The South’s Disproportionate Burden
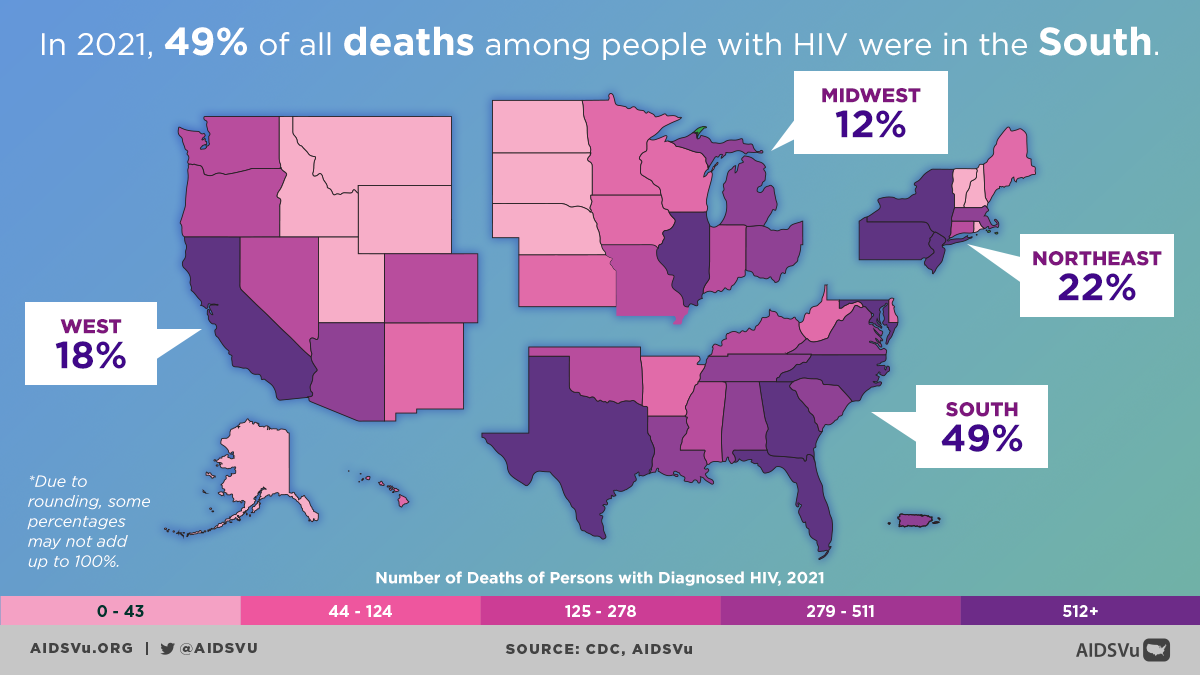
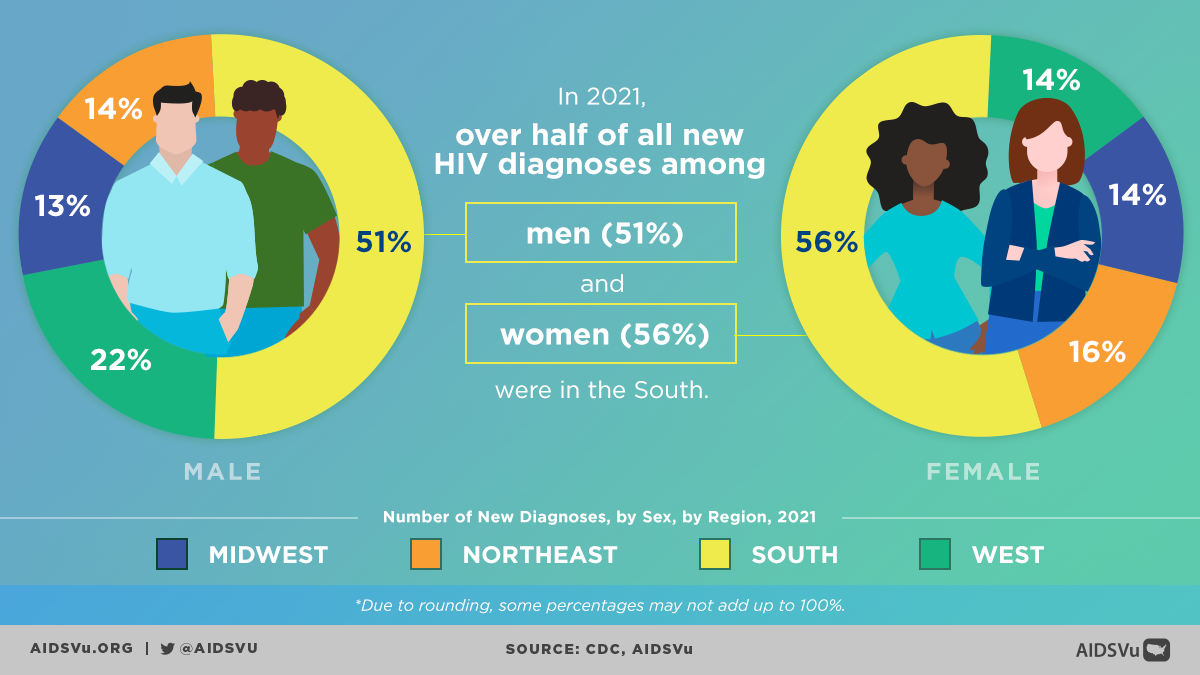
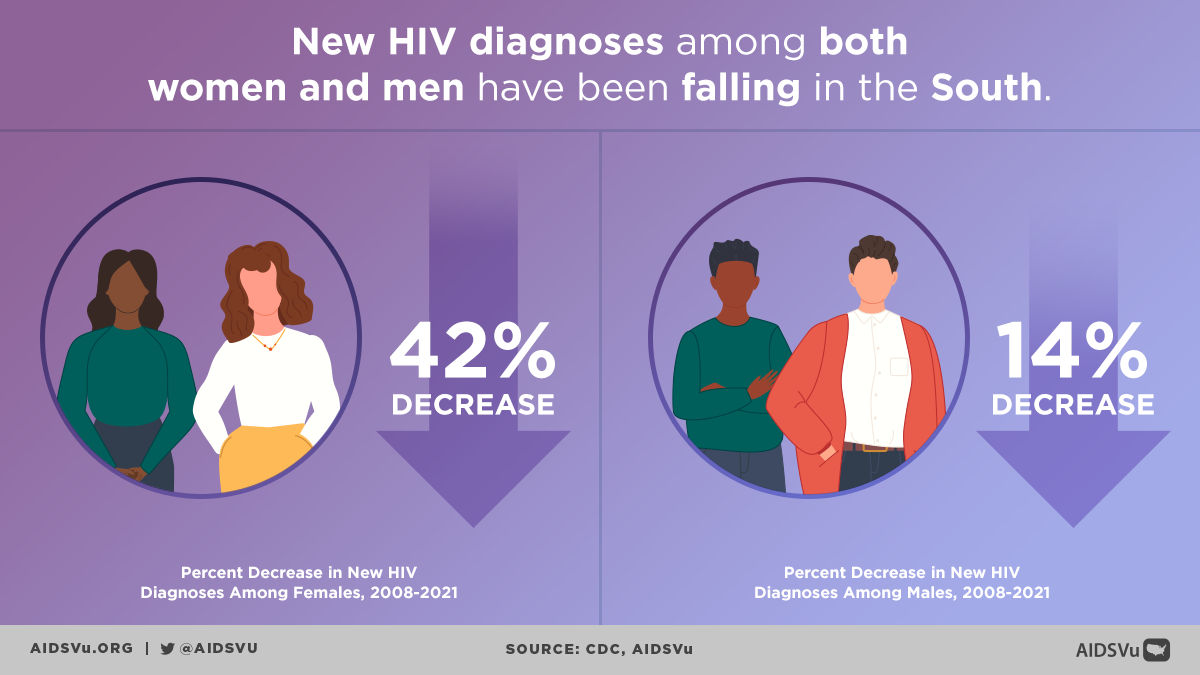
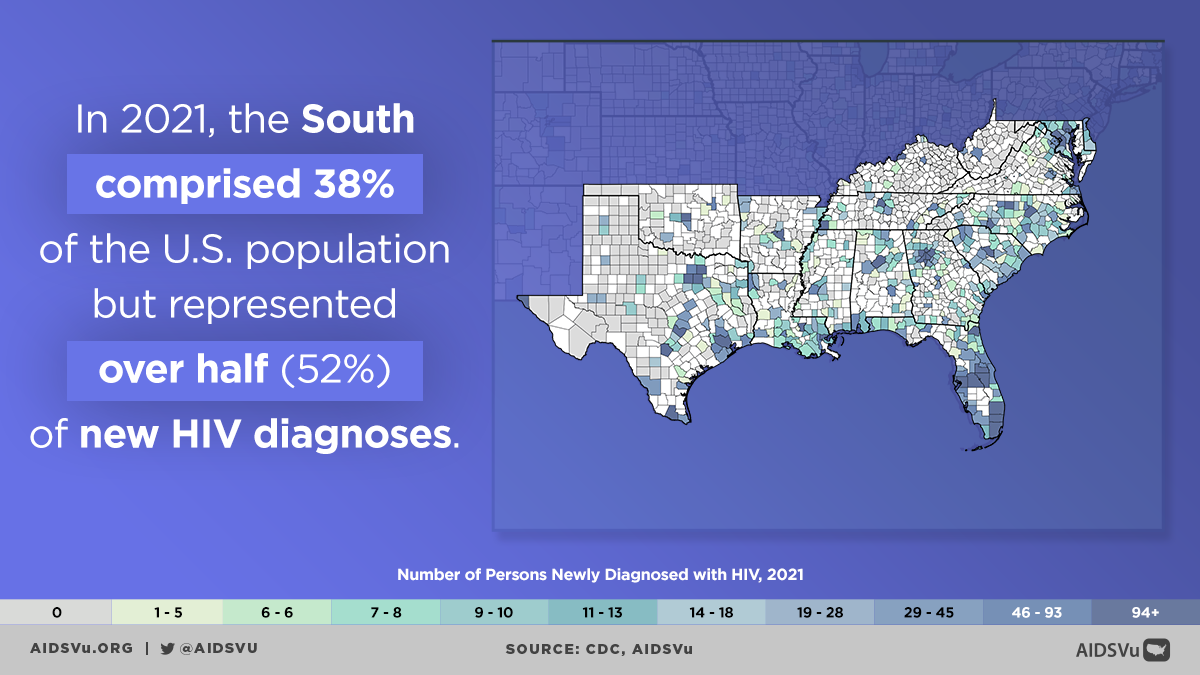
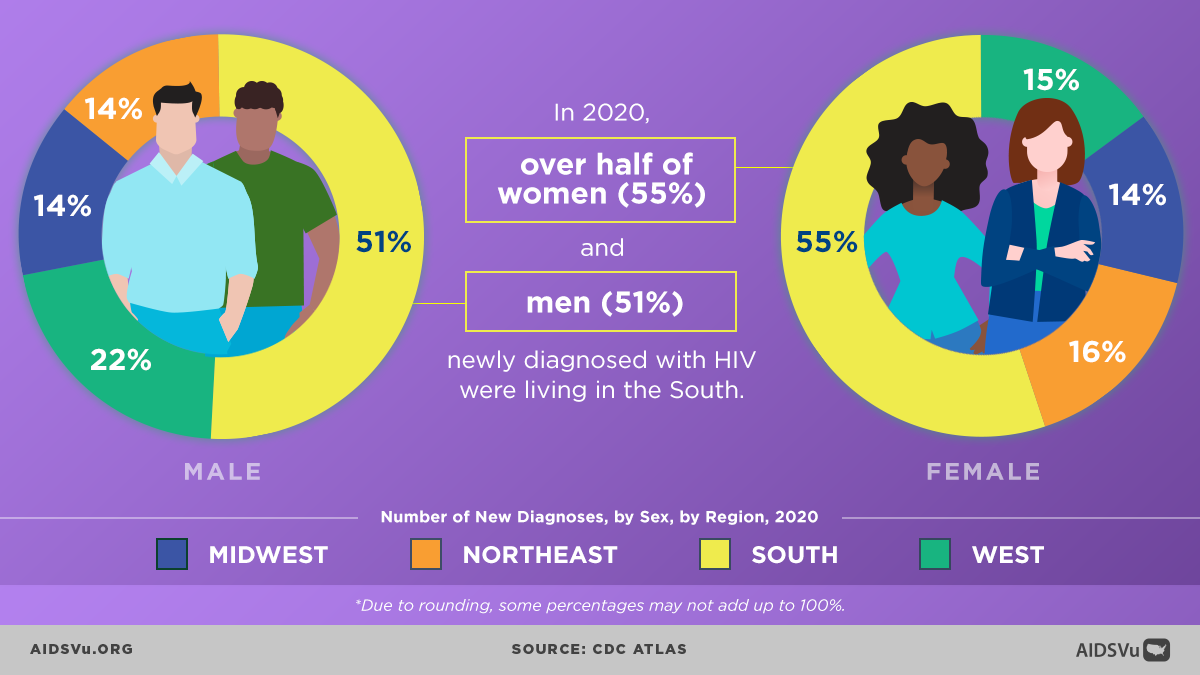
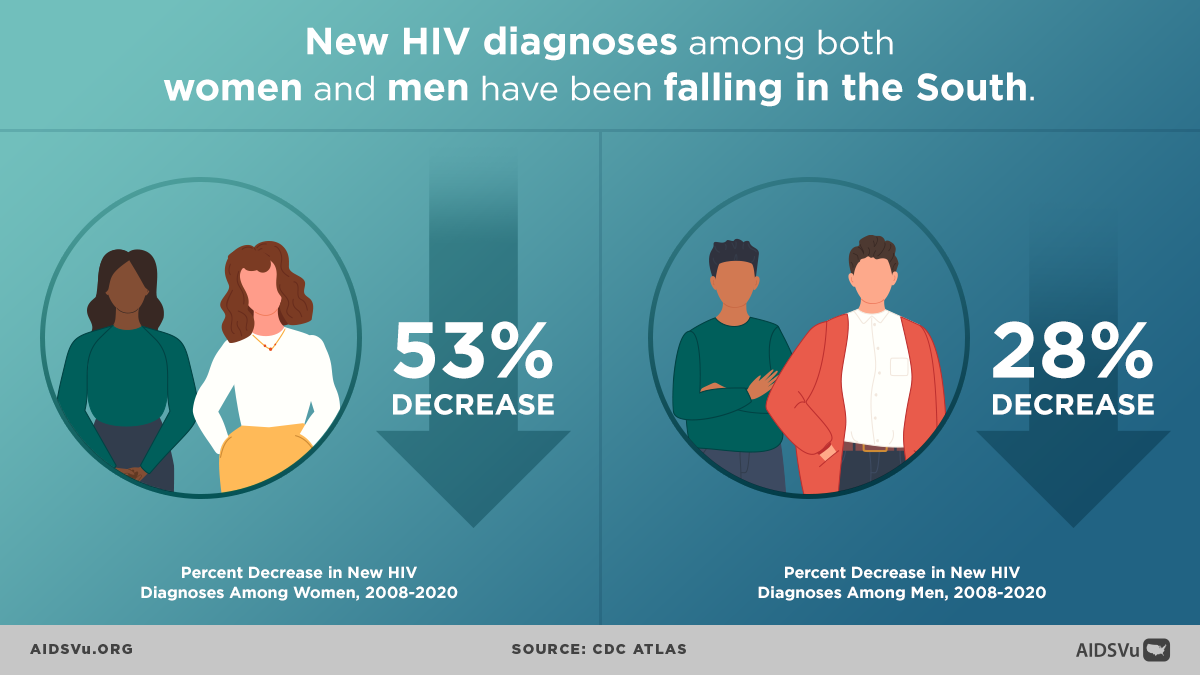
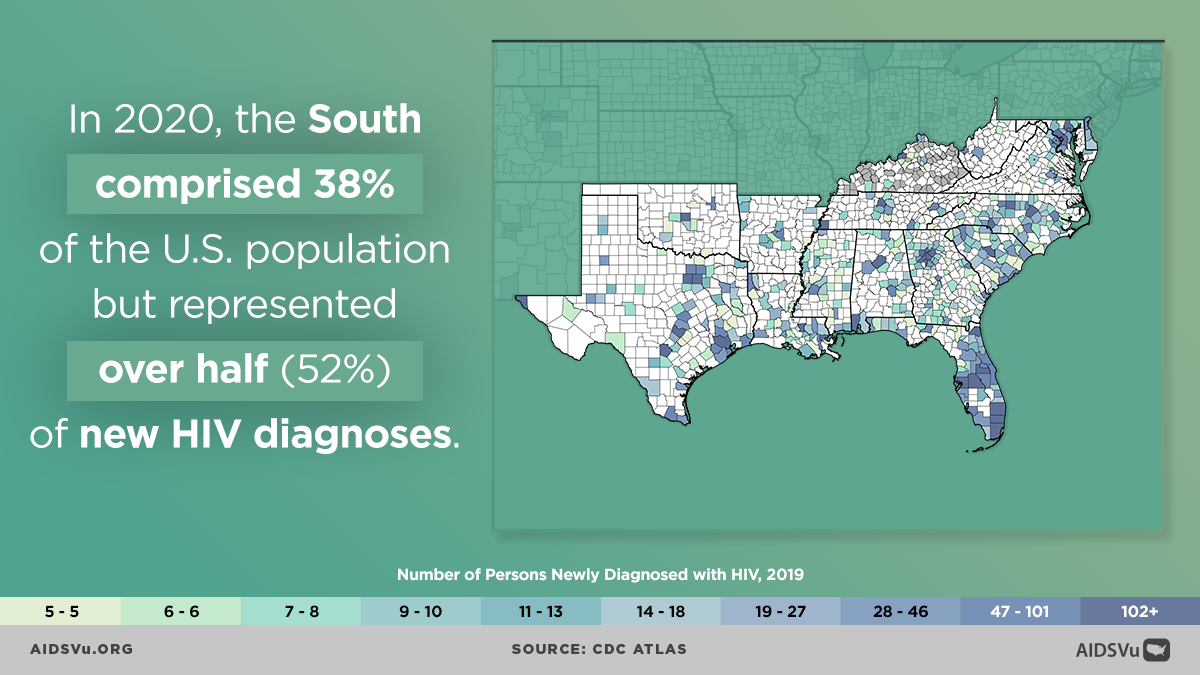
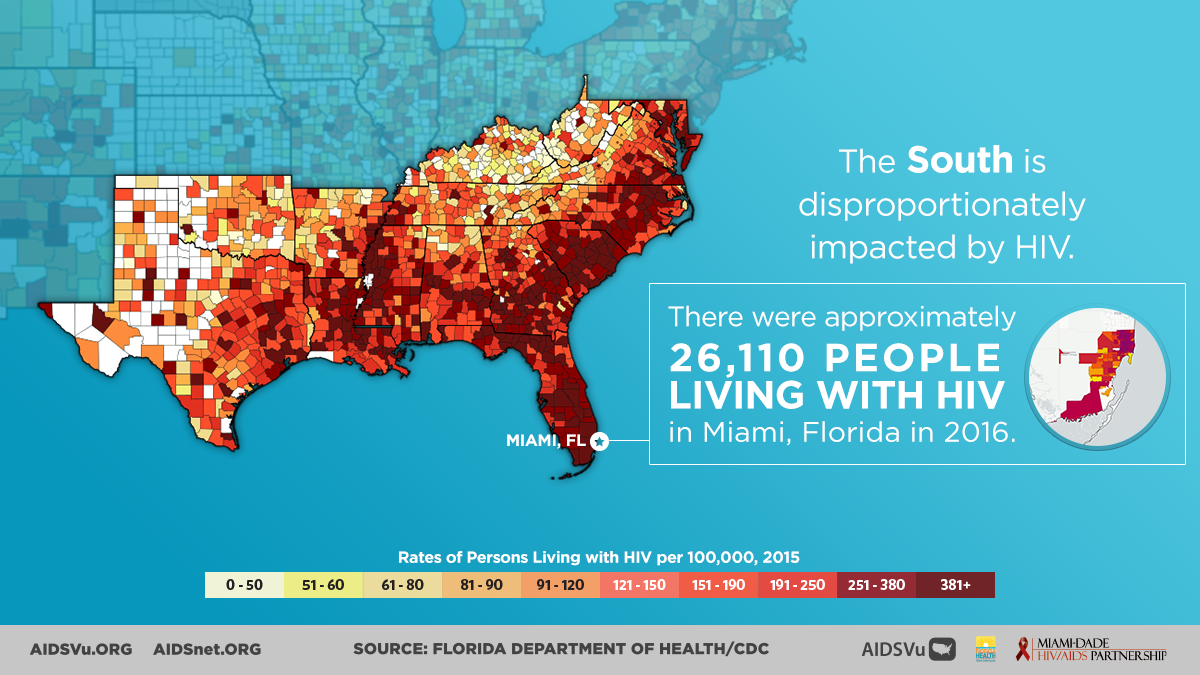
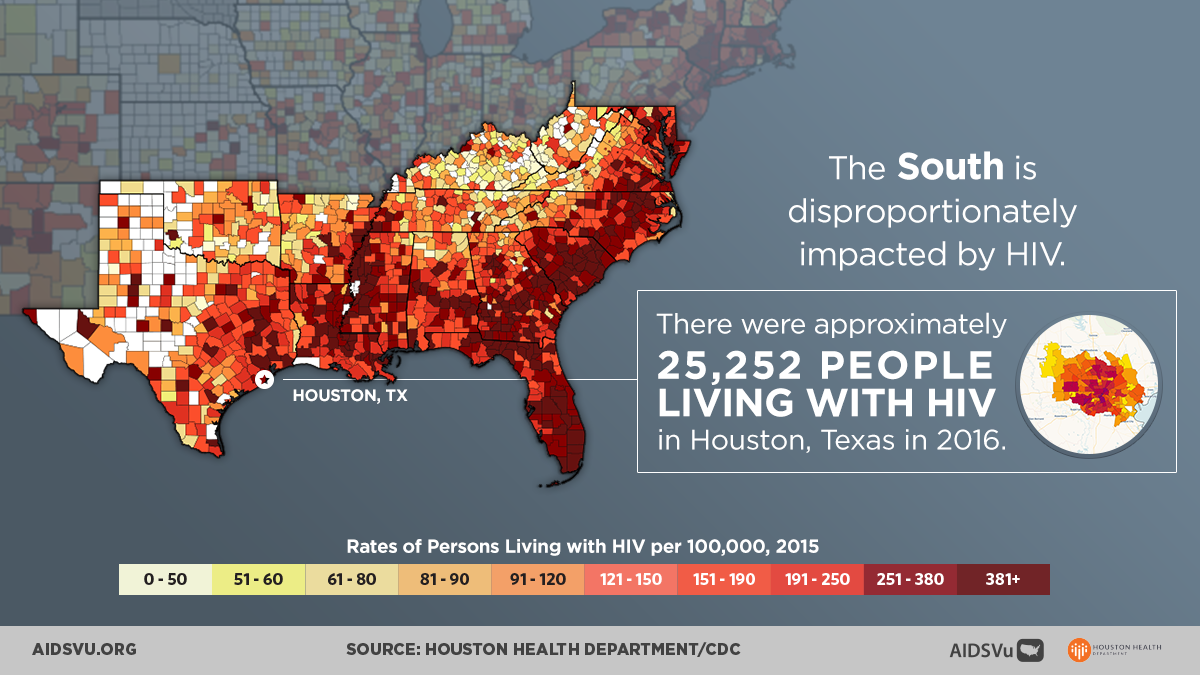
The Southern United States bears a disproportionate burden of HIV that reflects decades of structural inequities, policy decisions, and social