Dustin Hampton, M. Ed. Is the Bureau Chief of the Missouri Department of Health and Senior Services for HIV, STDs, and viral hepatitis and has worked in the field for over 15 years.
Kate Cleavinger, PhD, MPH is a senior epidemiologist for communicable disease in the Office of Epidemiology at the Missouri Department of Health and Senior Services.
How did you both become involved in this particular field of public health?
Kate: I was an undergraduate during the early years of the AIDS epidemic in the US which is how I initially got interested in the field of microbiology. I started out as a molecular microbiologist, working mostly with bacterial pathogens. Then four years ago, I went into the field of public health and this past year joined the Office of Epidemiology in the Department of Health and Senior Services providing data support to the Bureau of HIV, STDs and Hepatitis. So, I’ve really come full circle.
Dustin: I started in the field of HIV prevention about 17 years ago. It was my freshman year of college. I am from a small town in southeast Missouri where we did not talk about HIV or sex often, so I did not have much knowledge in that field. At an Earth Day event there was a booth that was promoting and advertising the Mpowerment Project, a behavioral intervention to reduce HIV infection. I became involved with that and quickly got a part-time job doing prevention education for that organization, which soon became a full-time position.
I earned a Masters in Counseling Psychology and transitioned into a role providing case management for people with co-occurring mental health conditions and HIV co-occurring. A few years later I moved to the Columbia/Boone County Health Department, the regional prevention lead agency contractor for Central Missouri. I have been here at the state Department of Health and Senior Services for about seven years. I started as a Prevention and Testing Program Coordinator, and now I am the Chief of the Bureau of HIV, STD and Hepatitis.
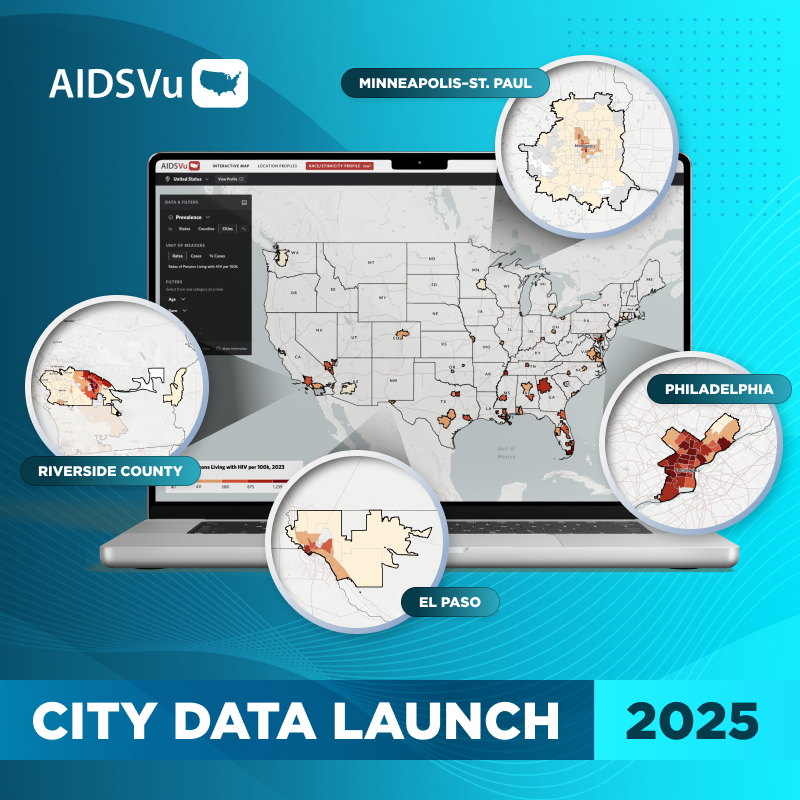
AIDSVu is adding city-level data for St. Louis and Kansas City, Missouri for the first time this year. Why is it so important to have city-level data available to the public?
Kate: At the state-level we do not have the capacity to regularly produce the kind of public-facing data that AIDSVu does, but we receive data requests from local health departments and CBOs asking for more granular data so that they can target their care better. The data that AIDSVu provides can help address their needs. There is now more data available to more people at a faster pace, which is great. A detailed ZIP Code breakdown of the cities is especially helpful. AIDSVu also offers additional data such as PrEP use data and the ability to overlay other factors for comparison, whether that is testing sites, PrEP sites, or some of the social determinants of health.
Dustin: Time, people, and money are limited. Having zip code level data available to our partners and the public is important to help ensure those limited resources are being focused in the geographic areas where they are most needed.
For example, a large percentage of people with HIV live north of I-70 in the St. Louis area, but whenever we looked at the places we were contracting for prevention and care, coverage in this area was lacking. This was a big factor that drove us to try to ensure that we are providing services where people are. While St. Louis may have public transportation, it still could take all day to get across town to get into a care appointment. In addition, not everyone has a job where they can take time off to take the bus for those kinds of appointments. This speaks to the idea of health equity and ensuring that we are giving people care where they are and where they want to receive it.
