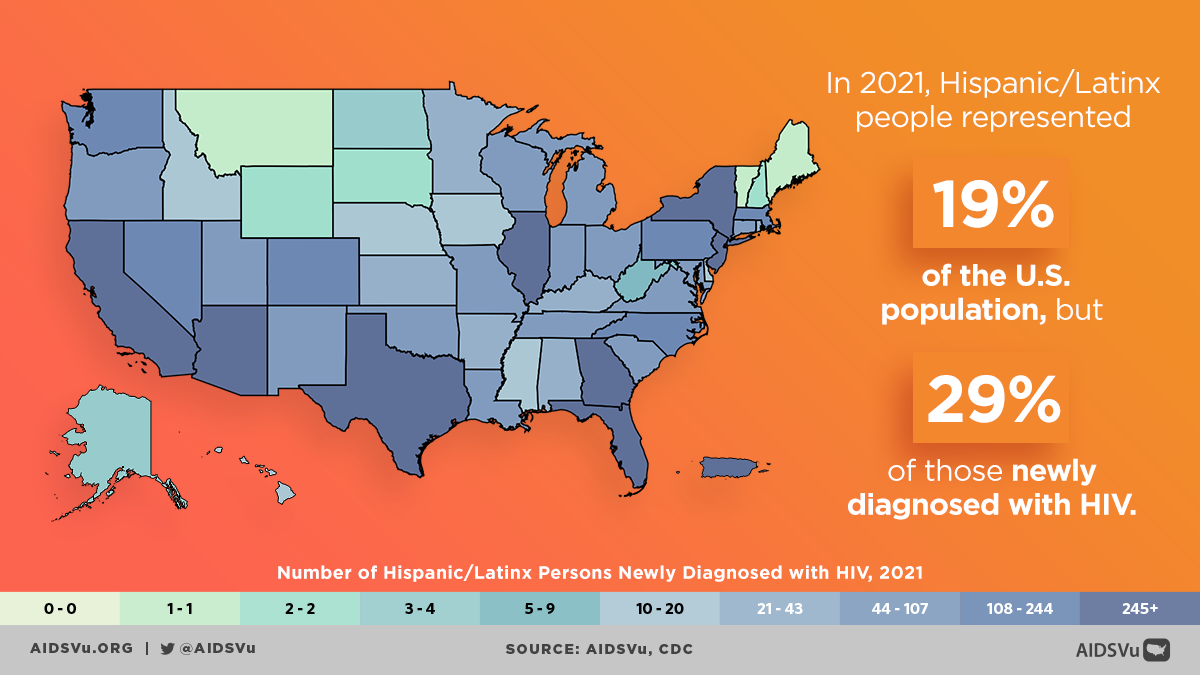
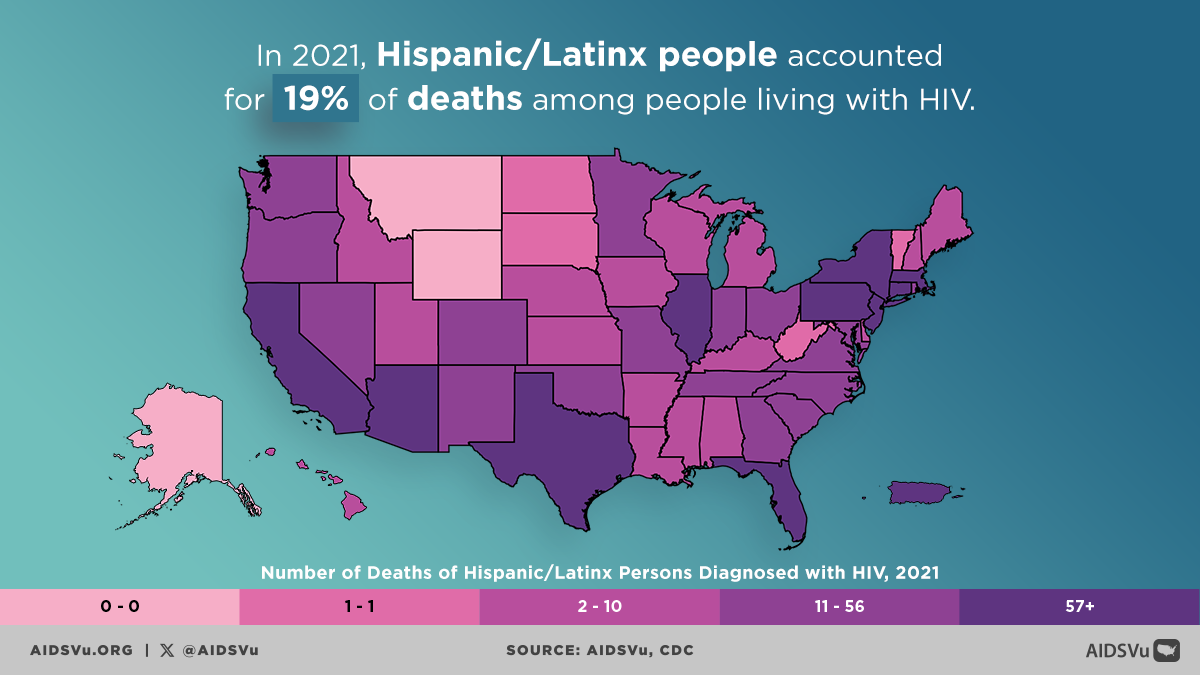
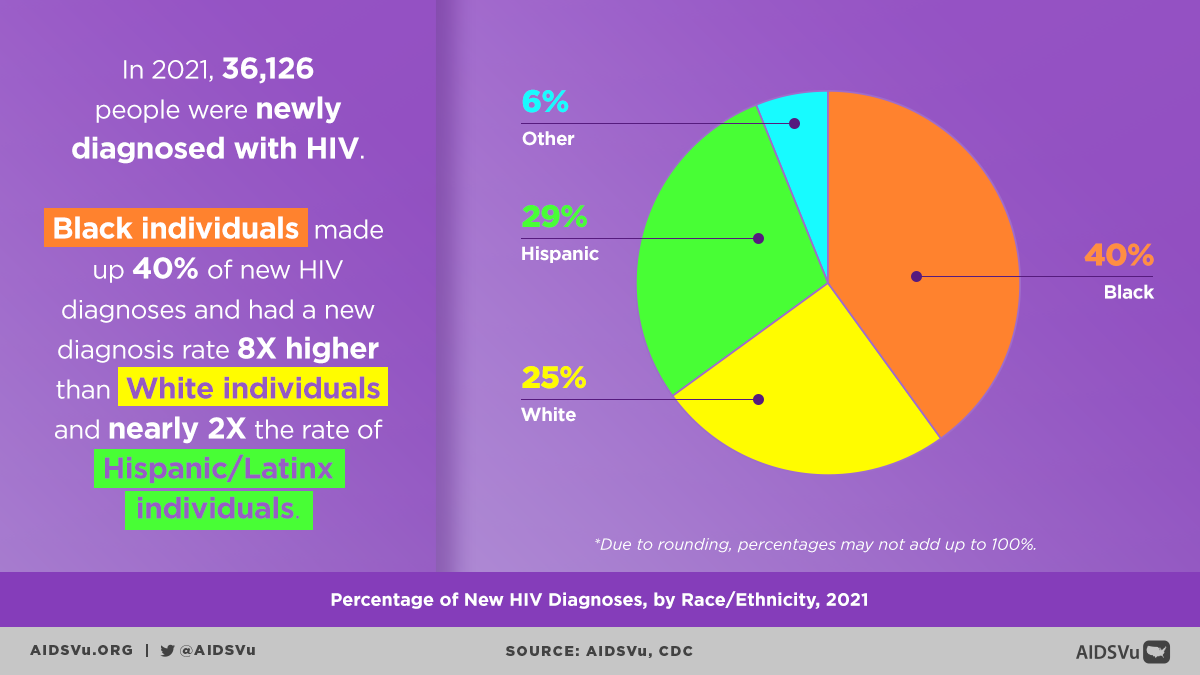
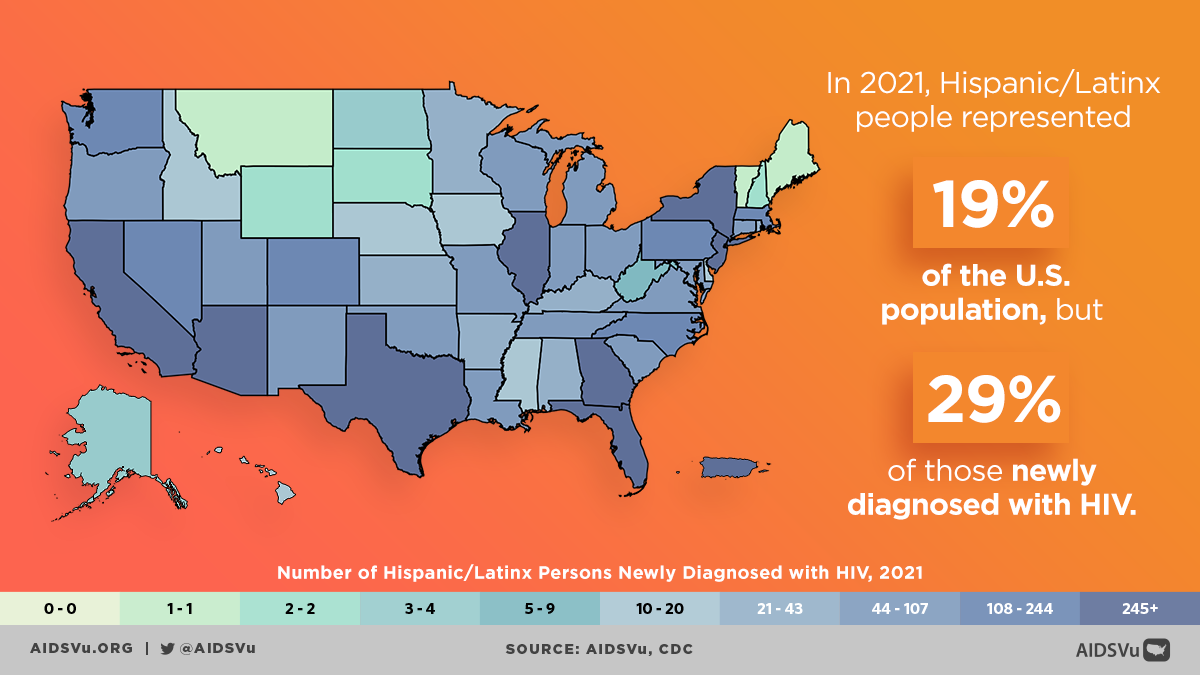
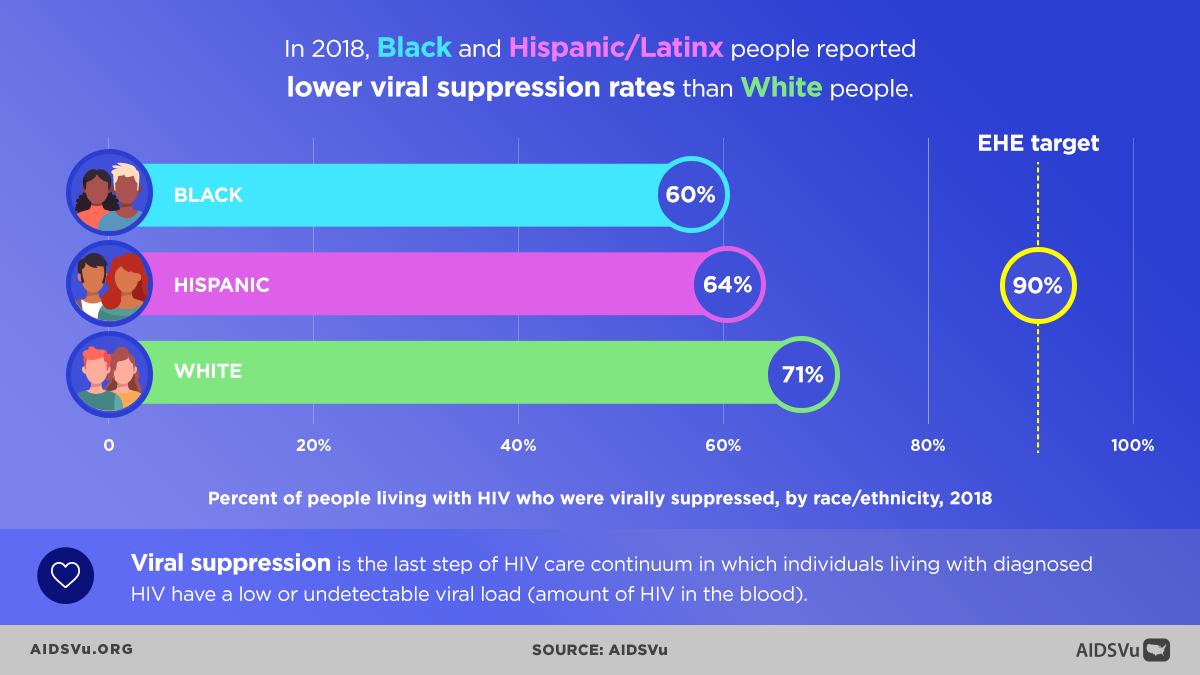
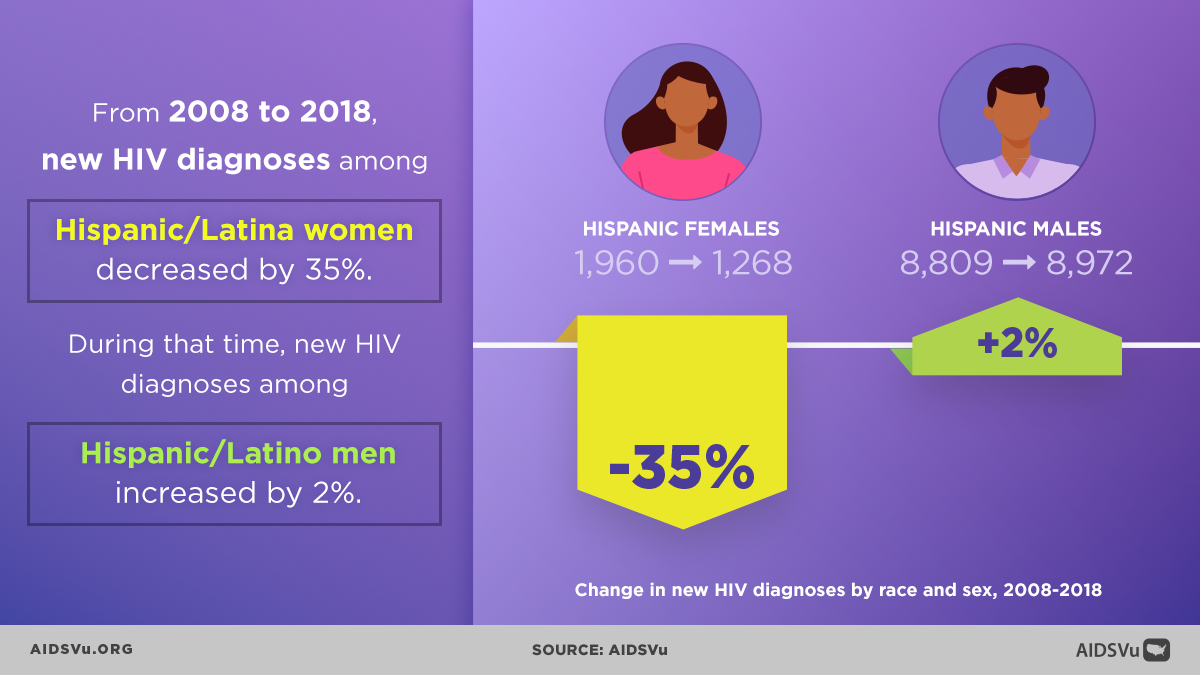
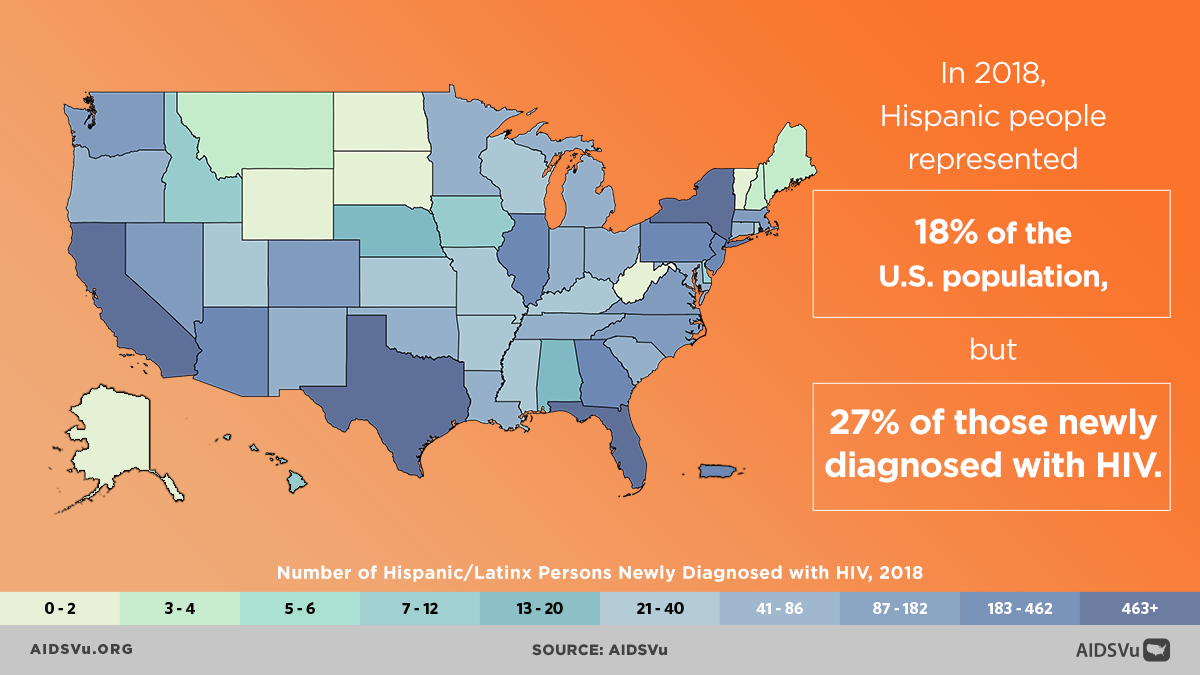
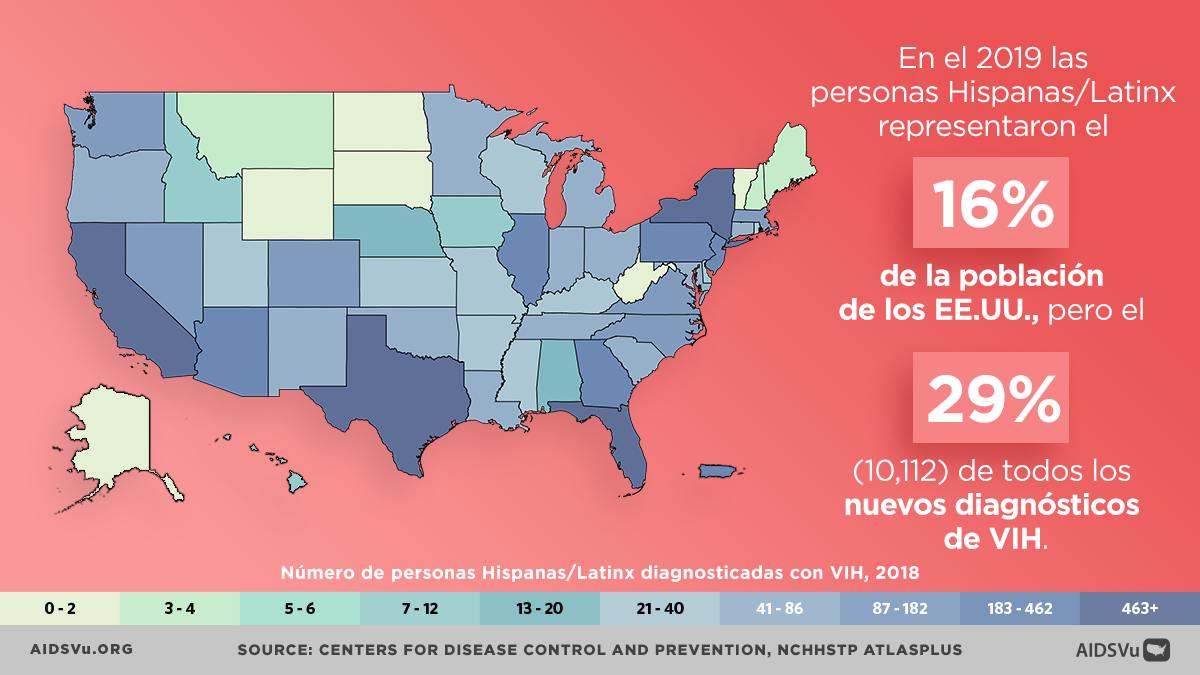
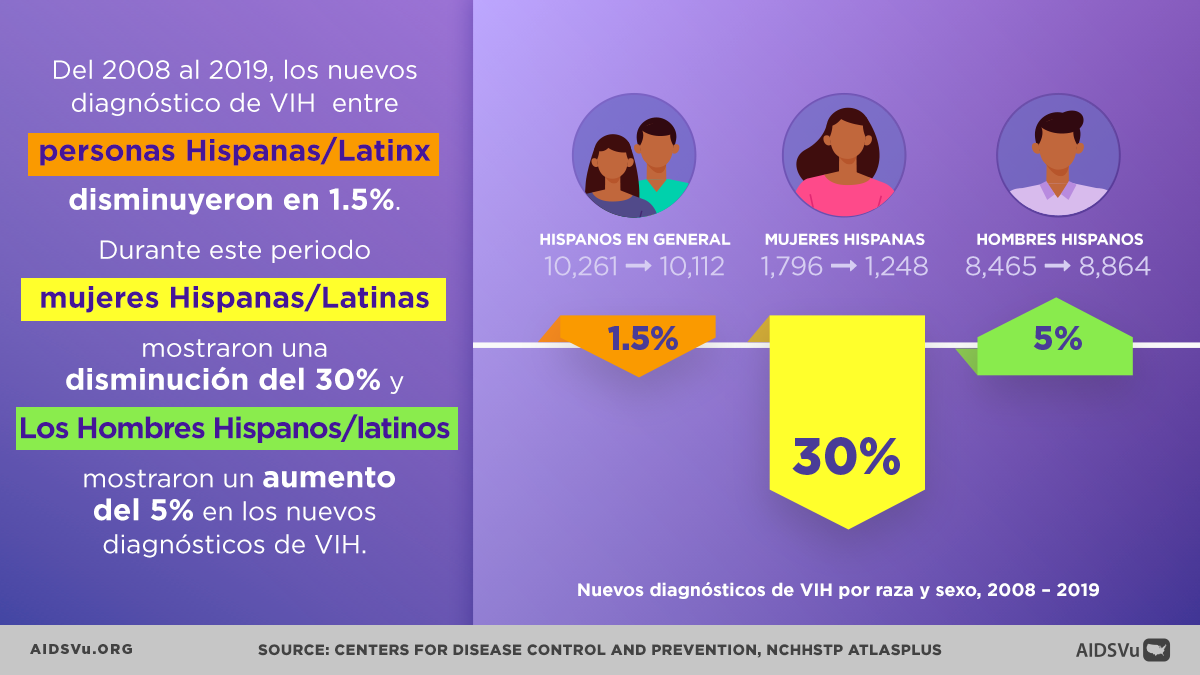
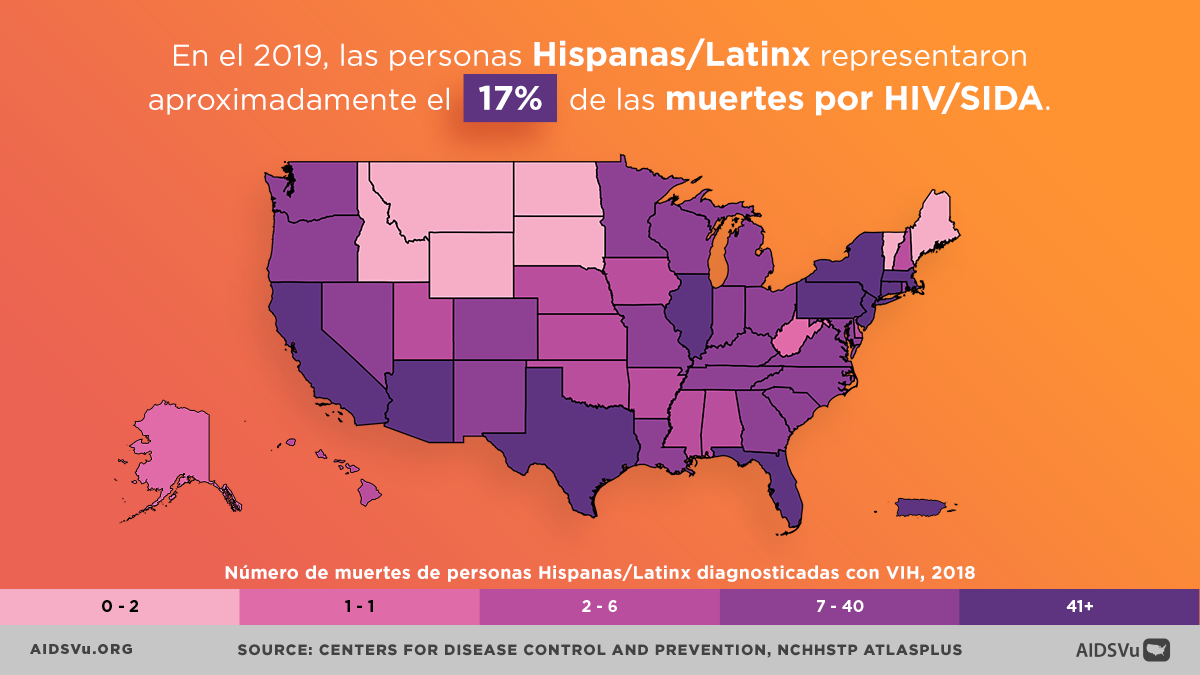
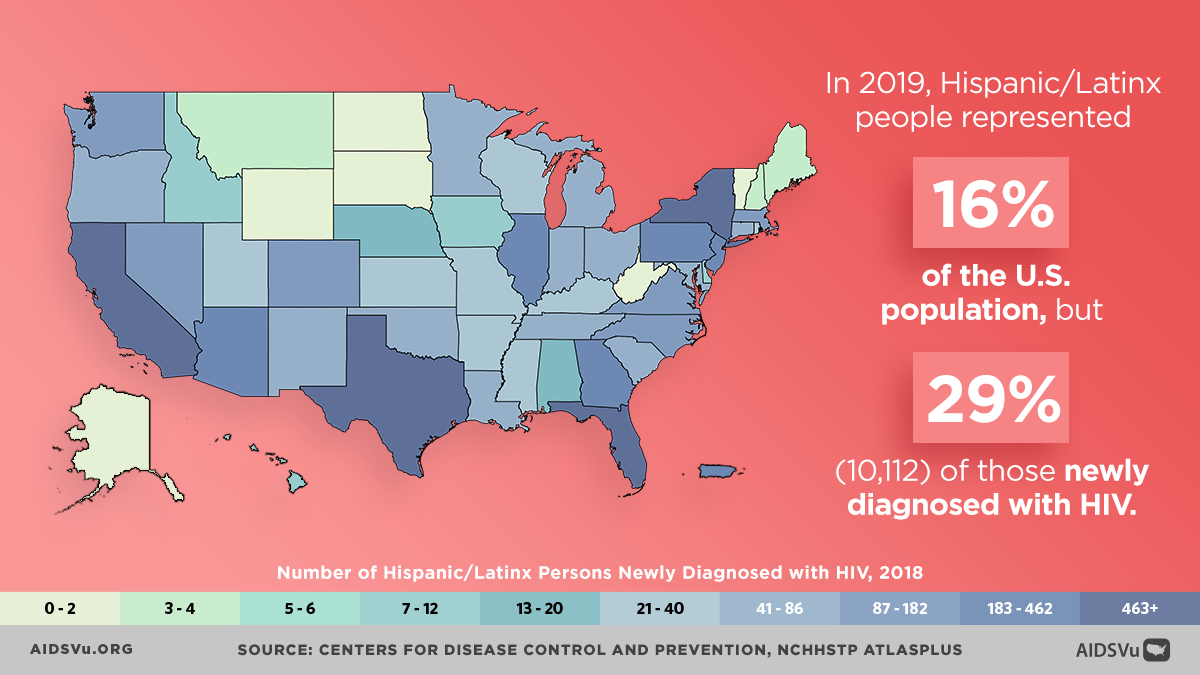
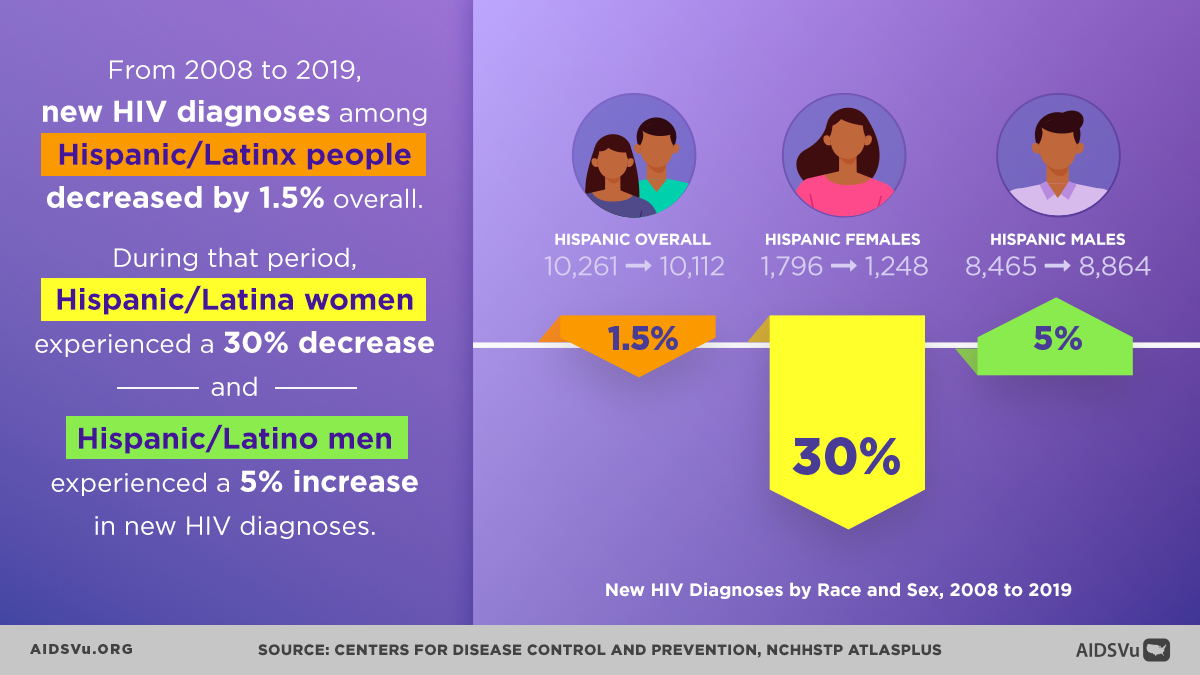
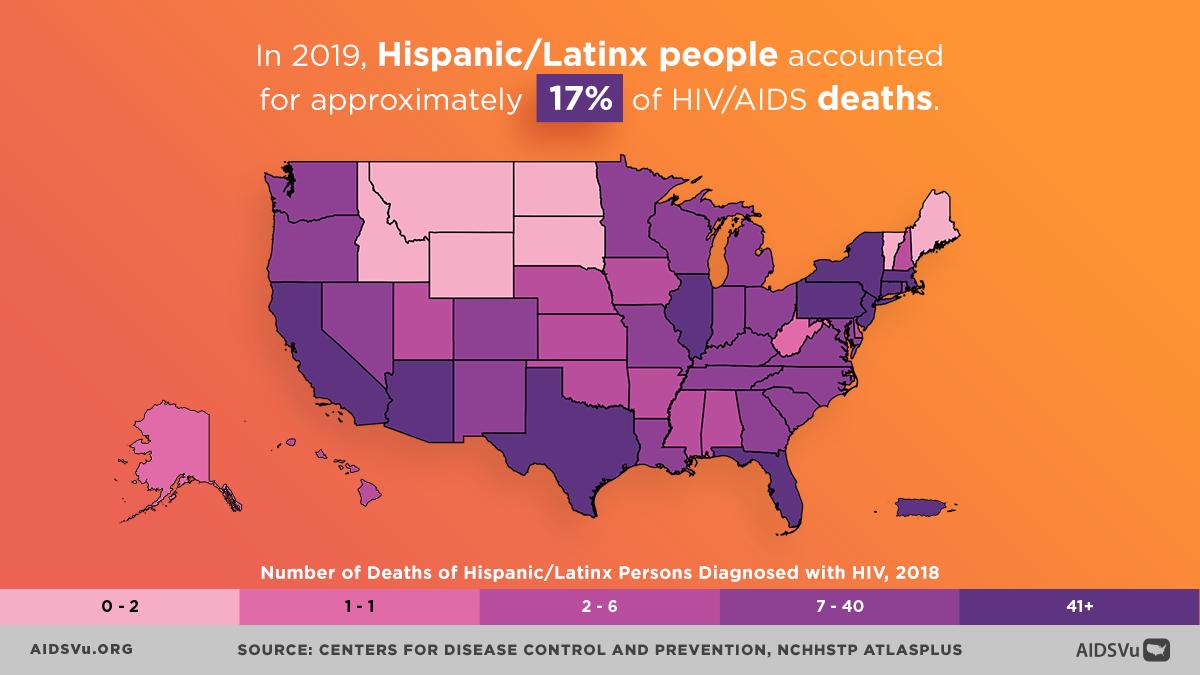
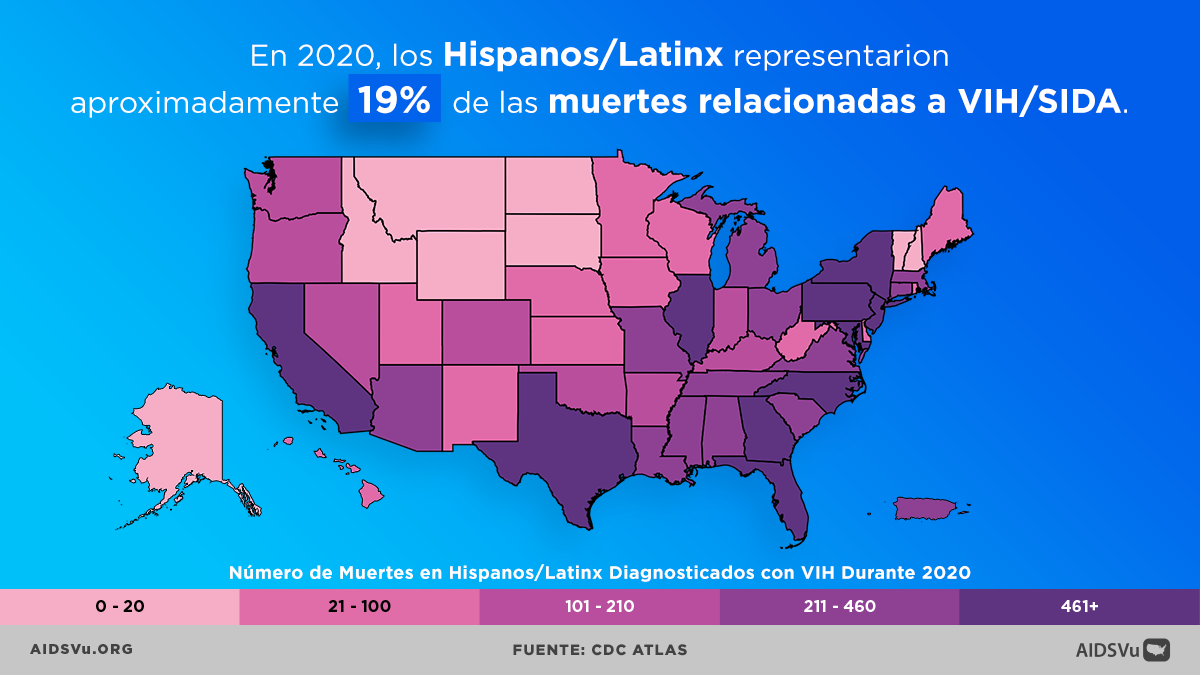
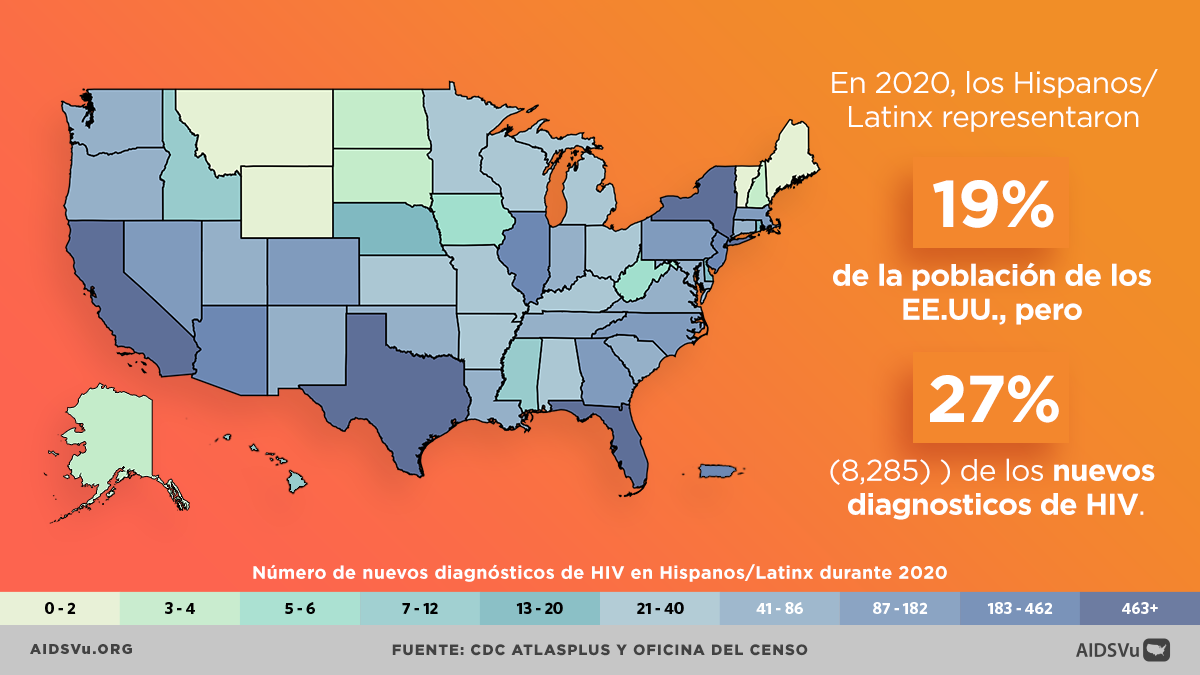