determinants that have created conditions for HIV transmission and barriers to prevention and care. Despite accounting for only 38% of the U.S. population, the South represented 51% of all new HIV diagnoses in 2023 and accounts for approximately 49% of all estimated new HIV infections nationally. This concentration of the epidemic makes the South the epicenter of HIV in America.
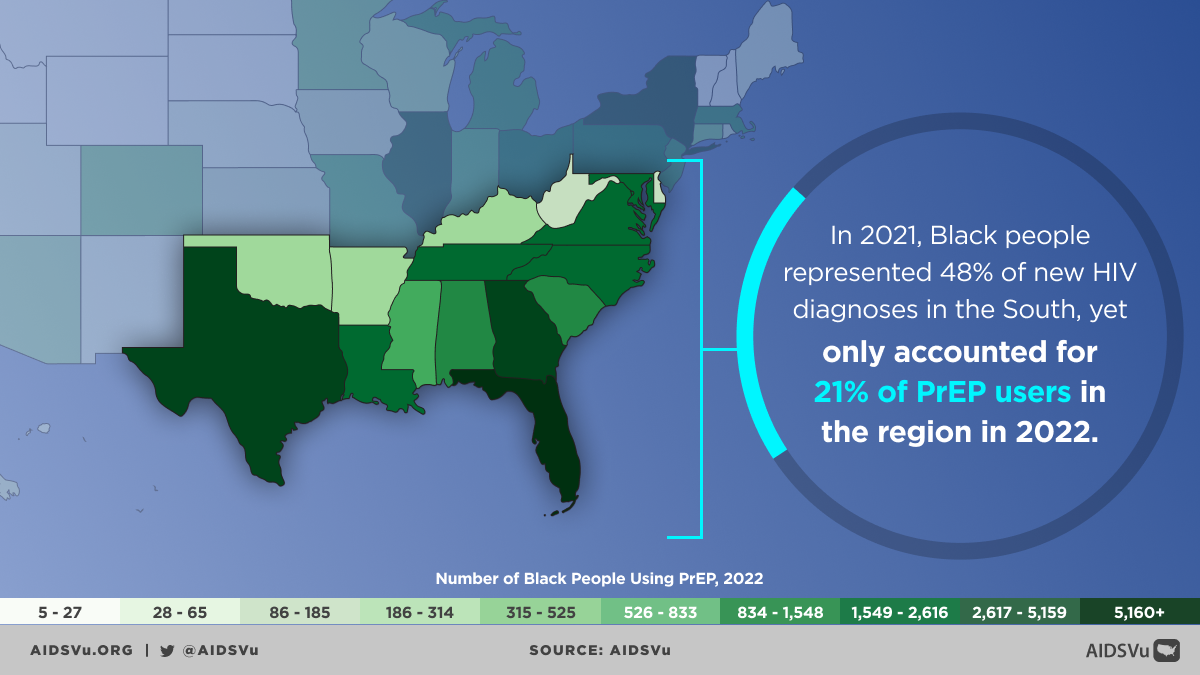
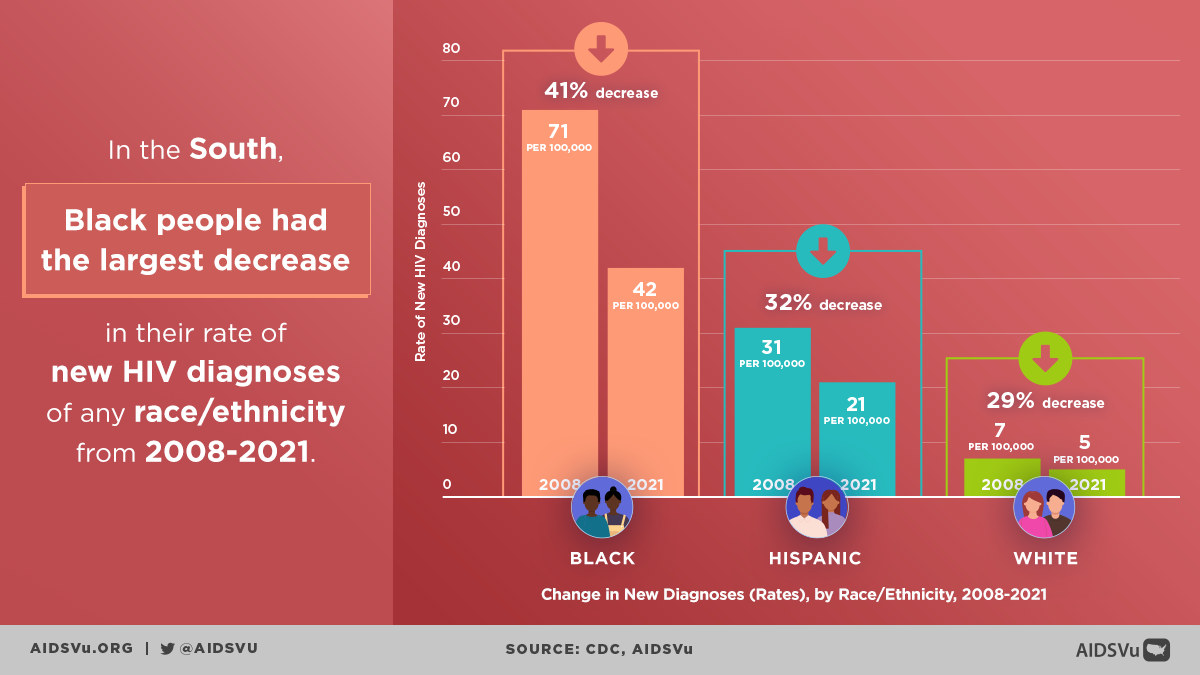
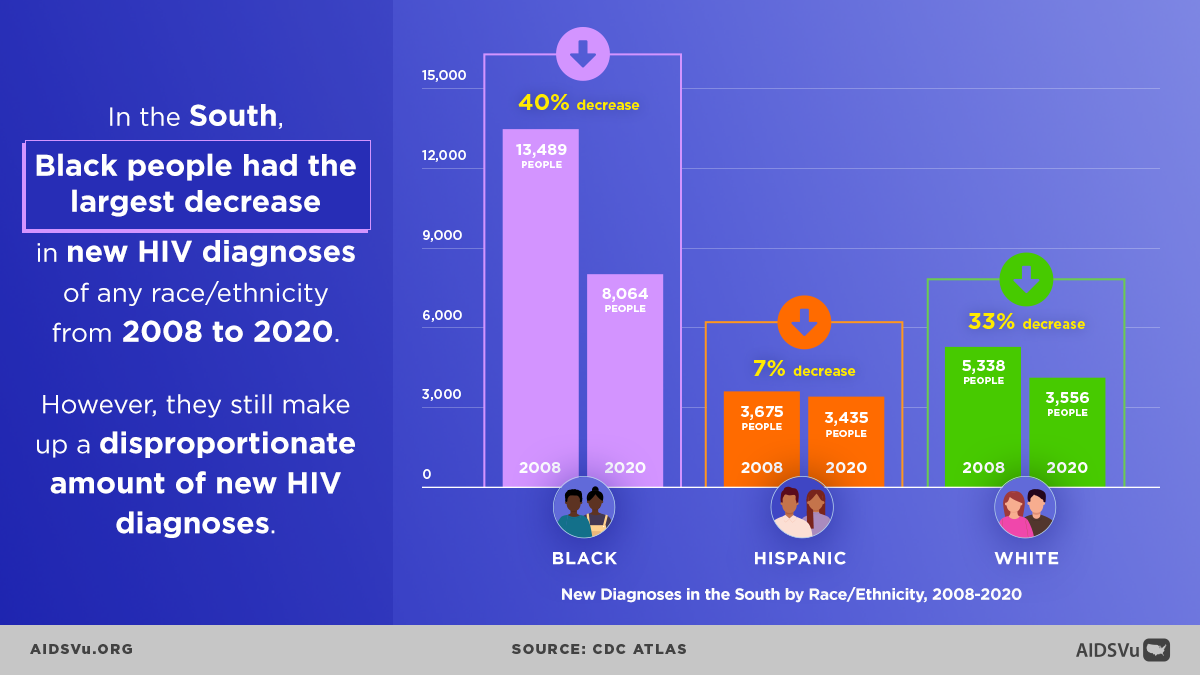
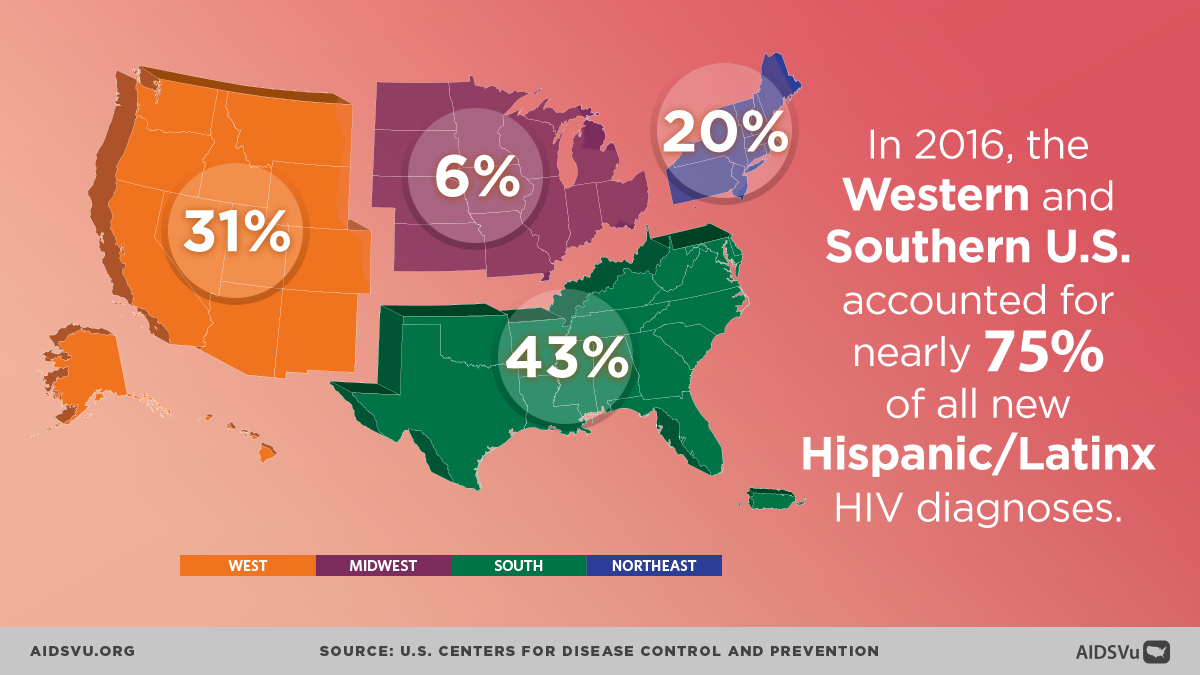