We have an expanded testing program out of Wash U in St. Louis, where a lot of emergency rooms and urgent cares are doing opt-out testing. Finally, after years of trying, they got into a hospital system just north of I-70. In the first month of operation, they identified 10 people with HIV who were unaware of their status, so the need was clearly already there.
Missouri is an Ending the Epidemic (EHE) state, one of the seven states targeted for additional funding by the EHE initiative. Missouri also has a lower rate of HIV diagnoses and lower HIV prevalence than the national average. What was Missouri doing to try and end the HIV epidemic prior to the federal plan and how has the federal EHE initiative impacted your own local efforts?
Dustin: The EHE money has been beneficial in allowing us to take that next step. We have PS18-1802 and PS20-2010 (EHE) funding, which are prevention and testing-based. We viewed EHE as an extension of what we already do to end the HIV epidemic.
The additional funding has been beneficial for working with additional partners, expanding services, and trying to get PrEP navigation to the public. We have been able to start up three PrEP clinics in rural southeast Missouri, where previously people were driving three hours to St. Louis each way just to access PrEP.
One of the reasons we were funded as a statewide jurisdiction is because of that rural burden. Missouri has two metropolitan areas on each side of the state, Kansas City and St. Louis. Those are both Transitional Grant Areas (TGAs) as well. They are large metropolitan areas, and they have a bi-state TGA.
At the broader state level, we also have some other regions. In Southwest Missouri, Springfield is the population center, but there is HIV in places beyond that immediate area. Unfortunately, in some of our regions, the only infectious disease provider is a three-hour drive each way. When it is the only provider, they get booked up quickly. With some new cases, it has taken 50 days to get someone into care. That is not meeting that goal of getting someone in within 30 days, much less within the seven days that is ideal.
EHE has allowed us to expand our prevention services, and increase access to Ryan White Care. The income limit for Missouri is 300% of the federal poverty level. As a case manager, I knew people that would be over the limit because they got a 25-cent per hour raise, but that 25 cents per hour was not going to pay those medication costs or those housing costs.
We have been able to expand what we are doing with EHE care to make sure we are able to provide medications, medical visits, and labs—those basic services for people that do not meet the Ryan White qualifications.
One of the big things that we are doing, and that Kate and her team have been instrumental in developing, is trying to get people back into care. We have some contractors that will focus on those individuals that we either know are not receiving care, or that we do not have evidence that they are receiving care, and to see what services they may still need or if there is some financial assistance that we can provide through EHE funding.
The entire goal is to get people on medications, keep people healthy, and if we can get people to that undetectable viral load to prevent transmission, we are really doing our jobs to reduce infections.
Despite positive progress compared to the rest of the region, what challenges still remain for Missouri when it comes to HIV care, treatment, and prevention?
Dustin: There are still a lot of challenges, HIV stigma being one of them. Stigma prevents people from getting tested. It prevents people from receiving care or taking their medication. It prevents people from disclosing that they are living with HIV. Missouri, overall, is a rural and conservative state, and we try to address that stigma. Last year we did a campaign against stigma—one for the general public but also one for providers, because we knew that clients were experiencing stigma trying to receive primary care.
During COVID, there was a lot of distrust and politicization of healthcare, and of public health especially. It was already difficult enough for our Disease Intervention Specialists (DIS) to contact somebody after they had been diagnosed to try to get partners and provide partner services. But now it is all that much harder for DIS.
STD rates did not decrease during COVID, but testing decreased. Even with the testing decrease, our STD rates still increased. Syphilis has high rates at the moment, but even more concerning is that the populations that we have diagnosed with syphilis have changed. Before COVID it was predominantly men that have sex with men in metropolitan areas that were diagnosed with syphilis. Recently, we have seen a shift to White heterosexual individuals in southern rural areas who have a history of injection drug use, especially methamphetamine. We have seen congenital syphilis increase considerably as well. In addition, there is a historical trend of seeing syphilis increase and then a year or two later we see an HIV increase.
This really concerns me. These are populations that we have not messaged to in decades. There are populations that have no idea that they are at risk for HIV, and sometimes there are also populations that hold a lot of stigmas towards HIV. It is important for us to try to intervene now to prevent those increases that we might see into the future.
Kate: The COVID-19 pandemic had a profound effect on public health even at a data level. One positive outcome was that it really forced us to modernize how we collect and disseminate surveillance data, but on the flip side it made getting some of that data more difficult. Because of the stigma surrounding HIV, many people are understandably hesitant to provide information to public health. When you add the distrust of public health that really increased during COVID-19, it just makes it really difficult to get complete data, which in turn makes it harder for us to identify those most of need of medical care or other services.
Dustin: I know just from my work around the state and as a case manager, there are specific areas of the state where injection drug use is especially active. Injection drug use and diagnoses of either syphilis or HIV often correlate, but we do not have enough information about substance use or injectable drug use, which prevents us from having a good grasp on what is happening across the state and from being able to intervene in useful ways.