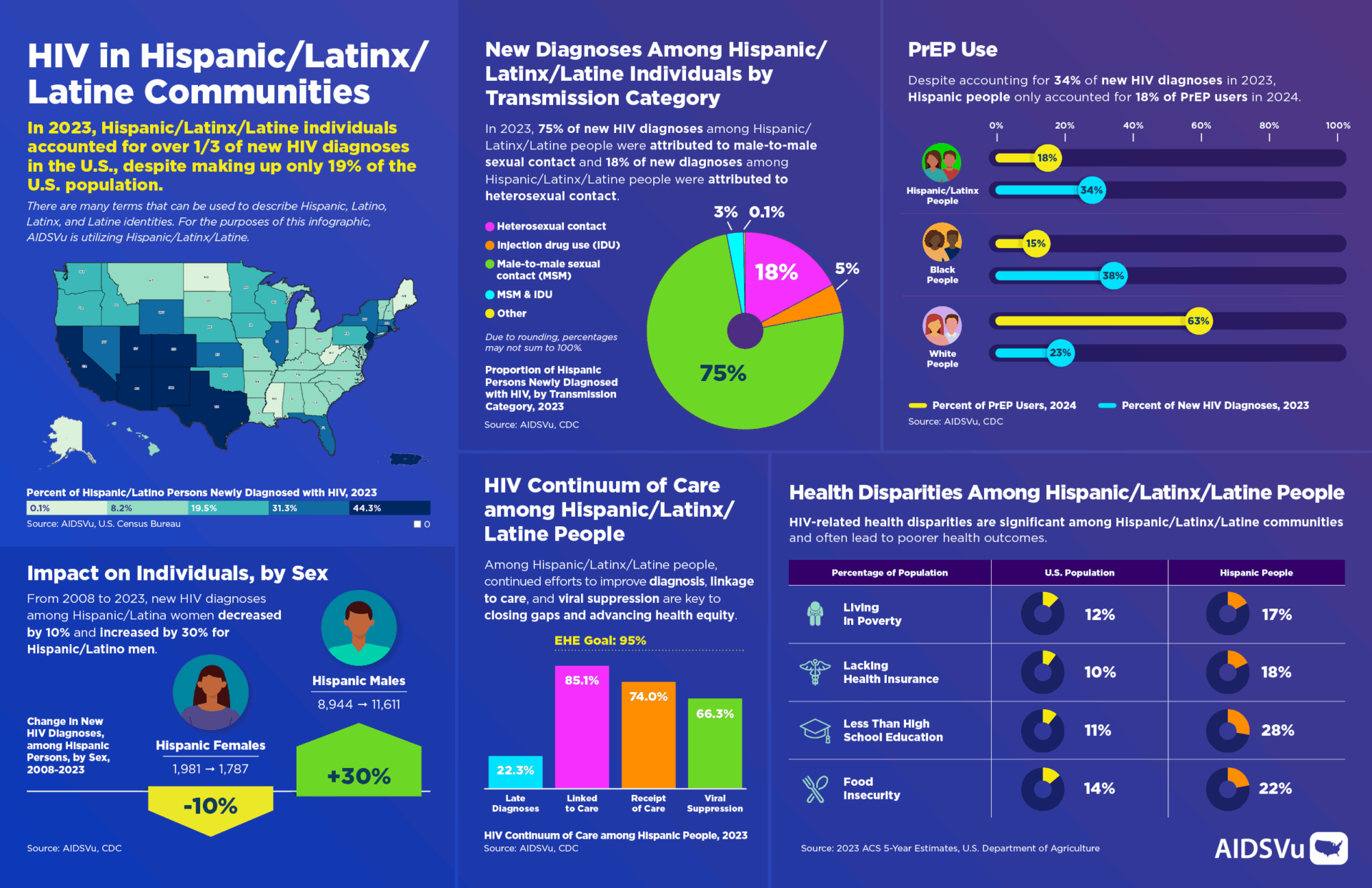
HIV has an increasingly disproportionate impact on Hispanic/Latinx/Latine populations in the United States, representing a troubling trend that demands urgent attention. In 2022, Hispanic/Latinx/Latine people represented 32% of new HIV diagnoses despite making up only 18% of the U.S. population. This disparity has been worsening over time, with HIV diagnoses among Hispanic/Latinx/Latine people increasing by 17% between 2018 and 2022, even as overall HIV diagnoses remained relatively stable.
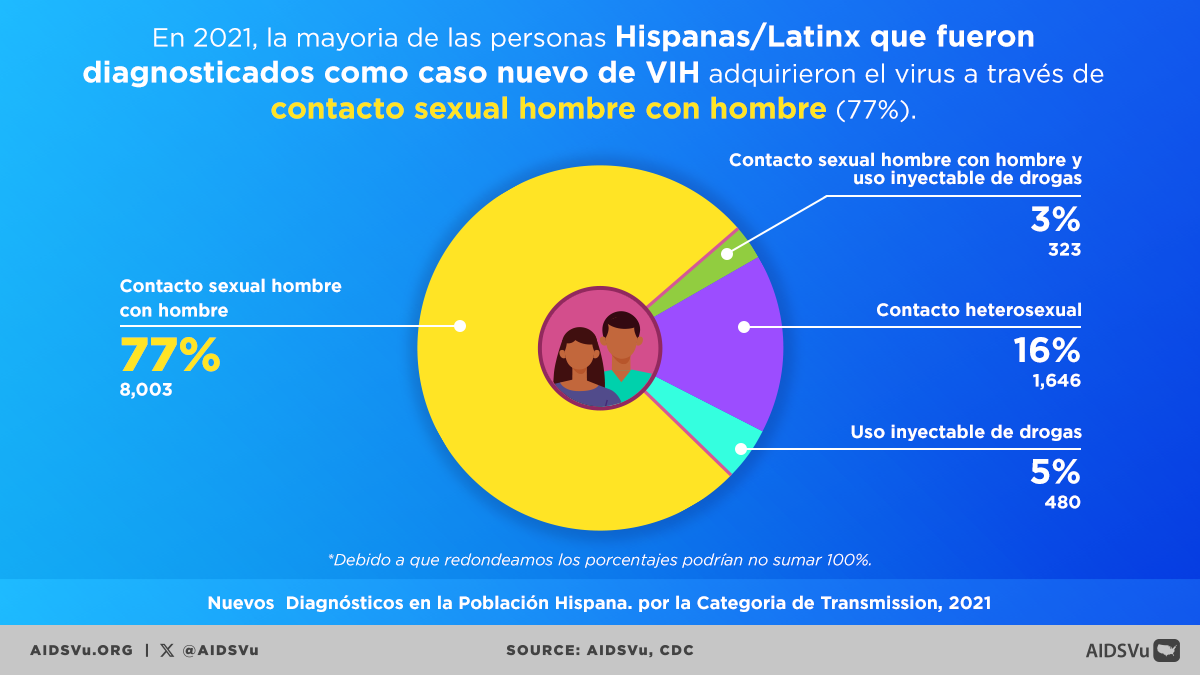
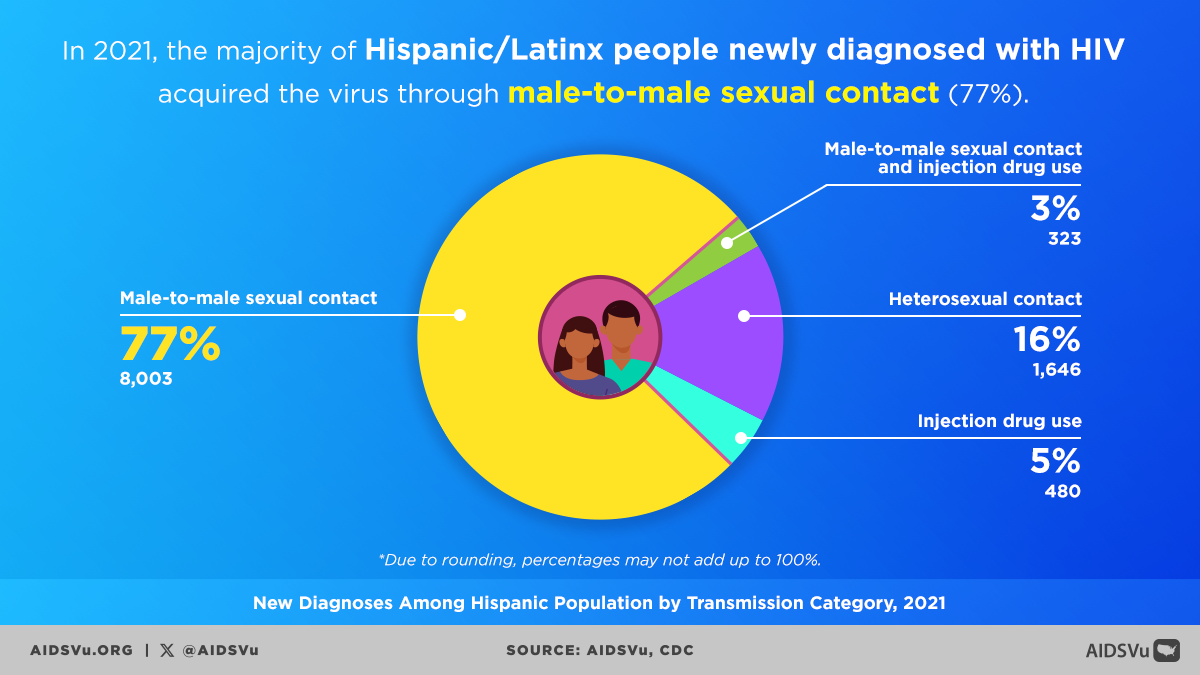