The disparities are even more pronounced when examining HIV’s impact on communities of color within the South. Black Americans in the South represented half of all new HIV diagnoses in the region despite comprising only 19% of the Southern population. This intersection of geography and race creates compounding vulnerabilities that require targeted, comprehensive responses addressing both regional factors and racial inequities.
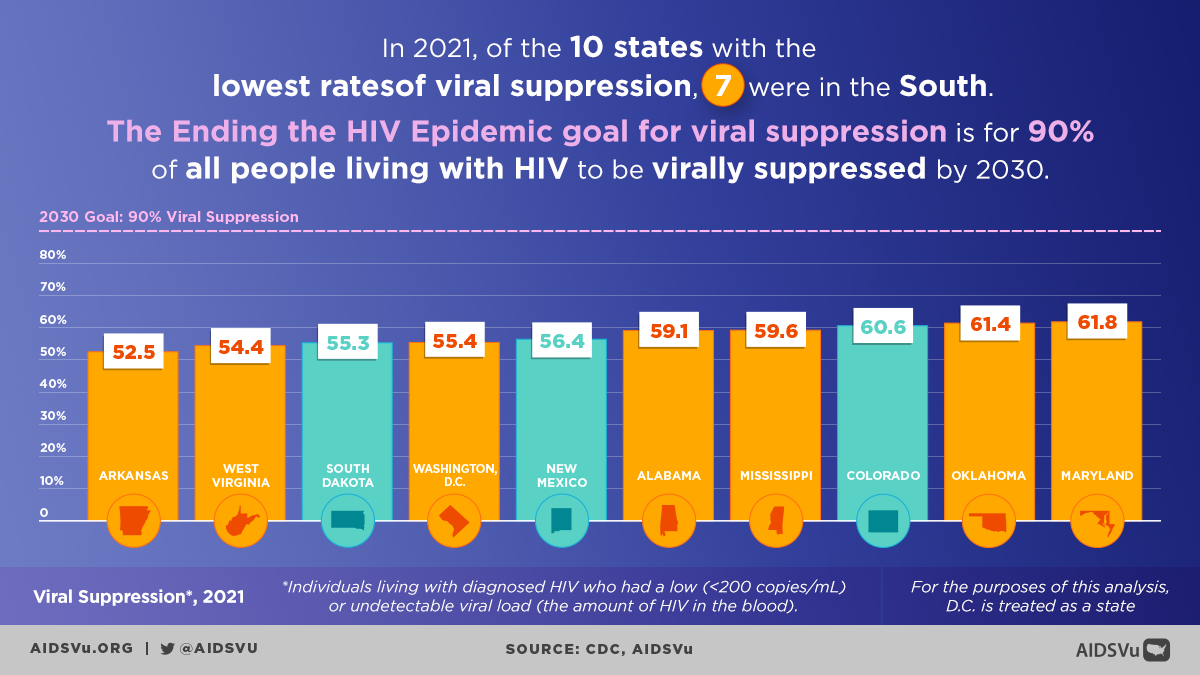
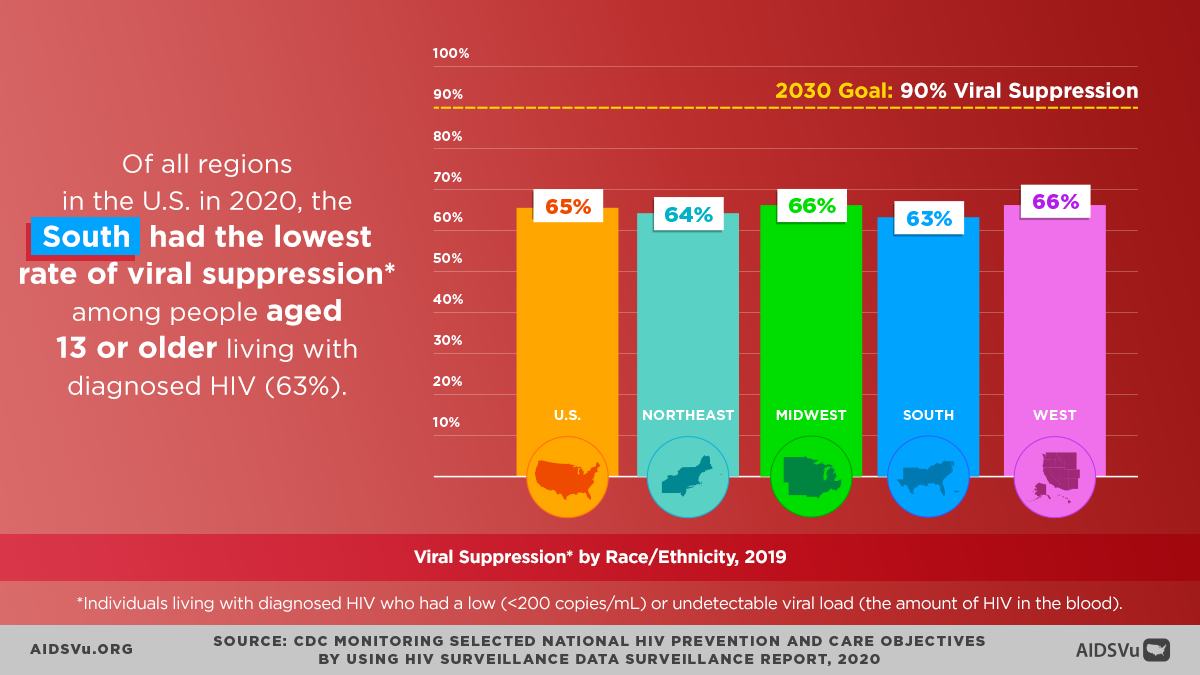
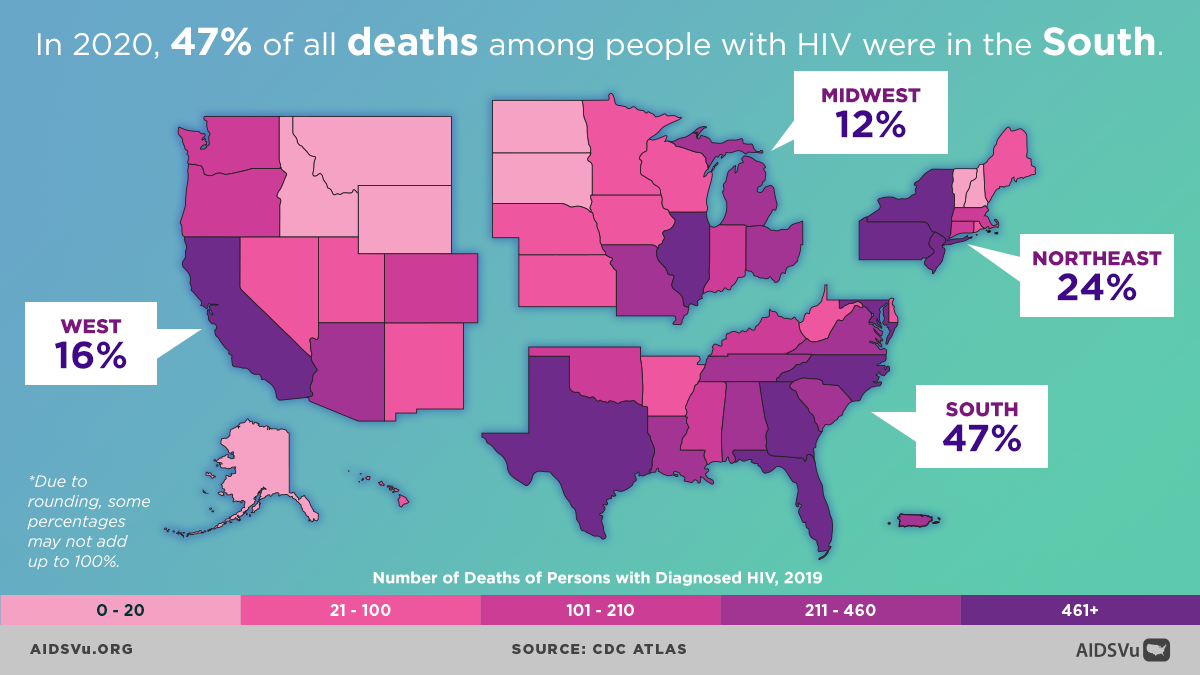