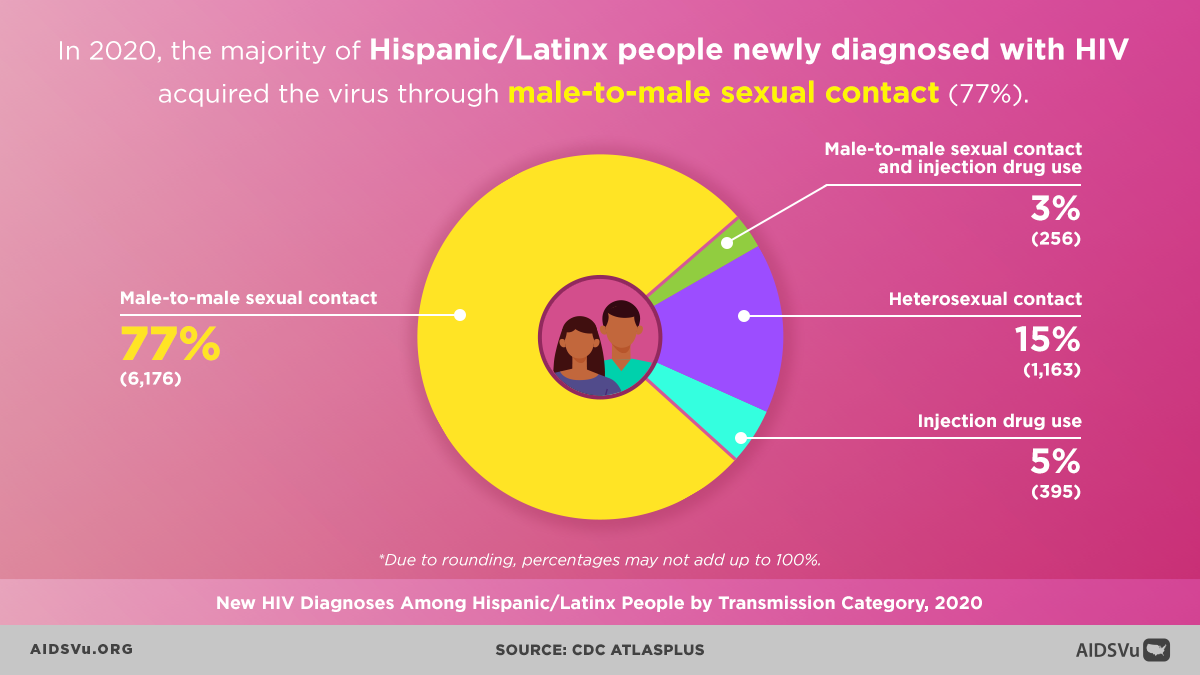
Hispanic/Latinx/Latine people now have the second-highest rate of new HIV diagnoses among all racial and ethnic groups, with approximately 19 new diagnoses per 100,000 people—nearly double the national rate. Among males aged older than 24 years, Hispanic/Latino males account for the highest percentage (40%) of diagnoses attributed to male-to-male sexual contact, while Hispanic/Latino females have a diagnosis rate of 6.7 per 100,000. These statistics reflect not individual failures but rather the impact of structural inequities, cultural barriers, and systemic exclusion.
Men Who Have Sex with Men: At the Epicenter
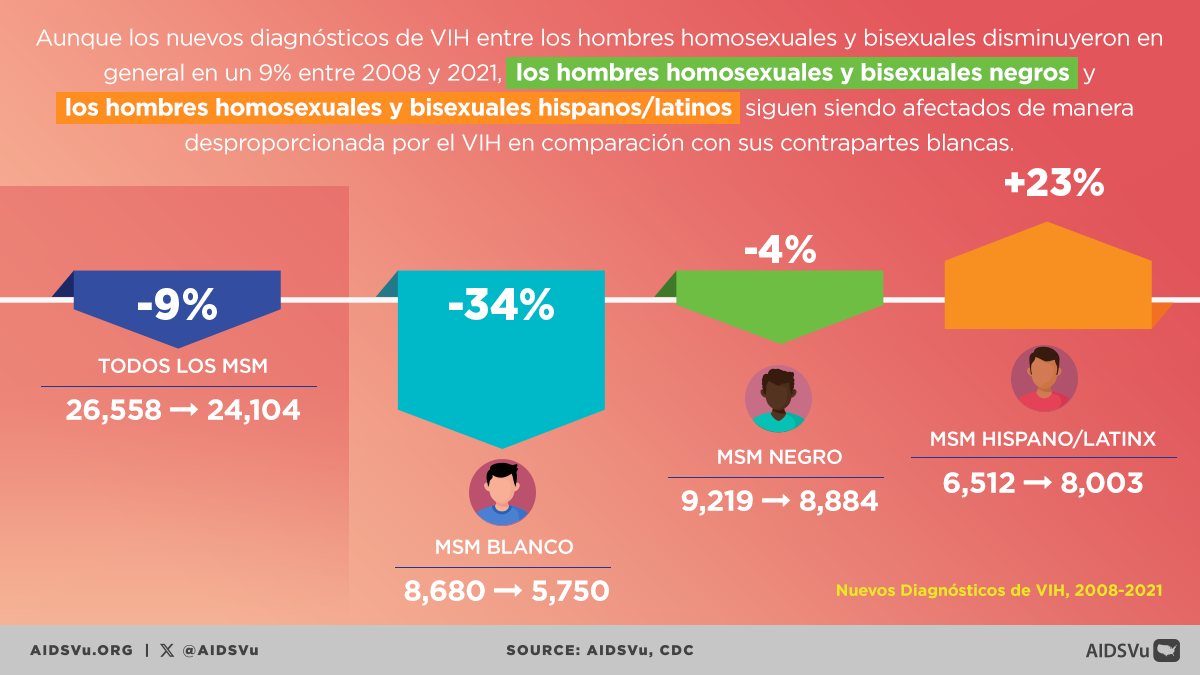
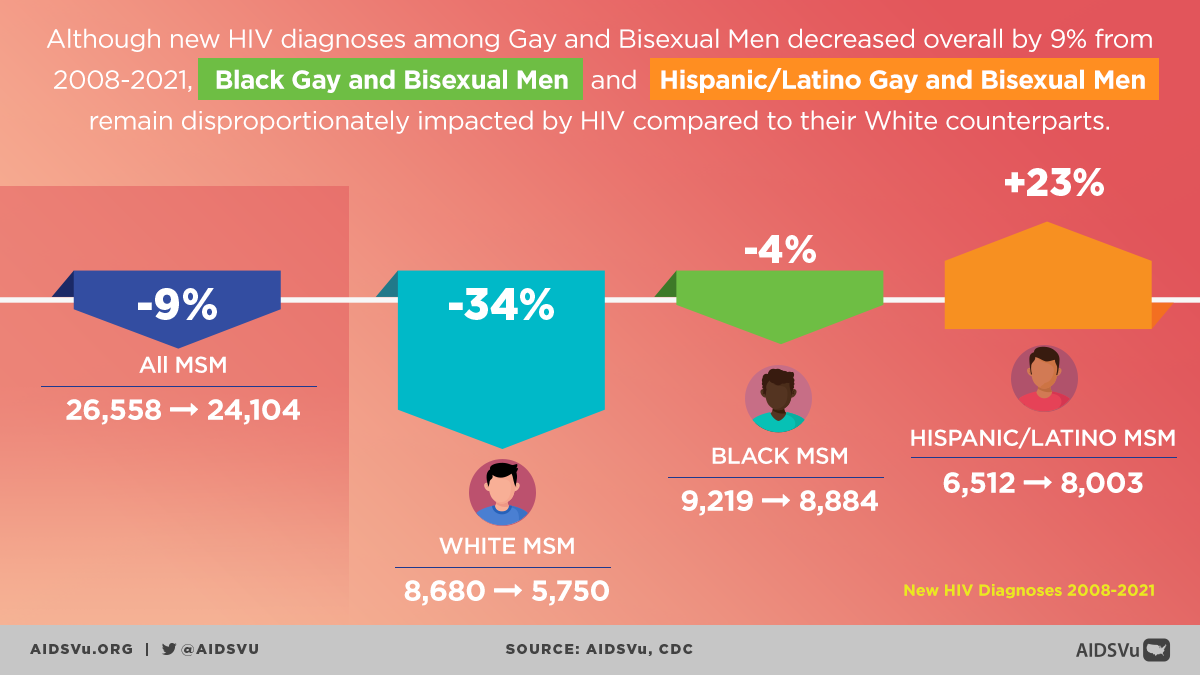
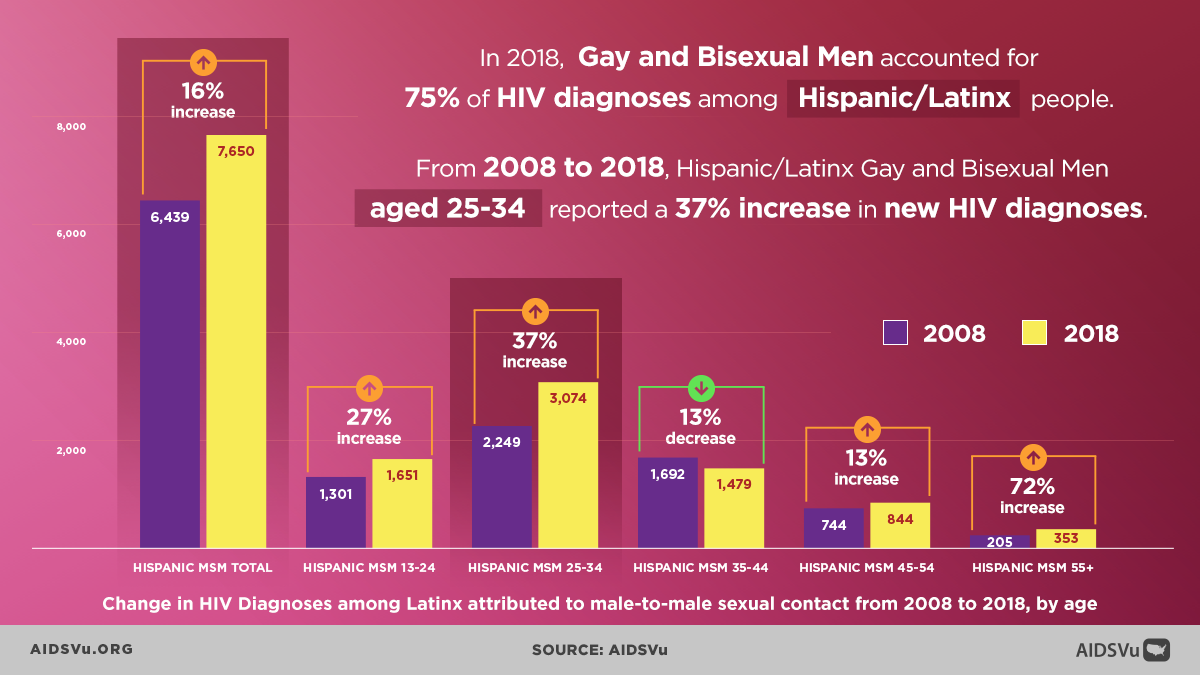
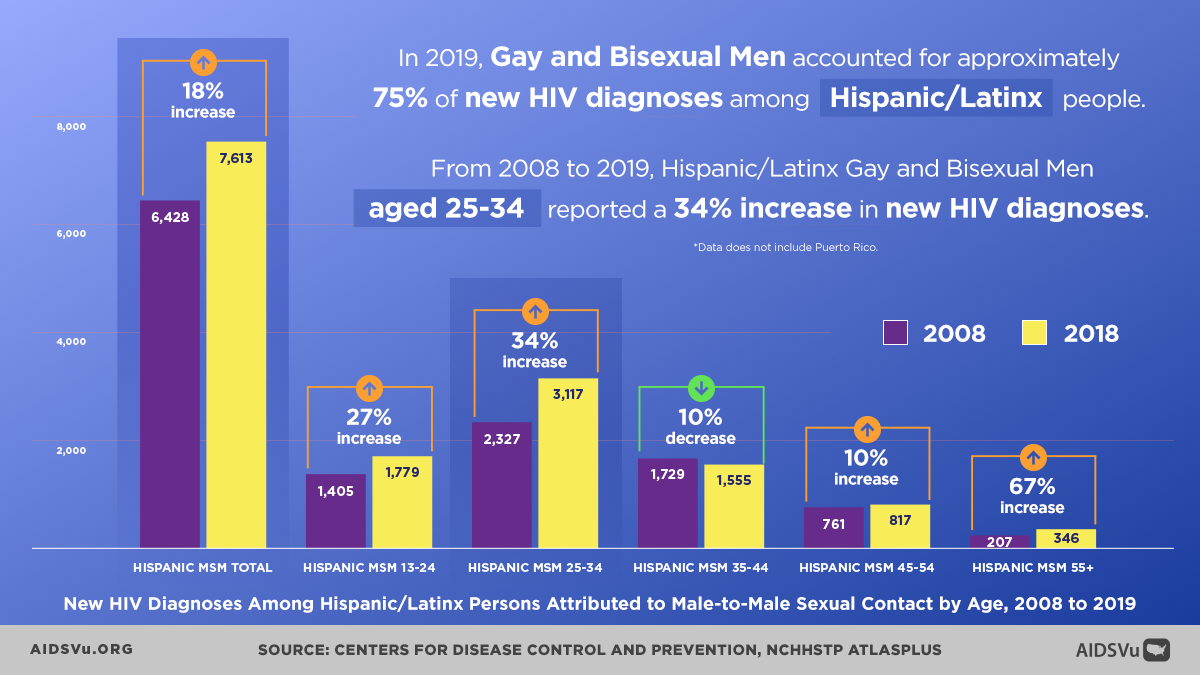
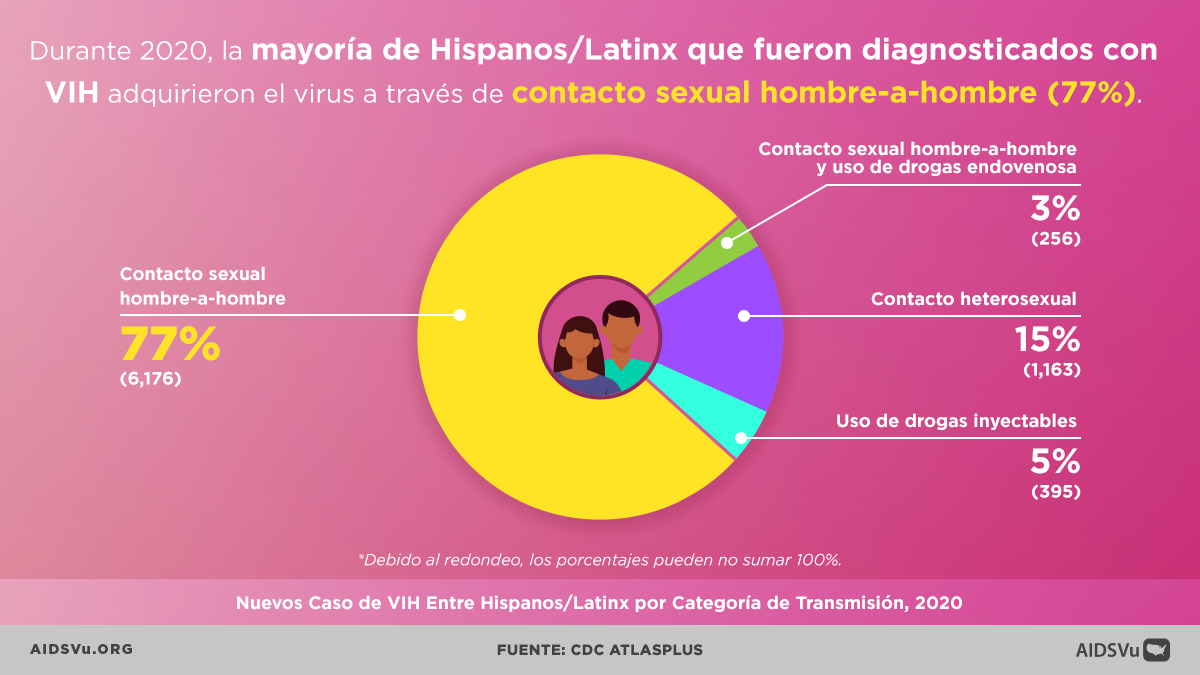
Hispanic/Latino men who have sex with men (MSM) represent the population most heavily affected by HIV within Hispanic/Latinx/Latine communities. In 2022, Hispanic/Latino MSM accounted for 37% of all new HIV diagnoses among men and now represent 39% of estimated new HIV infections among all MSM nationally.
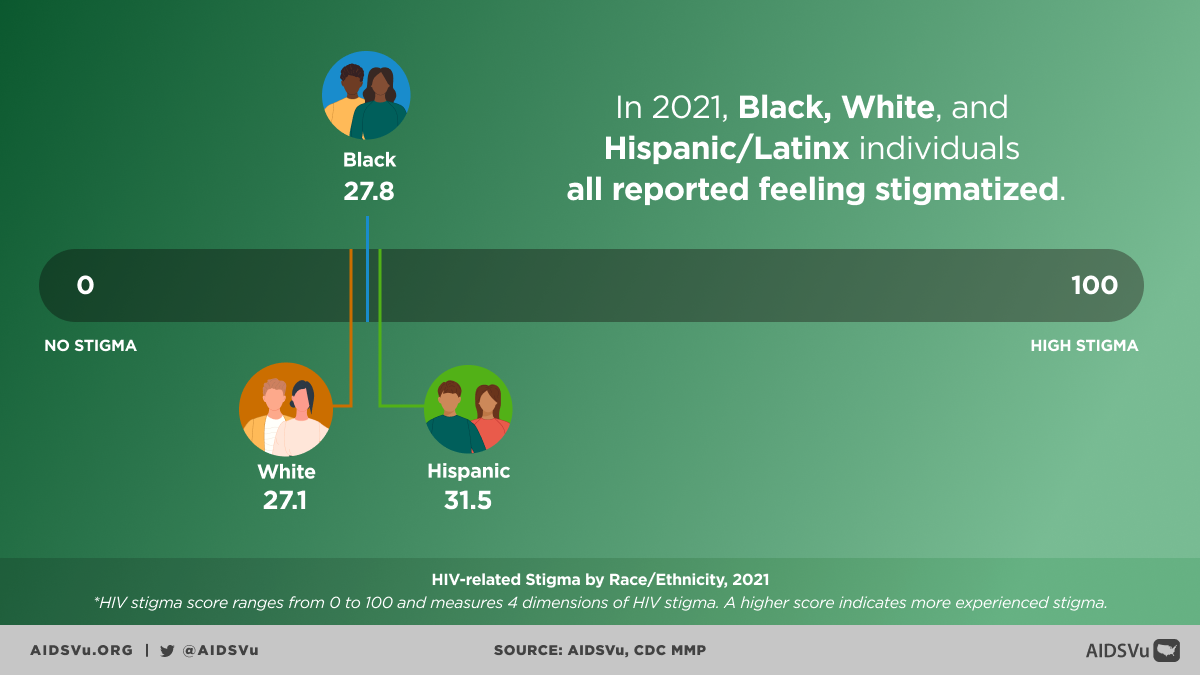
The persistence of high transmission rates among Hispanic/Latino MSM reflects the intersection of multiple barriers, including discrimination, social rejection, economic marginalization, and limited access to culturally competent healthcare services. Stigma related to homosexuality and bisexuality within some Hispanic/Latinx/Latine communities can create environments where men have difficulty accessing HIV prevention information or feel unable to disclose their sexual orientation to healthcare providers.