The burden extends beyond new infections to encompass the full spectrum of HIV outcomes. The South accounts for approximately 45% of all people living with diagnosed HIV in the United States and experiences higher rates of HIV-related mortality compared to other regions. These patterns reflect not only higher incidence but also challenges in HIV care access, retention, and viral suppression that affect long-term health outcomes.
Economic and Social Foundations of the Epidemic
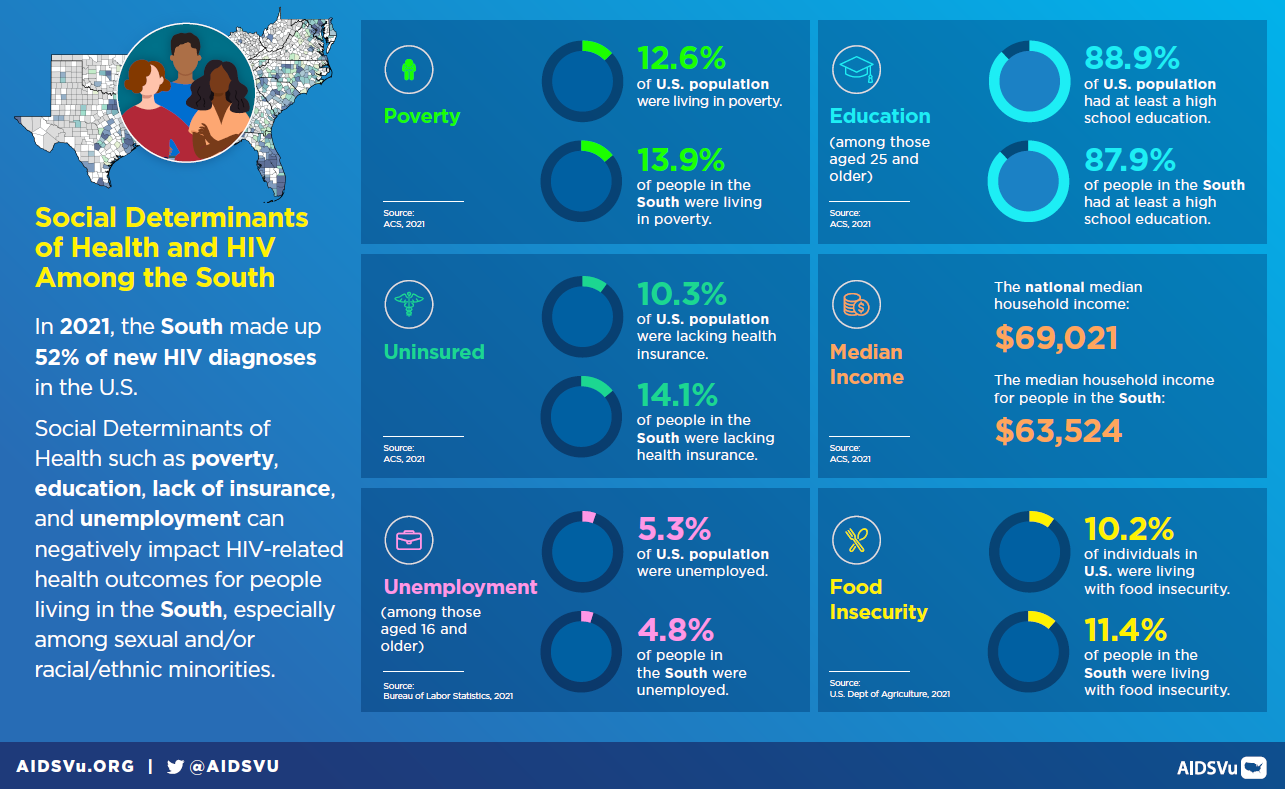
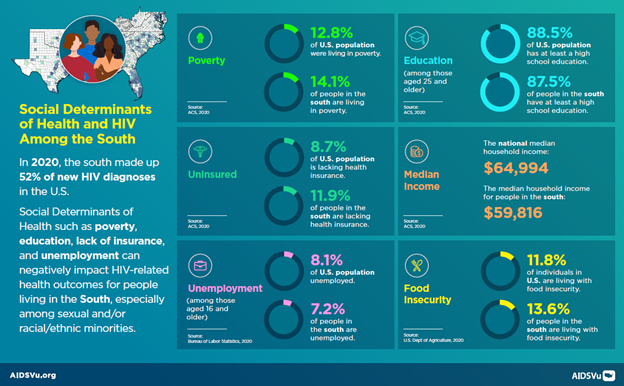
The HIV epidemic in the South is deeply rooted in economic and social conditions that create vulnerability to HIV while limiting access to prevention and care services. The South has the highest poverty rate and lowest median household income of any U.S. region, with economic disadvantage directly affecting health outcomes and HIV risk. Poverty influences HIV vulnerability through multiple pathways, including limited healthcare access, housing instability, food insecurity, and reduced capacity to negotiate safer sexual practices.
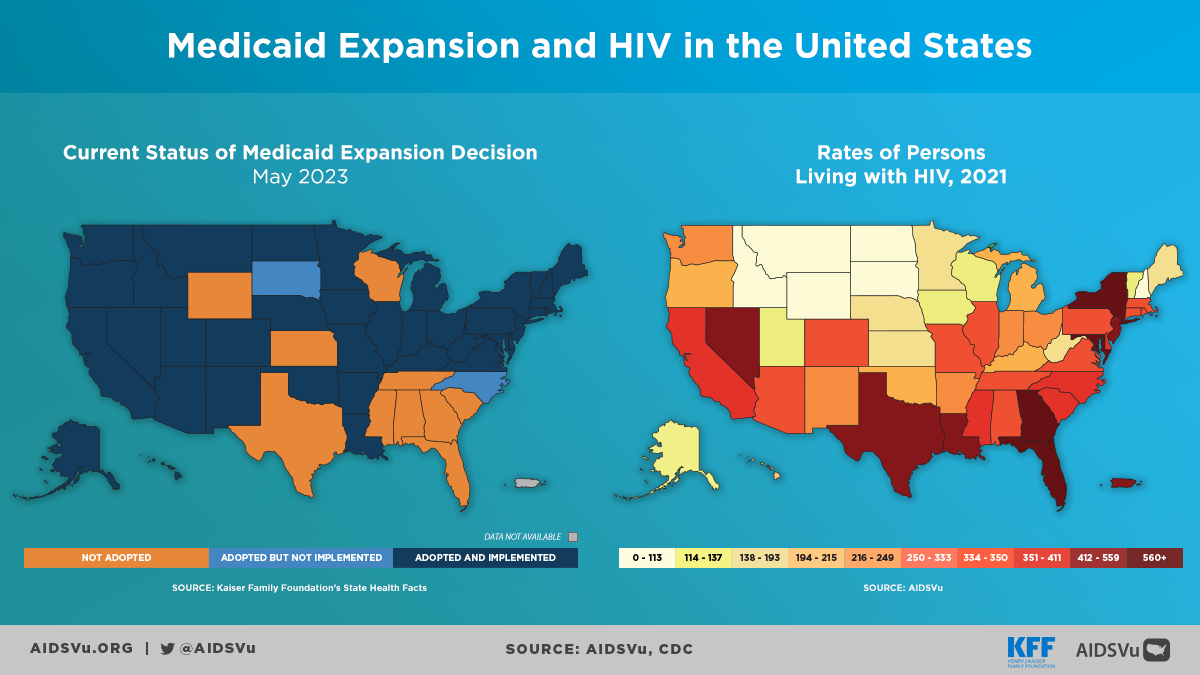
Nearly half of all Americans without health insurance live in the South, creating substantial barriers to HIV prevention, testing, and treatment services. This insurance gap is particularly pronounced in the nine states that have not expanded Medicaid under the Affordable Care Act. Medicaid serves as the largest source of coverage for people with HIV nationwide, making Medicaid expansion a critical factor in HIV care access. States that expanded Medicaid programs demonstrate significantly higher PrEP utilization rates—1.4 times higher on average compared to non-expansion states.
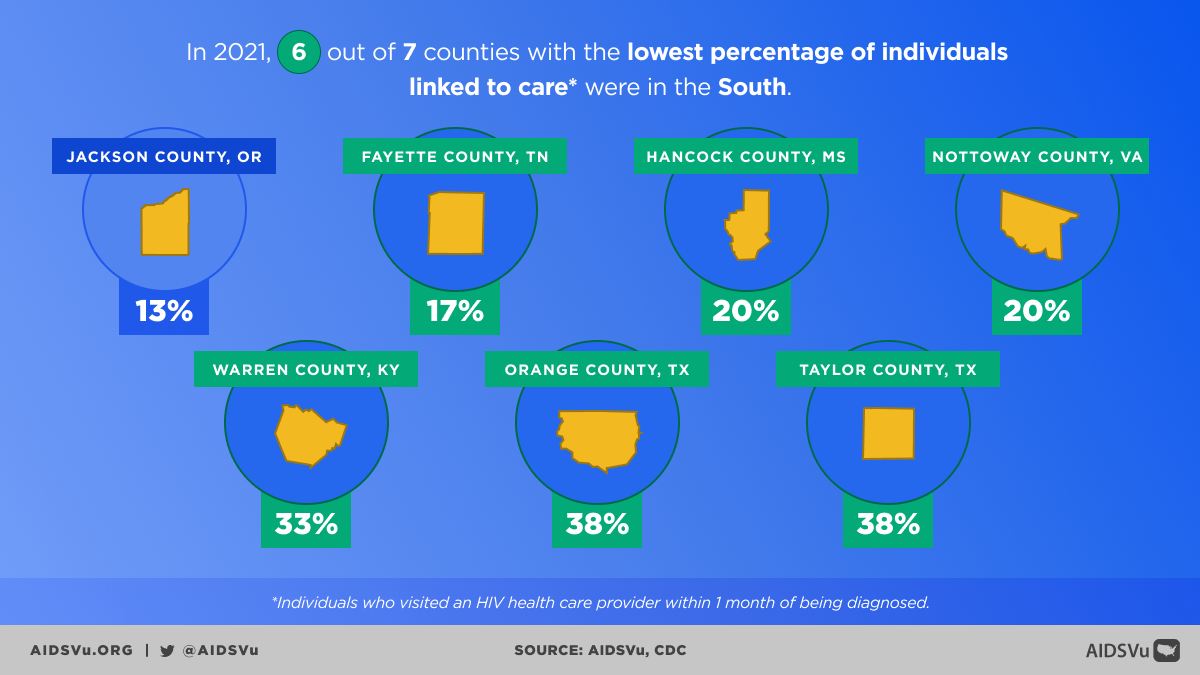
The concentration of uninsured individuals in the South creates cascade effects throughout the HIV care continuum. People without insurance are less likely to receive routine HIV testing, more likely to be diagnosed late in the course of infection, and face greater barriers to accessing consistent HIV care and treatment. These insurance-related barriers contribute to regional disparities in viral suppression rates and HIV-related health outcomes.
Rural Challenges and Geographic Barriers
Rural areas within the South face particular challenges in HIV prevention and care that compound regional disparities. Geographic isolation creates barriers including lack of public transportation, longer travel distances to receive care, and reduced availability of medical and social services compared to urban areas. These transportation and distance barriers can make routine HIV care visits difficult to maintain and may prevent people from accessing specialized HIV services.
Healthcare provider shortages affect rural Southern communities disproportionately, with many areas having no HIV-experienced clinicians. This workforce shortage means that people with HIV may need to travel long distances for specialized care or rely on providers with limited HIV expertise. The shortage is particularly acute for mental health and substance abuse treatment services that often complement HIV care.
The opioid crisis has created additional HIV risk in rural Southern communities, with injection drug use increasing HIV and Hepatitis C transmission risk. According to 2016 estimates, nearly 70% of counties vulnerable to HIV or hepatitis C outbreaks among people who inject drugs are located in the South. This vulnerability reflects both increased drug use and limited harm reduction services in rural areas.
Cultural and Social Factors
HIV stigma in the South is particularly pervasive and often intersects with stigma around sexual orientation, substance use, poverty, and sex work. This stigma operates at multiple levels, from individual internalized shame to community rejection to institutional discrimination in healthcare and social services. Southern religious and cultural traditions may contribute to stigma around behaviors associated with HIV transmission, making disclosure and help-seeking more difficult.
The intersection of HIV stigma with other forms of discrimination creates compounding barriers for key populations most affected by HIV. Gay and bisexual men may face rejection from families and communities, while people who inject drugs encounter criminalization and judgment that prevent them from accessing harm reduction services. These intersecting stigmas can delay HIV testing, interfere with care engagement, and prevent disclosure to sexual partners.
However, Southern communities also demonstrate significant strengths, including strong family and community networks, traditions of mutual support, and faith communities that can provide resources for healing and care. Many Southern HIV organizations have successfully leveraged these community assets while working to address stigma and discrimination.
Technology and Innovation Gaps
Southern states have been slower to adopt some HIV prevention and care innovations compared to other regions, creating missed opportunities for epidemic impact. For example, many Southern states have not widely implemented antigen/antibody combination HIV tests that can detect acute HIV infection when transmission risk is highest. Early detection of acute infection is crucial for both individual health outcomes and community prevention.
Similarly, adoption of newer prevention technologies like long-acting PrEP and integration of HIV services with routine healthcare have been uneven across the South. These innovation gaps may reflect resource constraints, workforce challenges, and policy environments that are less supportive of comprehensive HIV programming.
Telemedicine and digital health innovations offer particular promise for addressing geographic barriers in rural Southern areas, but implementation has been limited by internet access limitations, provider capacity, and regulatory barriers that restrict telehealth service delivery across state lines.