However, Hispanic/Latino MSM communities have also created vibrant support networks, advocacy organizations, and cultural expressions that provide resilience and resources for HIV prevention and care.
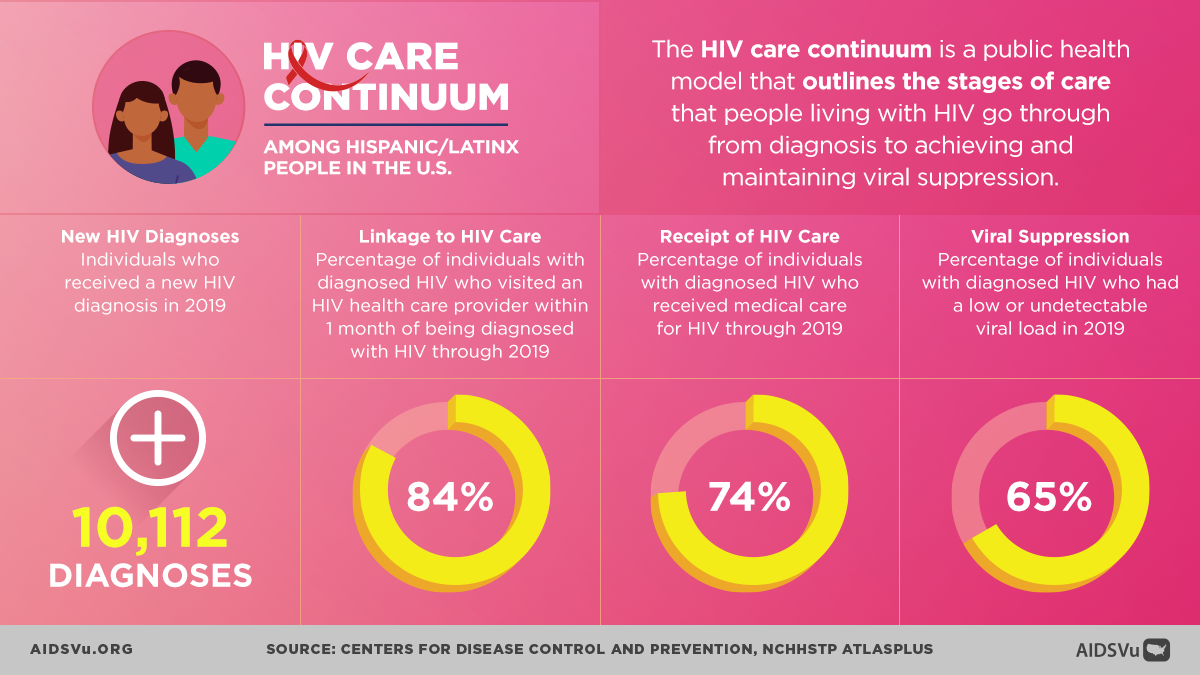
Late Diagnosis and Treatment Gaps
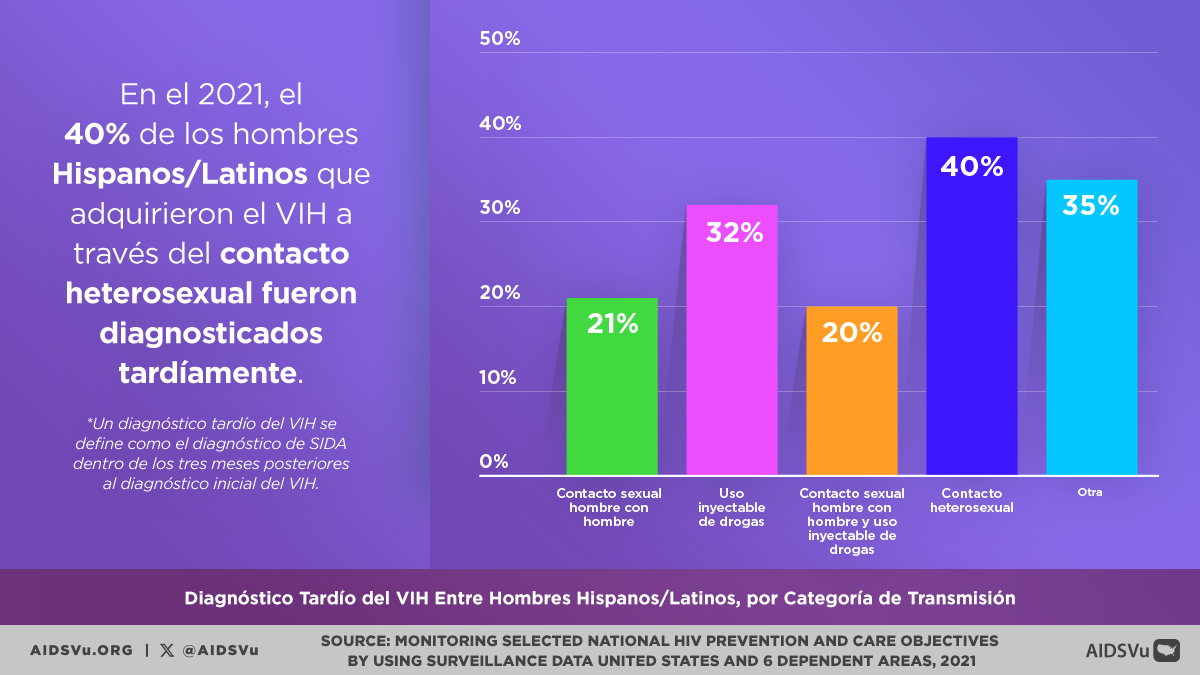
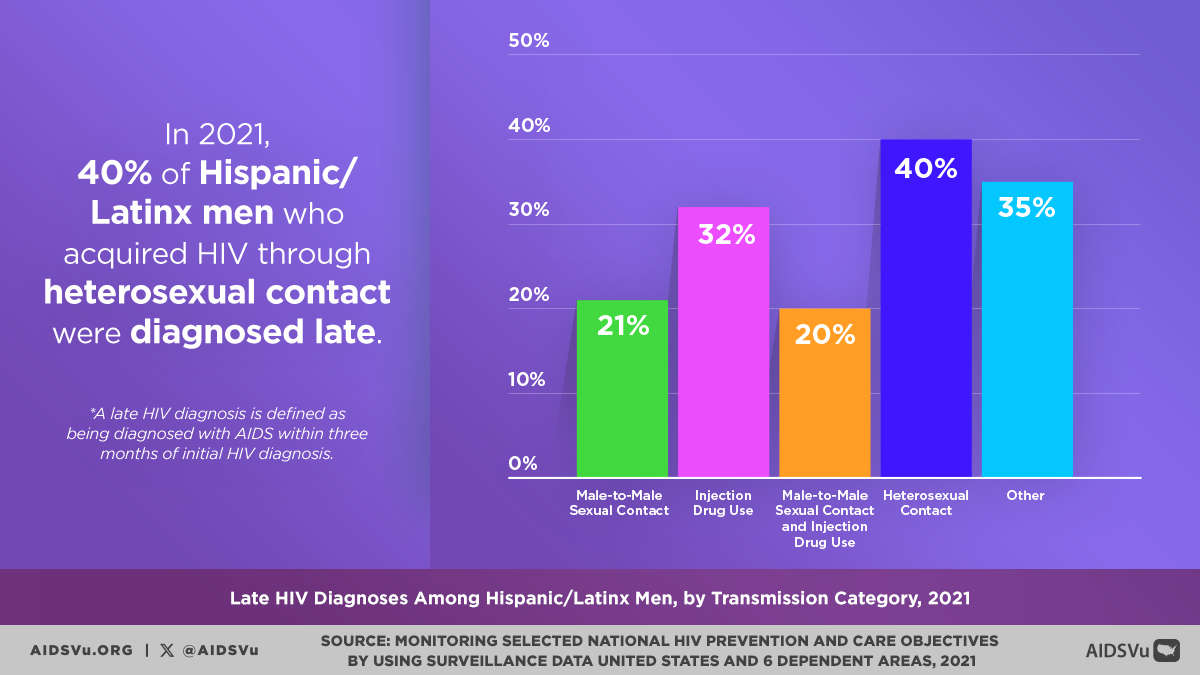
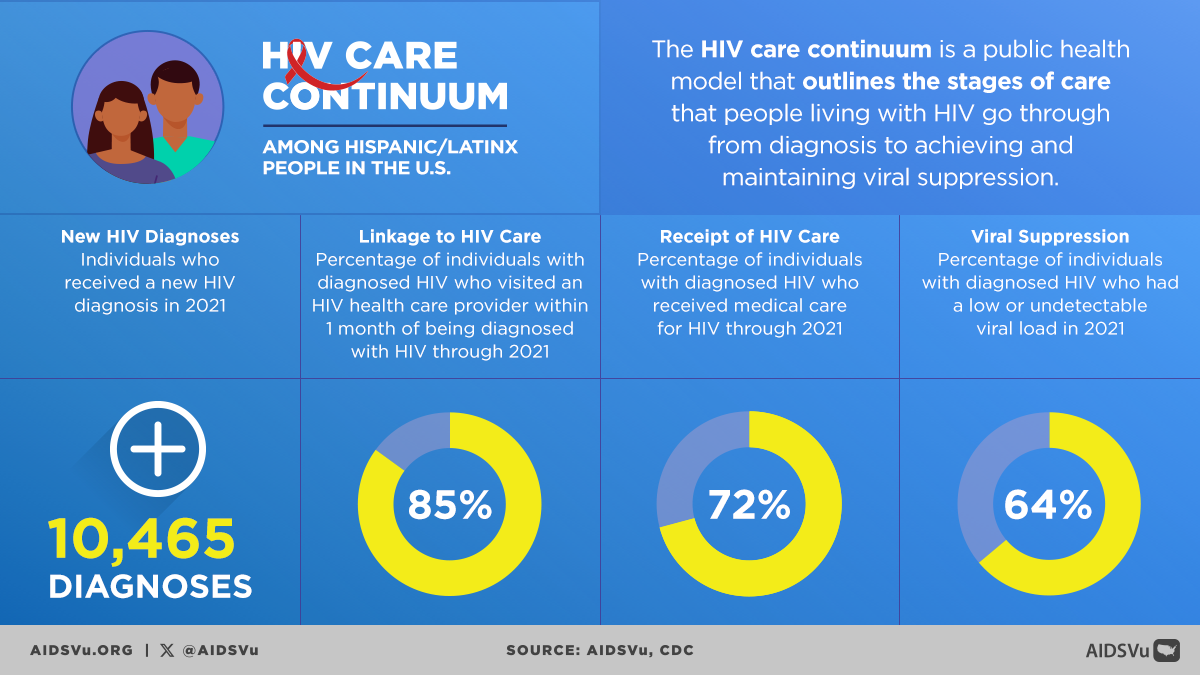
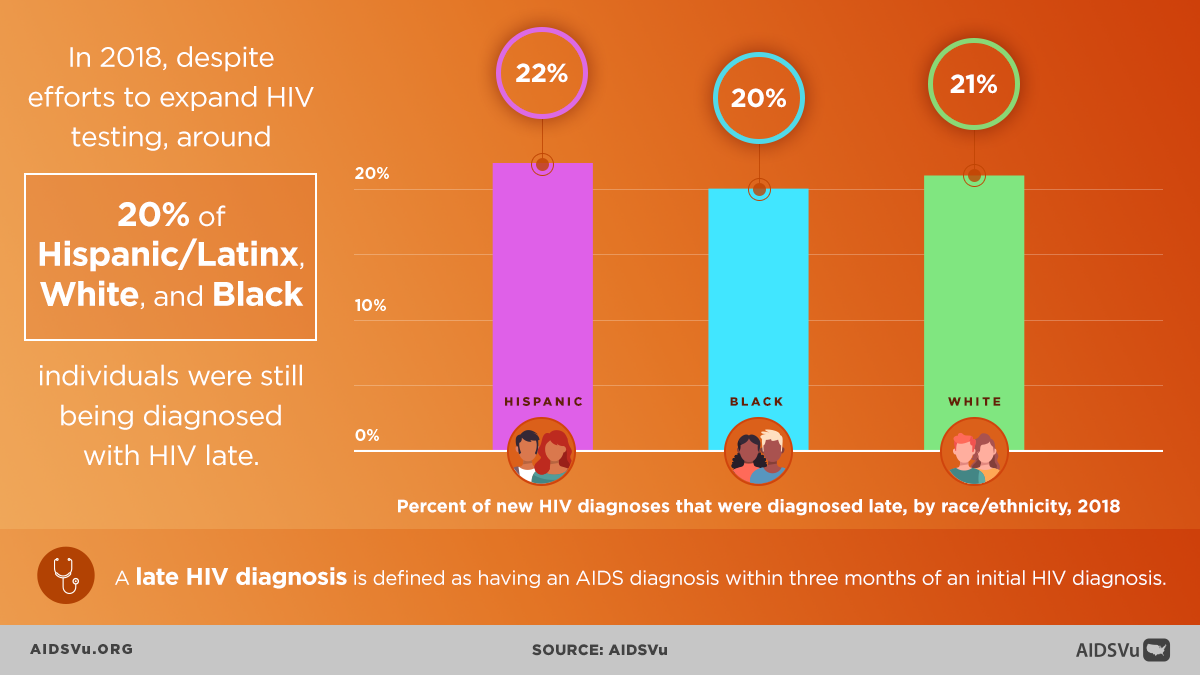
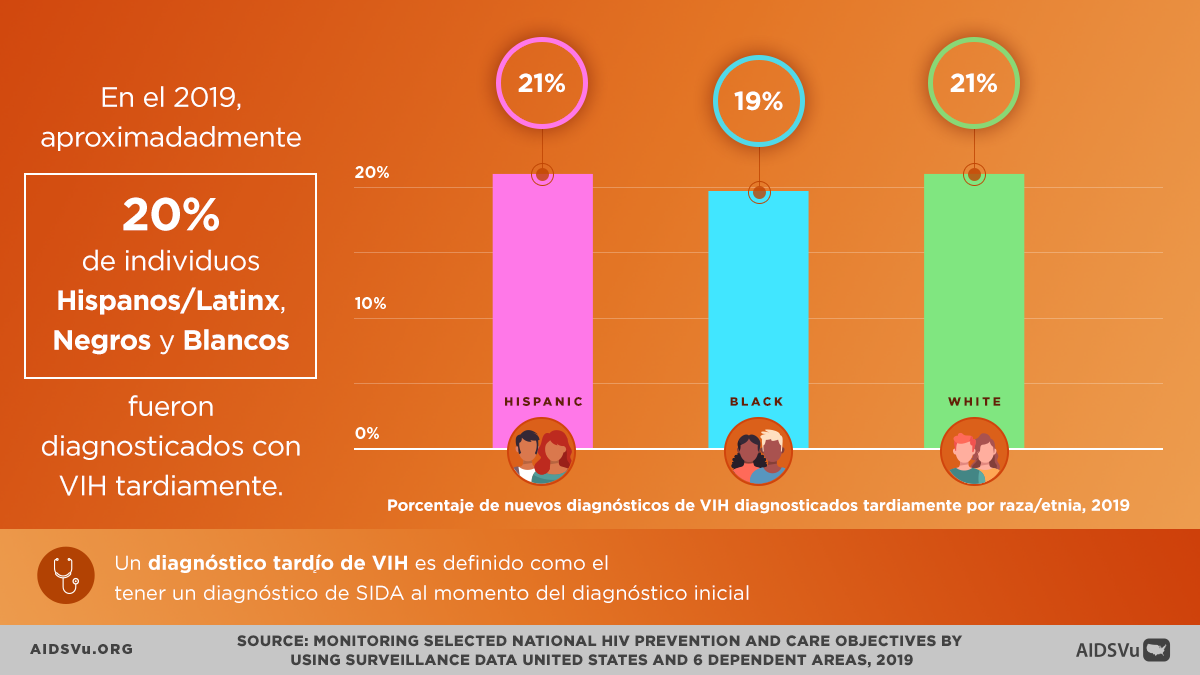
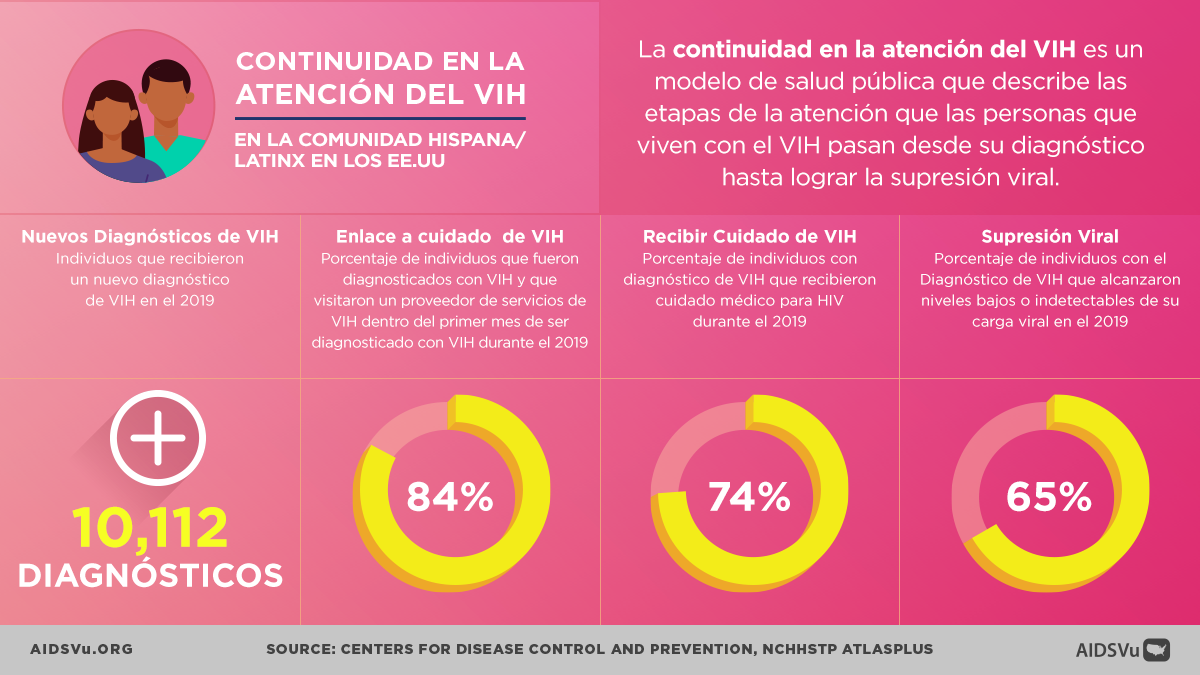
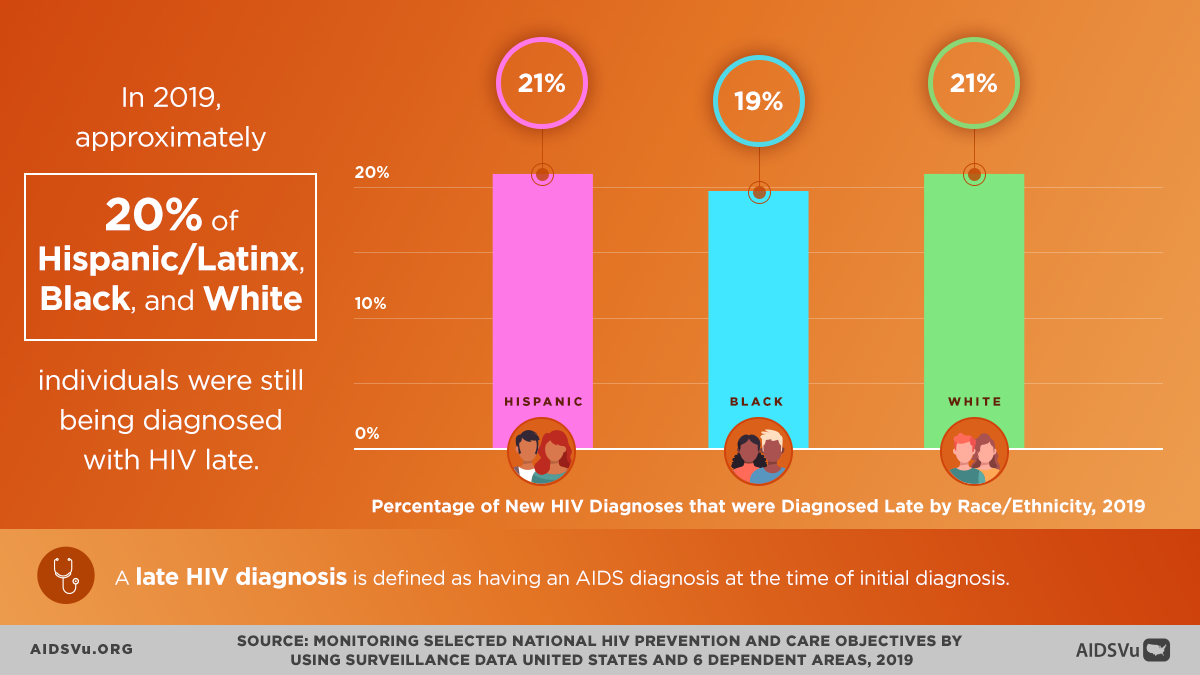
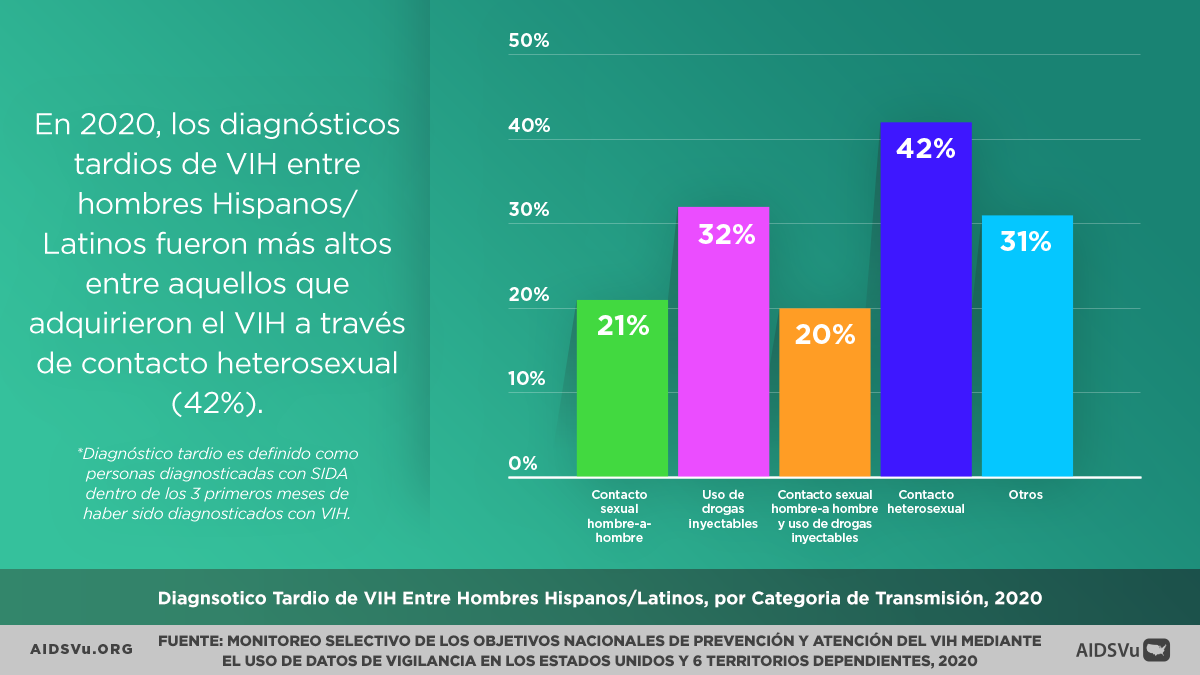
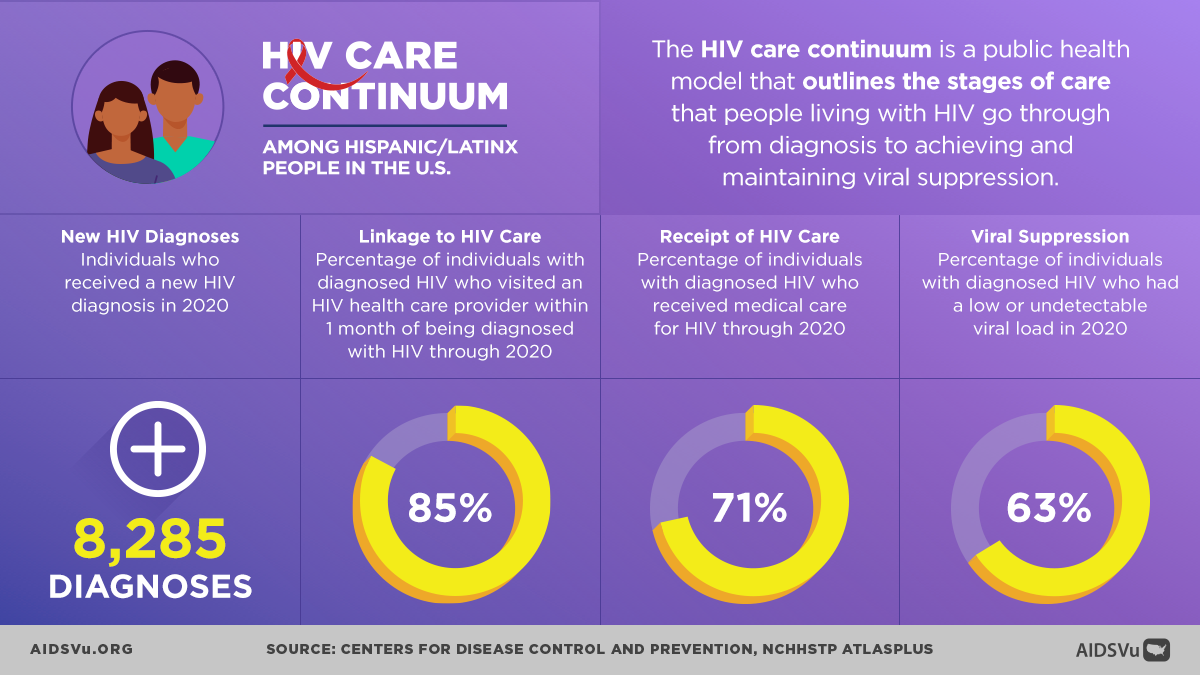
One of the most concerning aspects of the HIV epidemic among Hispanic/Latinx/Latine people is the pattern of late diagnosis and