PrEP Access
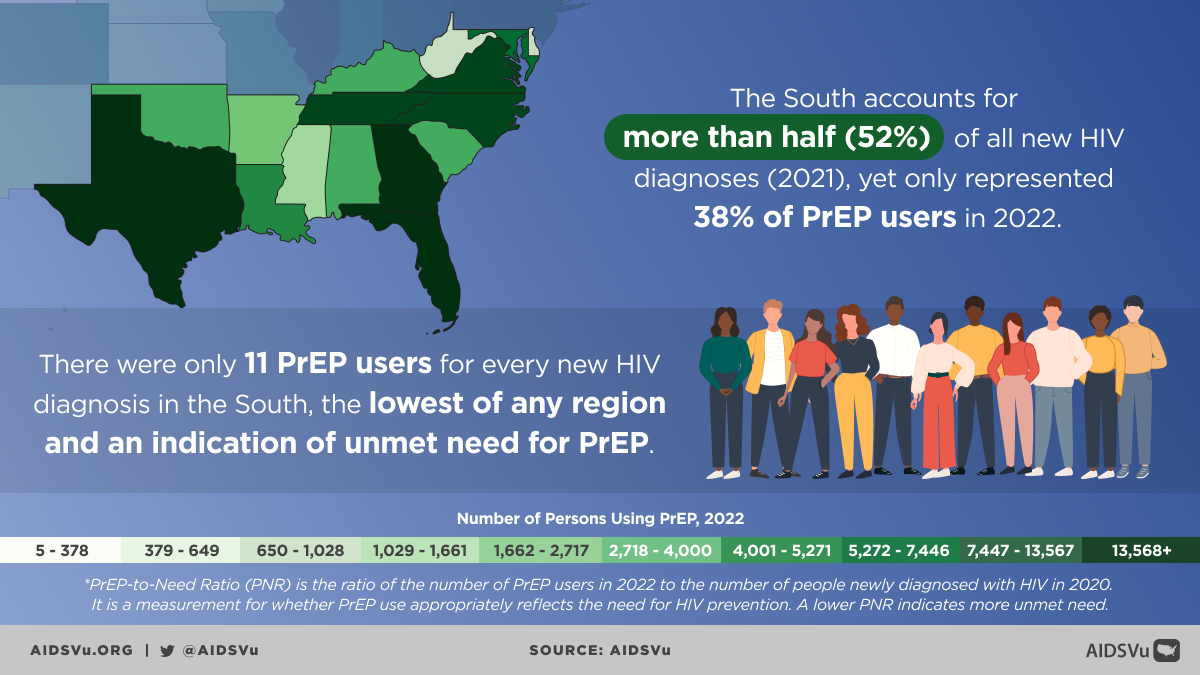
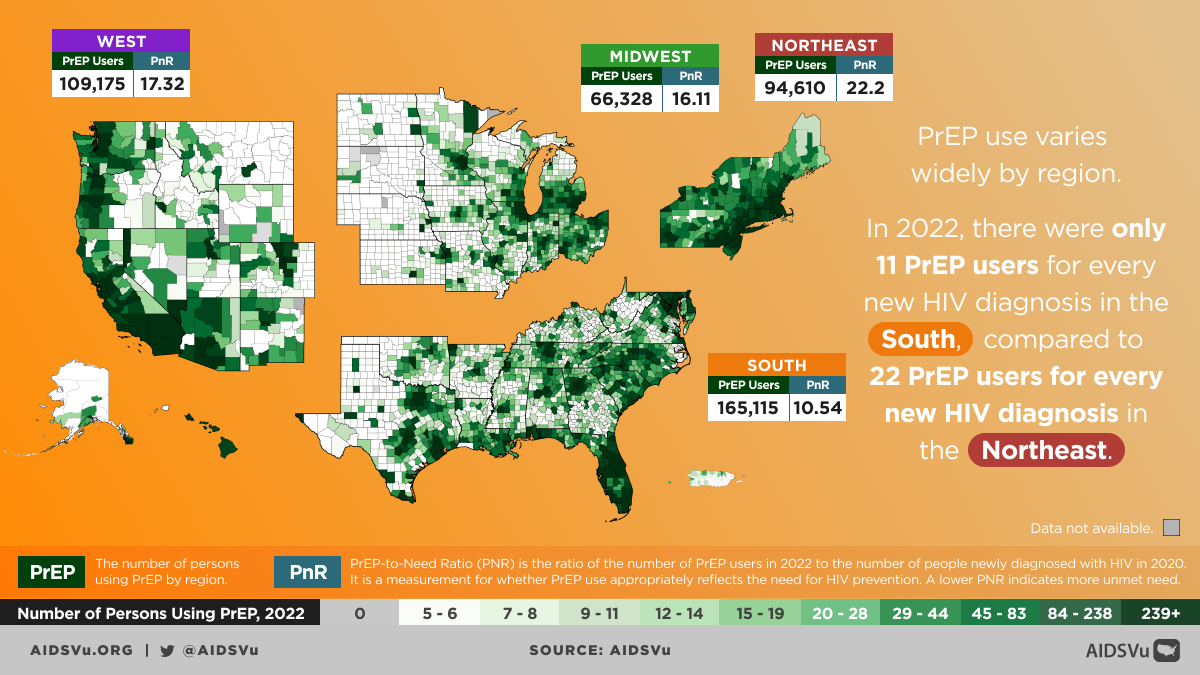
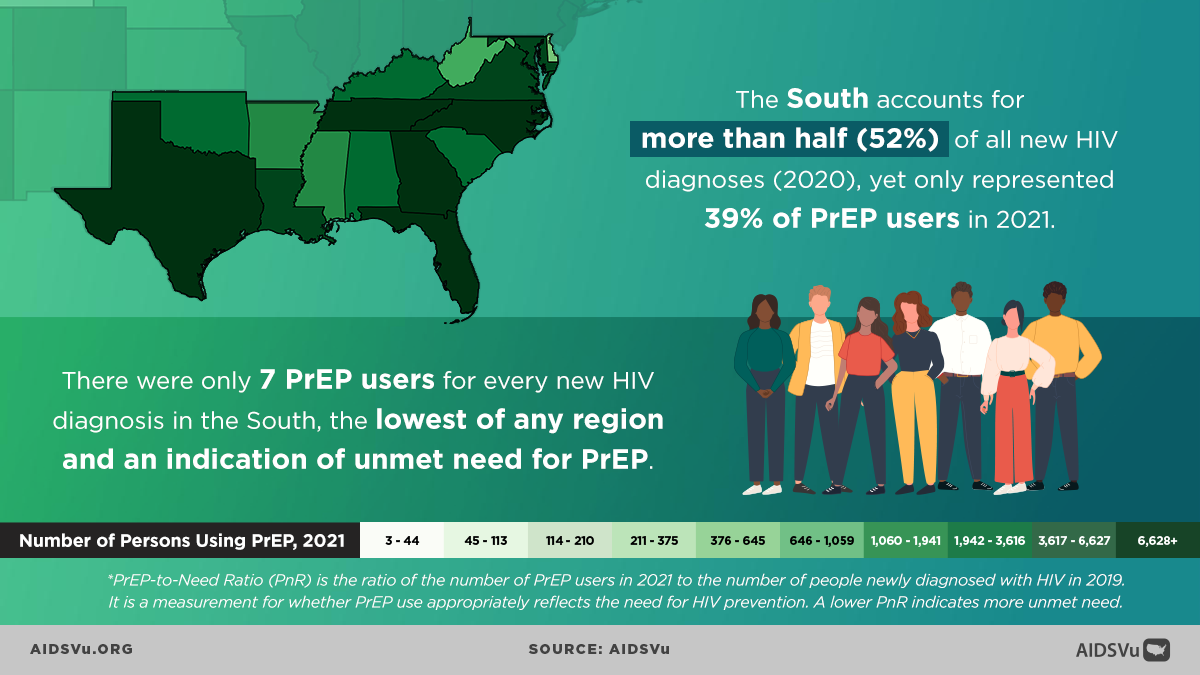
The South faces a particularly acute crisis in PrEP access and utilization that directly contributes to ongoing HIV transmission. Despite accounting for over half of new HIV diagnoses, the South accounted for only 38% of PrEP users in 2023. This dramatic mismatch between HIV burden and prevention tool utilization represents one of the most significant prevention gaps in the U.S. HIV response.
The disparities are even more pronounced for Black Southerners, who made up 48% of new HIV diagnoses in the South but only 21% of PrEP users. All five states with the greatest unmet need for PrEP are located in the South (West Virginia, Alabama, Puerto Rico, Mississippi, and South Carolina), highlighting the regional concentration of prevention gaps.
Multiple factors contribute to low PrEP uptake in the South, including limited provider knowledge and comfort with PrEP prescribing, insurance and cost barriers, stigma associated with HIV prevention medication, and concerns about confidentiality and discrimination. Rural areas face additional barriers including limited numbers of PrEP-prescribing providers and greater distances to access services.
Healthcare System Challenges
Southern healthcare systems face multiple challenges that affect HIV outcomes, including provider shortages, limited specialist availability, and organizational cultures that may not prioritize HIV care. Many Southern states have fewer infectious disease specialists per capita compared to other regions, and rural areas often lack any HIV-specialized providers.
The intersection of healthcare access barriers with stigma and discrimination creates particularly challenging environments for HIV care. People with HIV may delay seeking care due to concerns about confidentiality, fear of discrimination, or previous negative experiences with healthcare providers. These delays can result in late diagnosis, delayed treatment initiation, and poorer long-term health outcomes.
However, Southern healthcare systems also demonstrate innovations and strengths, including community health centers that serve as safety nets for uninsured and underinsured populations, academic medical centers that provide specialized HIV care, and community-based organizations that bridge healthcare and social service systems.