delayed entry into care. In 2022, 21% of new HIV diagnoses among Hispanic/Latinx/Latine people were classified as late diagnoses, meaning individuals were diagnosed with stage 3 HIV (AIDS) within three months of their initial HIV diagnosis.
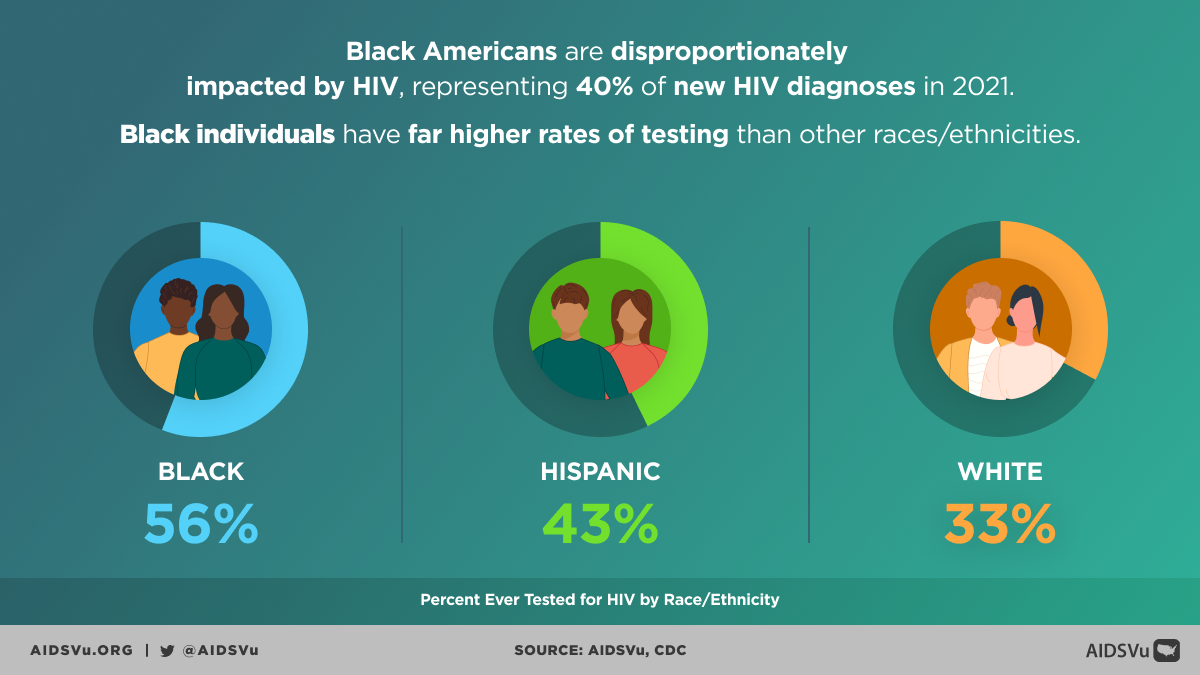
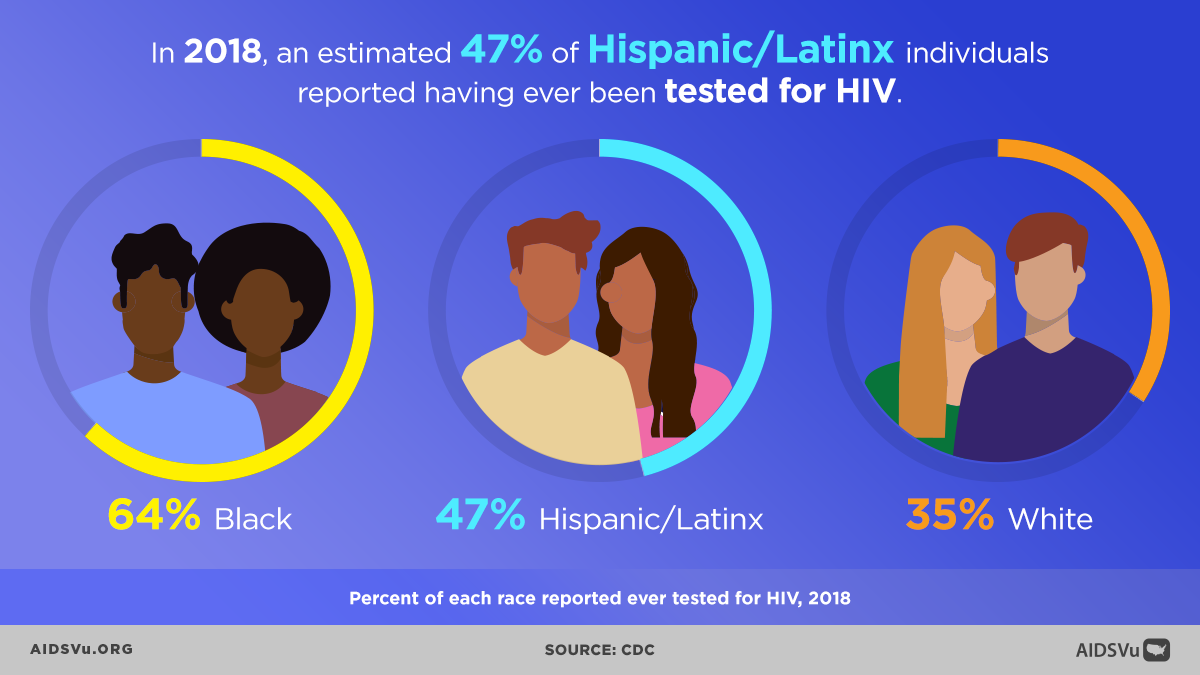
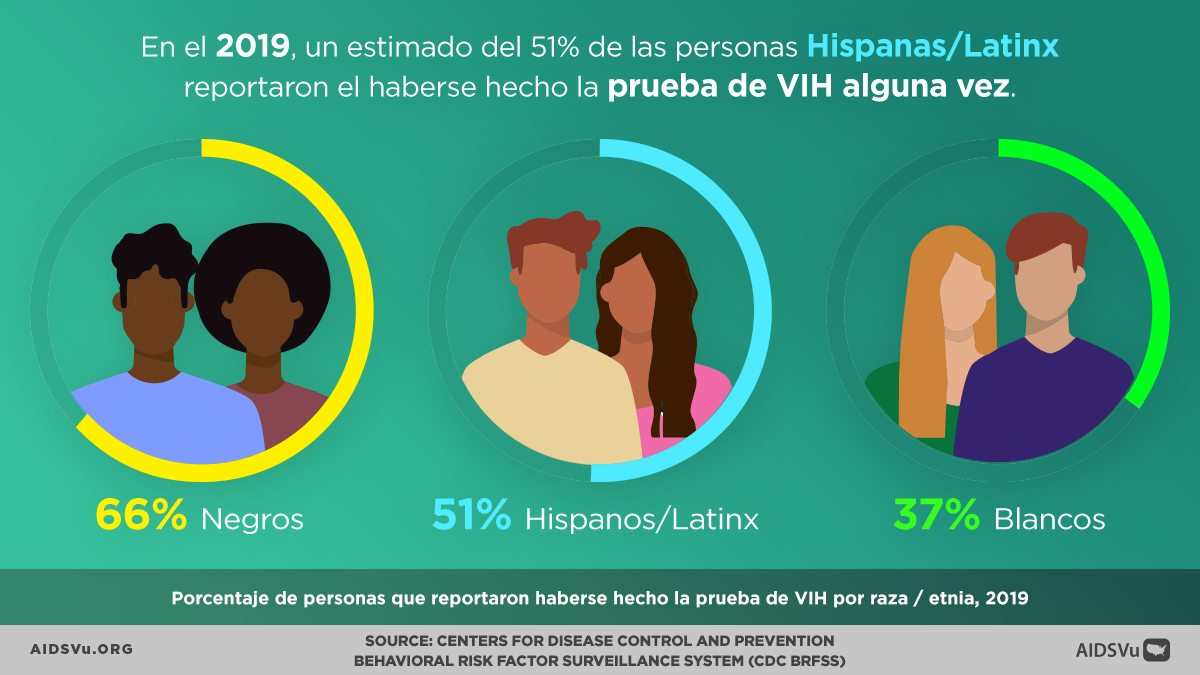
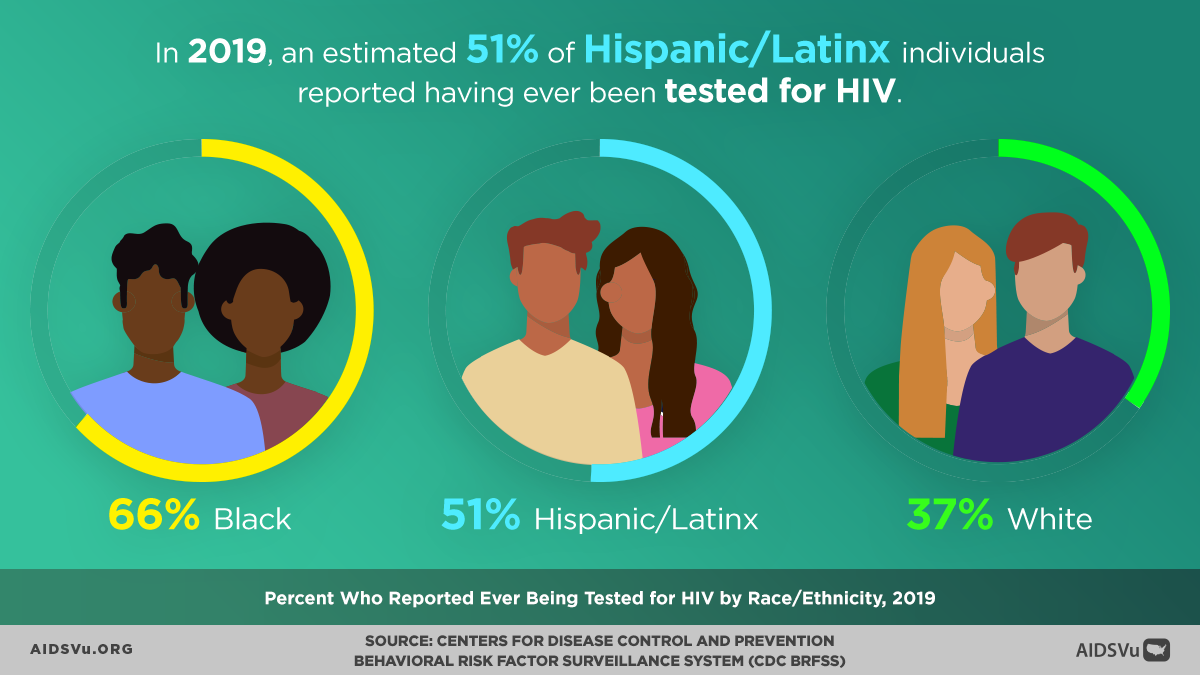
Additionally, only an estimated 45% of Hispanic/Latinx/Latine individuals reported ever being tested for HIV in 2022, significantly lower than testing rates in other populations. This low testing rate reflects both individual barriers to accessing testing and systemic failures to reach Hispanic/Latinx/Latine communities with culturally appropriate testing programs.
Late HIV diagnosis has serious consequences for both individual health outcomes and community transmission prevention, as people with undiagnosed HIV may unknowingly transmit the virus to others, particularly during acute infection when viral loads are highest.
Beyond the Map
AIDSVu offers tools and resources beyond the HIV map that provide users with a deeper understanding of the HIV epidemic, its socioeconomic-driving factors, and services available at the community level.
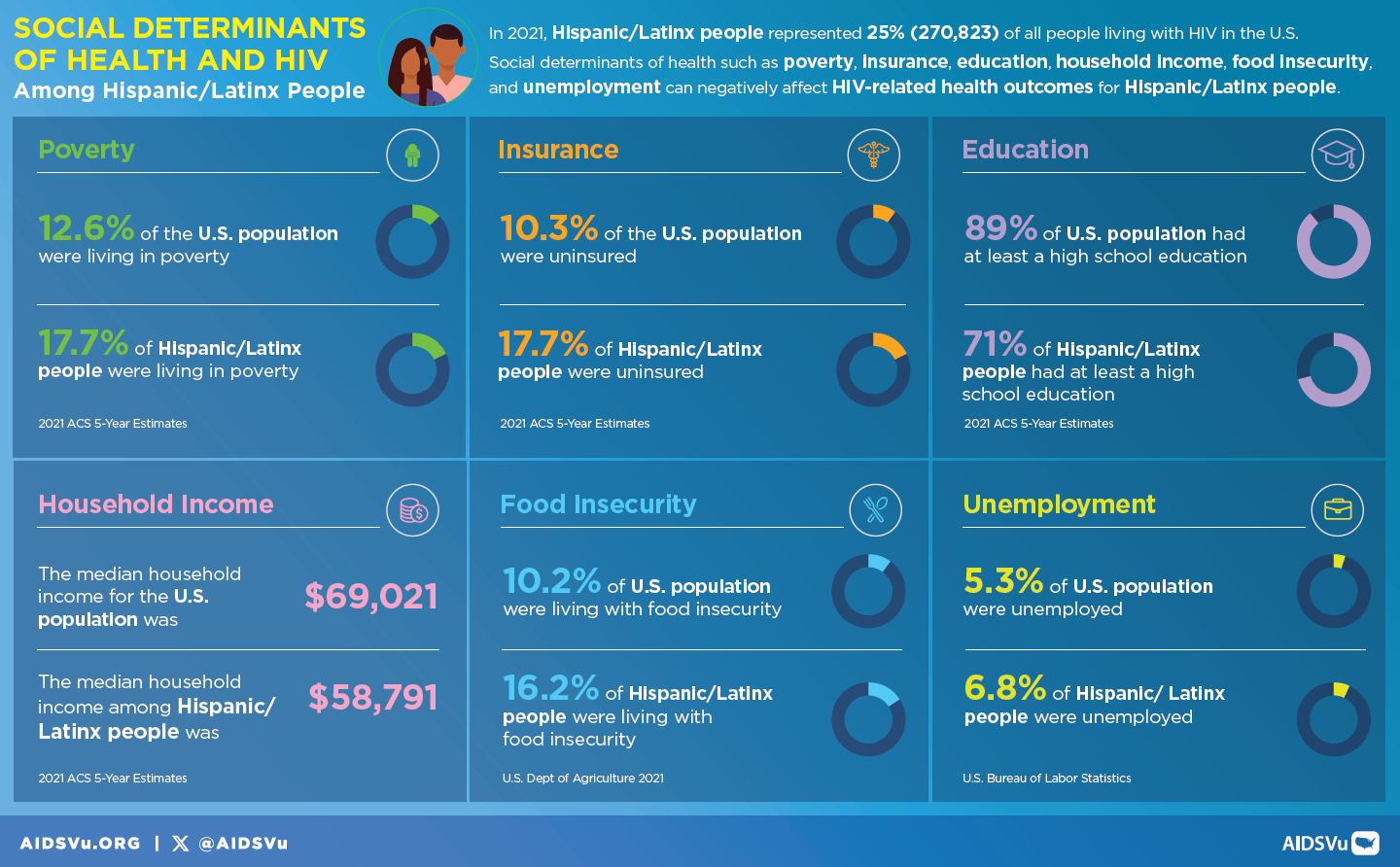
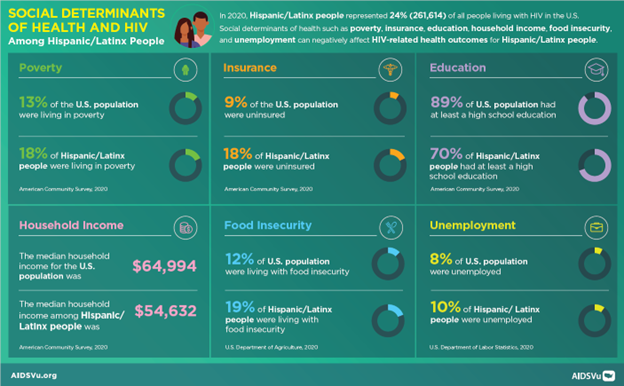
Social Determinants of Health
See how HIV prevalence is related to poverty, high school education, median household income, etc.
Learn MoreFind Services
Use the testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services locators to find critical HIV/AIDS services near you.
Learn MoreLocal Data
View city and state profiles with local HIV/AIDS statistics, national comparison charts, and local resources.
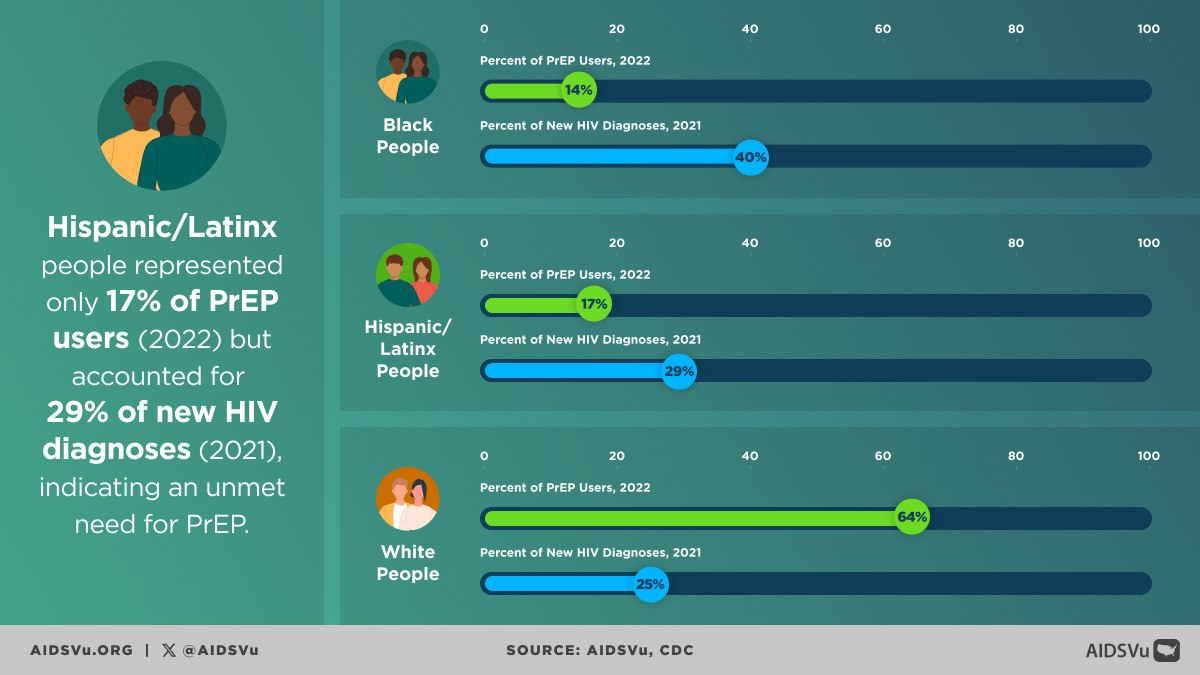
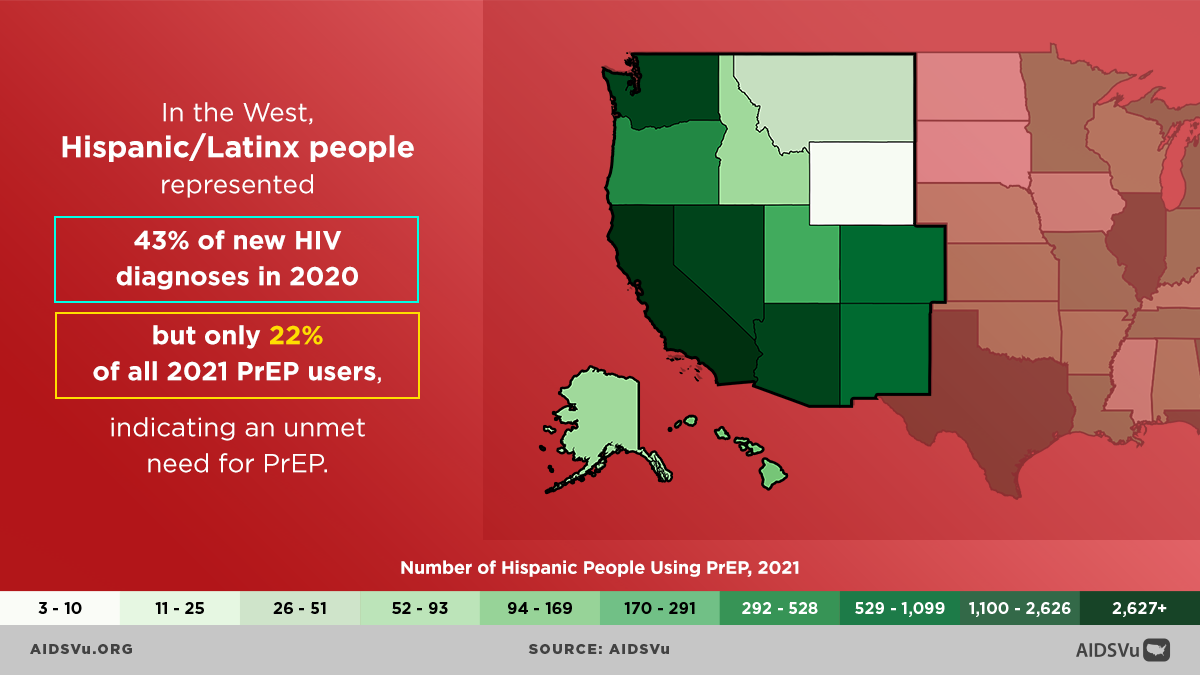
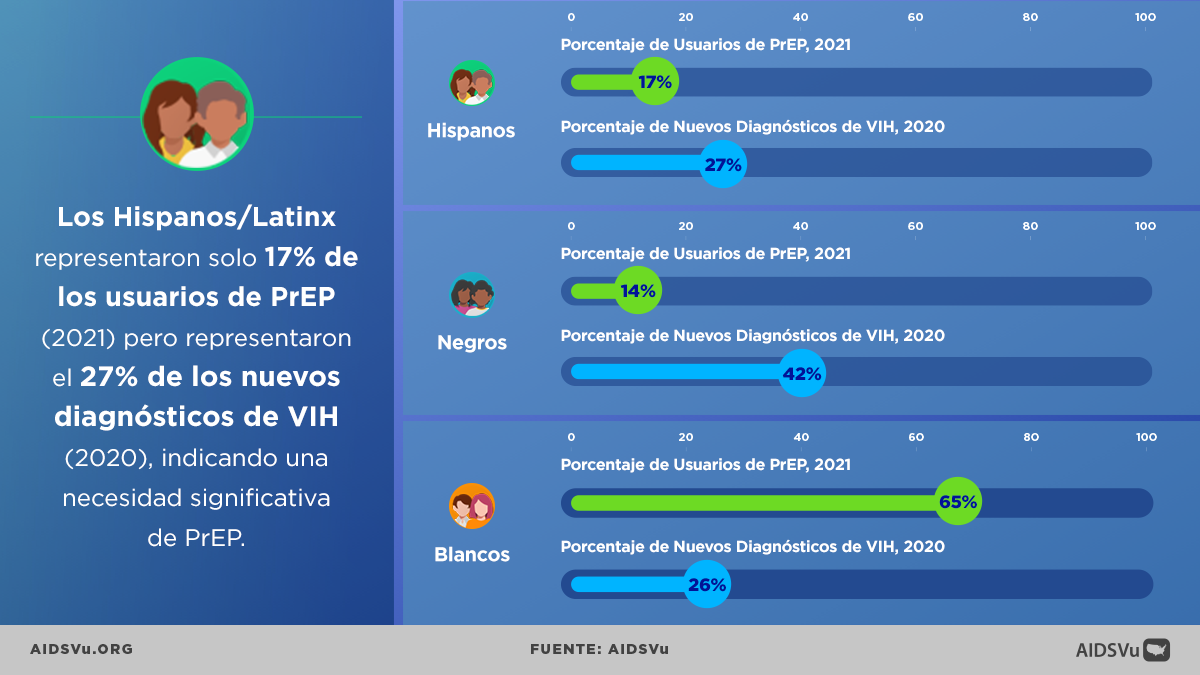
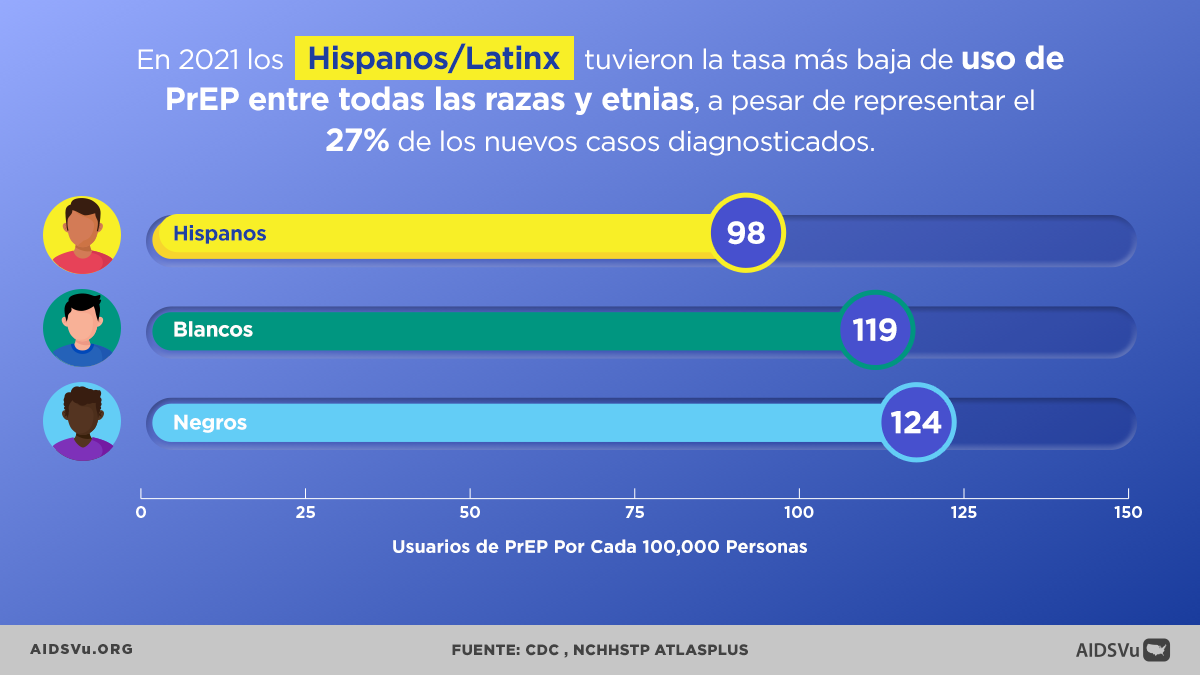
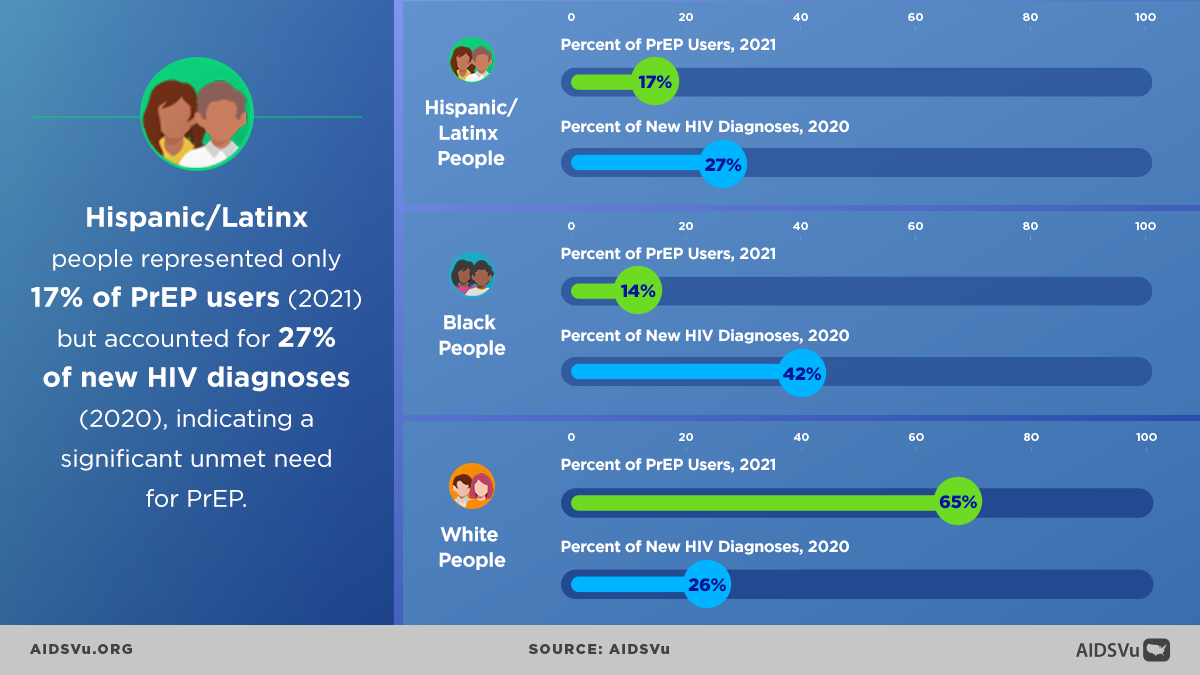
Learn MoreThe Prevention Gap: PrEP Access and Utilization
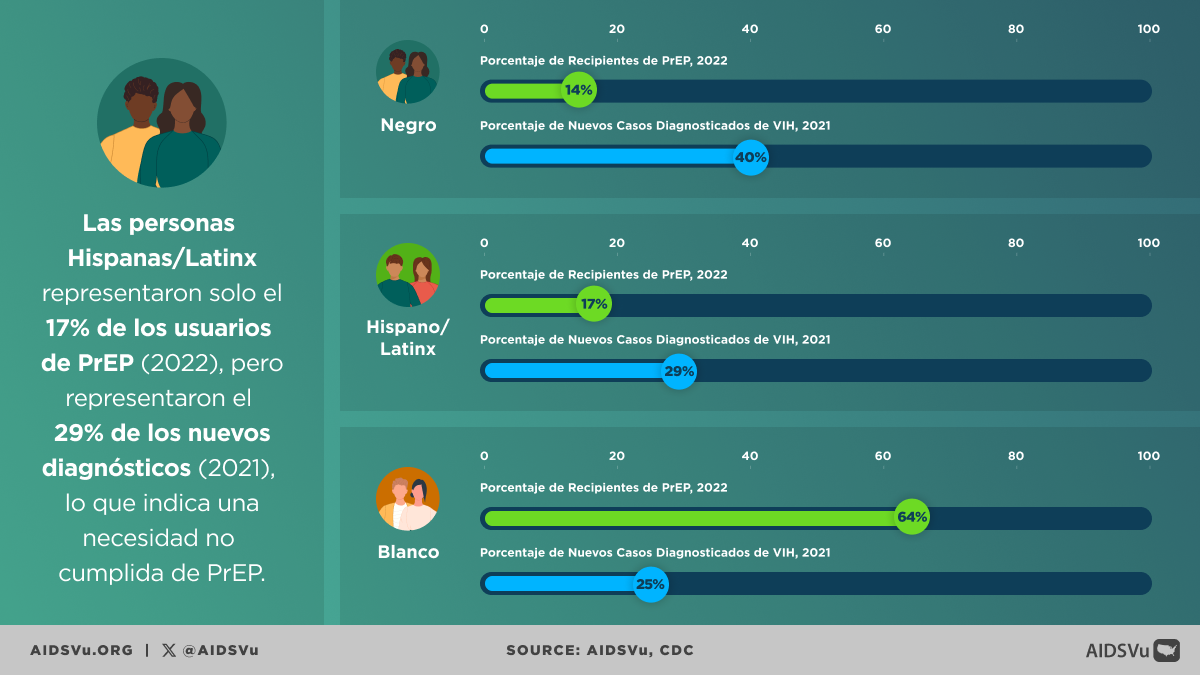
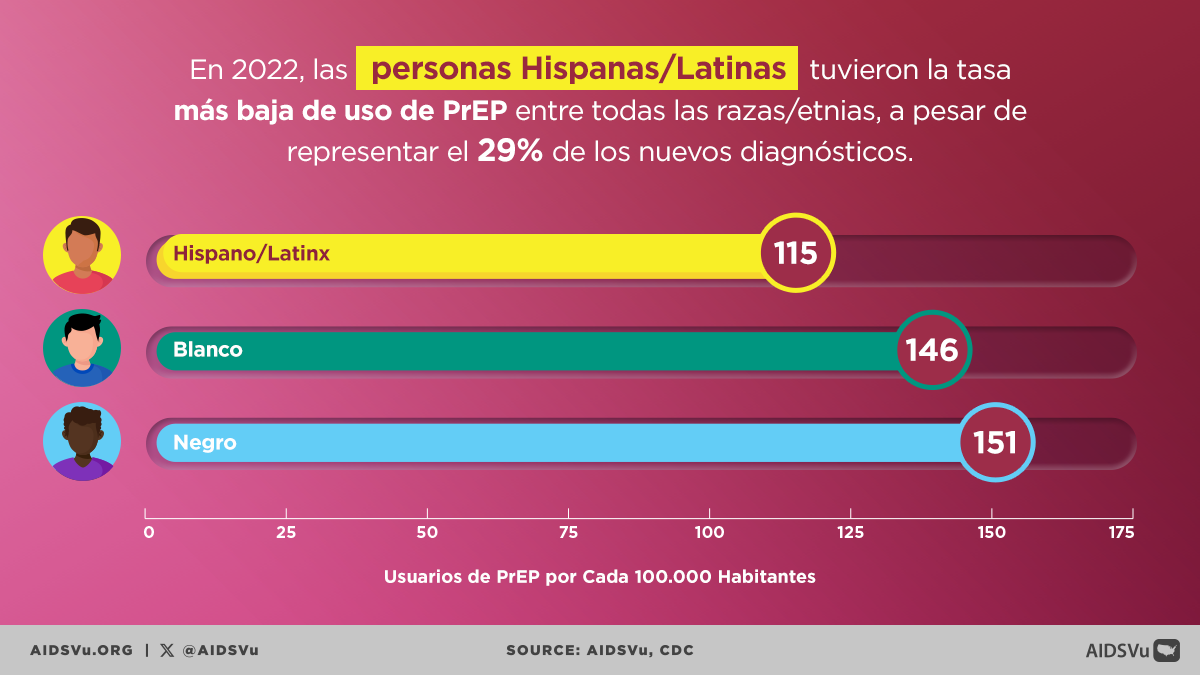
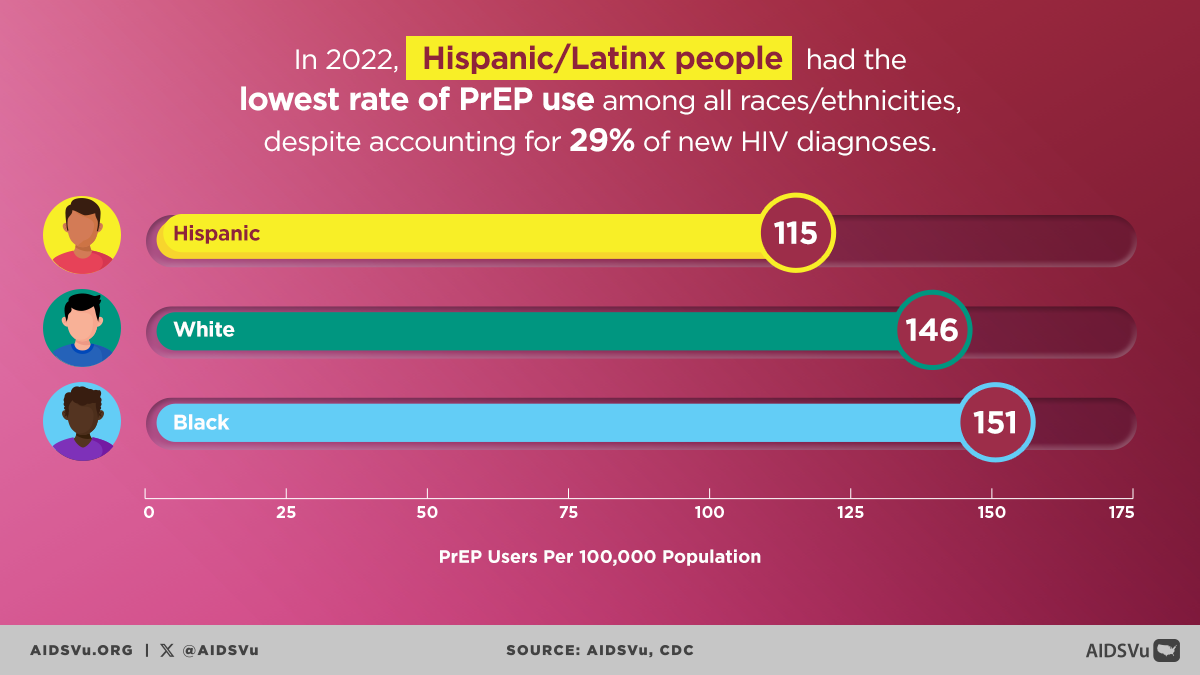
Pre-exposure prophylaxis (PrEP) represents one of the most significant advances in HIV prevention, yet PrEP uptake among Hispanic/Latinx/Latine people remains dramatically lower than their representation among new HIV diagnoses. In 2023, Hispanic/Latinx/Latine people had the lowest rate of PrEP use among all racial and ethnic groups despite accounting for 32% of new HIV diagnoses.
The PrEP-to-Need Ratio among Hispanic/Latinx/Latine people is four times lower than for white individuals, demonstrating substantially higher unmet need. These disparities vary by geographic region, ranging from 3 to 6 times lower than white individuals depending on the area.
Multiple barriers contribute to low PrEP uptake, including limited awareness of PrEP availability, concerns about side effects, difficulty accessing PrEP-prescribing providers, cost and insurance concerns, and immigration-related fears. Cultural and linguistic barriers also play important roles, as many healthcare providers lack training in culturally competent PrEP counseling.
Healthcare System Challenges and Opportunities
The healthcare system presents both barriers and opportunities for improving HIV outcomes. Many healthcare settings lack cultural competency, language services, and structural accommodations needed to effectively serve Hispanic/Latinx/Latine patients. Provider bias can create unwelcoming environments that discourage people from seeking care.
However, Federally Qualified Health Centers and community health centers often serve large numbers of Hispanic/Latinx/Latine patients and can be important sites for integrating HIV services with primary care. Integration with other healthcare that people already access—such as family planning, prenatal care, or chronic disease management—can help normalize HIV prevention and testing.