The Ending the HIV Epidemic Initiative Impact
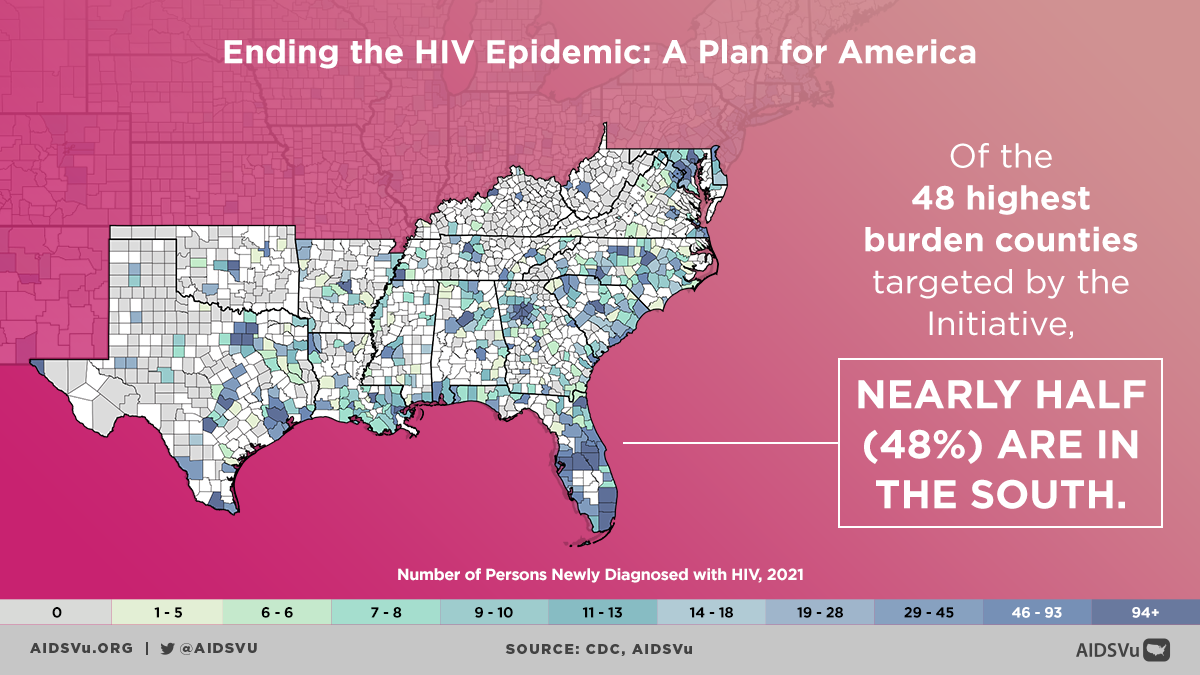
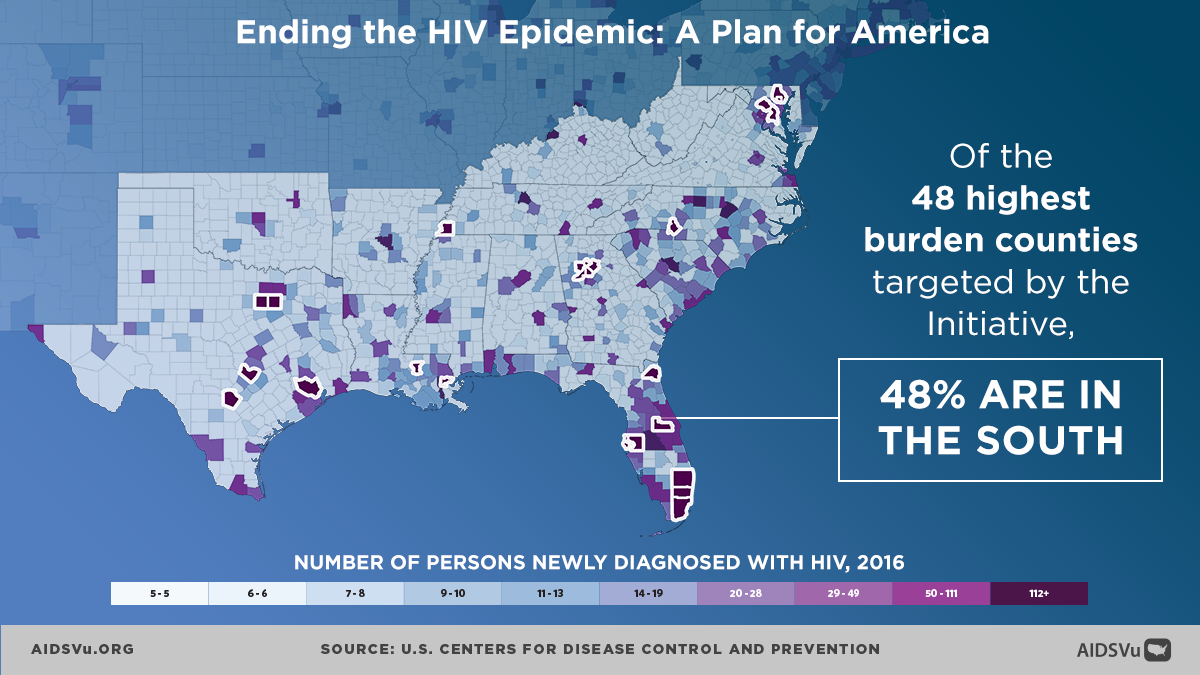
The federal Ending the HIV Epidemic (EHE) initiative has prioritized many Southern jurisdictions, recognizing the region’s disproportionate HIV burden. Of the 48 highest-burden counties targeted by the initiative, 48% are located in the South. Additionally, seven states with substantial rural HIV burden (Alabama, Arkansas, Kentucky, Mississippi, Missouri, Oklahoma, and South Carolina) receive dedicated EHE funding.
The EHE initiative has brought additional resources and attention to Southern HIV responses, supporting expanded testing programs, increased PrEP access, enhanced linkage to care services, and community-based prevention programming. However, the initiative’s success in the South faces particular challenges related to workforce shortages, infrastructure limitations, and policy environments that may not fully support comprehensive HIV programming.
Early indicators suggest that EHE investments are beginning to show impact in some Southern jurisdictions, with improvements in testing rates, linkage to care, and viral suppression outcomes. However, achieving the initiative’s ambitious goals will require sustained investment and attention to the structural factors that drive HIV vulnerability in the South.
Community Strength and Innovation
Southern communities have developed innovative, culturally responsive approaches to HIV prevention and care that build on regional strengths while addressing unique challenges. Faith-based HIV programming has been particularly important in the South, with many religious organizations providing HIV testing, care support, and stigma reduction programming that reaches people who might not access secular services.
Community-based organizations throughout the South have pioneered approaches that integrate HIV services with other community needs, including economic development, housing assistance, and criminal justice support. These integrated approaches recognize that HIV cannot be addressed in isolation from other life circumstances and community needs.
Southern HIV advocates and organizations have also been leaders in policy advocacy, working to expand Medicaid, protect civil rights, and increase HIV funding. This advocacy has achieved important victories while building coalitions that can support sustained policy change.
Looking Forward: Comprehensive Solutions
Addressing HIV in the South requires comprehensive approaches that acknowledge both the urgency of the epidemic and the complex factors that sustain HIV transmission and limit care access. Policy-level interventions remain crucial, particularly Medicaid expansion in the remaining non-expansion states, which would dramatically improve HIV care access and outcomes.
Workforce development represents another critical priority, including training programs for HIV care providers, incentives for providers to practice in underserved areas, and support for innovative service delivery models that can extend specialist care to rural and underserved communities.
Community-based programming needs sustained funding and support to expand reach while maintaining cultural responsiveness and community connections. This includes support for peer navigation programs, community health worker initiatives, and faith-based programming that can reach populations that traditional healthcare systems might miss.
The fight against HIV in the South ultimately reflects broader struggles for health equity, economic justice, and social inclusion. Success will require not only expanding access to HIV services but also addressing the poverty, discrimination, and structural inequities that create vulnerability to HIV and barriers to care. Only through such comprehensive approaches can the South achieve the HIV outcomes that all communities deserve.
5 Ways to Use AIDSVu
Explore Maps
Explore the interactive map, customize your view, and easily print for presentations, grant applications, or other materials.
Learn MoreView Local Statistics
View local statistics for your city or state, and download high-impact data visualizations for your work
Learn MoreDownload Data
Download the datasets that inform AIDSVu’s visualizations for your own research and analysis
Learn MoreLocate Services
Visit our service locators to find and share HIV prevention, testing, and Ryan White care services across the South. Our service locator also includes service location sites in the Deep South for stigma reduction, overdose prevention/reversal, harm reduction, and trauma-informed care.
Learn MoreInteractive Maps
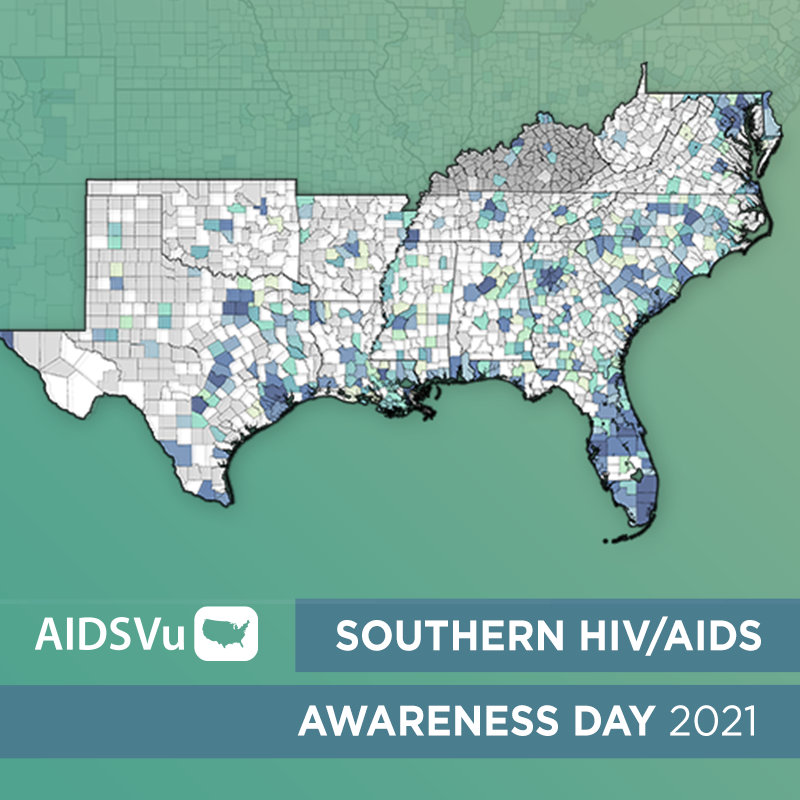
Explore AIDSVu’s interactive maps that visualize HIV prevalence, new diagnoses and mortality in the Southern U.S. Filter by race/ethnicity, sex, age, and transmission category to see how HIV impacts certain groups.
Beyond the Map
AIDSVu offers tools and resources beyond the HIV map that provide users with a deeper understanding of the HIV epidemic, its socioeconomic-driving factors, and services available at the community level.
Social Determinants of Health
See how HIV prevalence is related to poverty, high school education, median household income, etc.
Learn MoreFind Services
Use the testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services locators to find critical HIV/AIDS services near you.
Learn MoreLocal Data
View city and state profiles with local HIV/AIDS statistics, national comparison charts, and local resources.
Learn MoreFor More Information
Learn more about the impact of HIV in the Southern U.S. with the following additional resources.