Mental Health and Social Support
Among Hispanic/Latinx/Latine people with diagnosed HIV, 23% reported needing but not receiving mental health services in 2022. The mental health impact reflects not only the challenges of living with HIV but also the intersection of HIV-related stigma with other forms of discrimination and marginalization.
Social determinants create additional challenges, including food insecurity that can interfere with medication adherence, housing instability that complicates HIV care, and employment discrimination that limits economic opportunities. However, Hispanic/Latinx/Latine communities also demonstrate significant strengths, including strong family and community networks and cultural traditions of care and support.
Community Response and Innovation
Hispanic/Latinx/Latine communities have developed innovative, culturally grounded approaches to HIV prevention and care. Community-based organizations have pioneered integrated approaches that address HIV within the context of other community needs, including immigration services, job training, and family support.
Peer support and navigation programs have proven particularly effective, providing culturally grounded support from people with shared experiences and cultural understanding. These programs help address language barriers, navigate complex systems, and provide emotional support that acknowledges participants’ cultural context.
Moving Forward: Comprehensive Solutions
Addressing HIV among Hispanic/Latinx/Latine people requires comprehensive approaches that acknowledge both the urgency of the epidemic and the complex factors driving HIV vulnerability. Critical priorities include expanding culturally competent healthcare services, supporting community-based prevention and care programs, addressing immigration-related barriers through policy advocacy, and investing in research that improves understanding of HIV within these diverse communities.
Success requires sustained commitment from healthcare providers, public health agencies, community organizations, and Hispanic/Latinx/Latine communities themselves, working together to create environments where all people can access the resources they need to prevent HIV and live healthy, fulfilling lives.
5 Ways to Use AIDSVu
Explore Maps
Explore the interactive map, customize your view, and easily print for presentations, grant applications, or other materials.
Learn MoreView Local Statistics
View local statistics for your city or state, and download high-impact data visualizations for your work
Learn MoreDownload Data
Download the datasets that inform AIDSVu’s visualizations for your own research and analysis
Learn MoreLocate Services
Use AIDSVu’s service locators to find HIV testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services near you
Learn MoreFor More Information
Learn more about the impact of HIV in Hispanic/Latinx/Latine communities with the following additional resources.