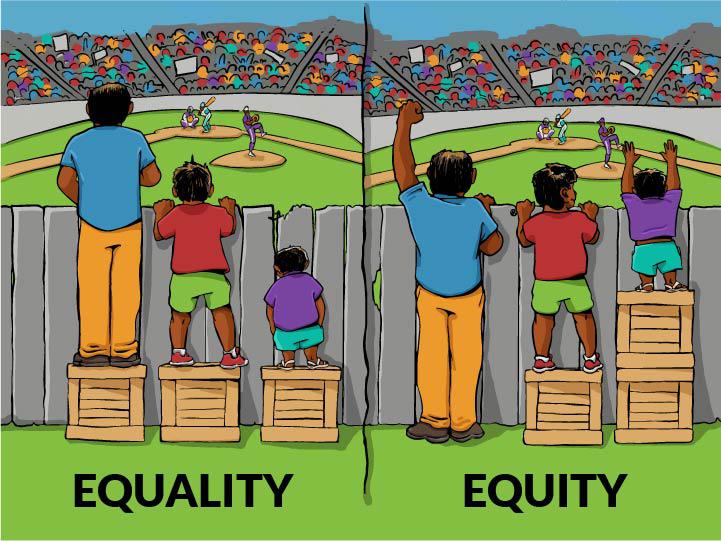
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving this requires ongoing societal efforts to:
- Address historical and contemporary injustices;
- Overcome economic, social, and other obstacles to health and health care; and
- Eliminate preventable health disparities.
To achieve health equity, we must change the systems and policies that have resulted in the generational injustices that give rise to racial and ethnic health disparities.
Health equity is closely linked to the concept of health disparities and social determinants of health (SDOH).
Health Disparities
The Centers for Disease Control and Prevention (CDC) defines health disparities as “differences in the incidence, prevalence, and mortality of a disease and the related adverse health conditions that exist among specific population groups. These groups may be characterized by gender, age, race or ethnicity, education, income, social class, disability, geographic location, or sexual orientation.” Addressing disparities in health is important to increase the health outcomes of the broad population, reduce health care costs, and achieve equity (KFF).
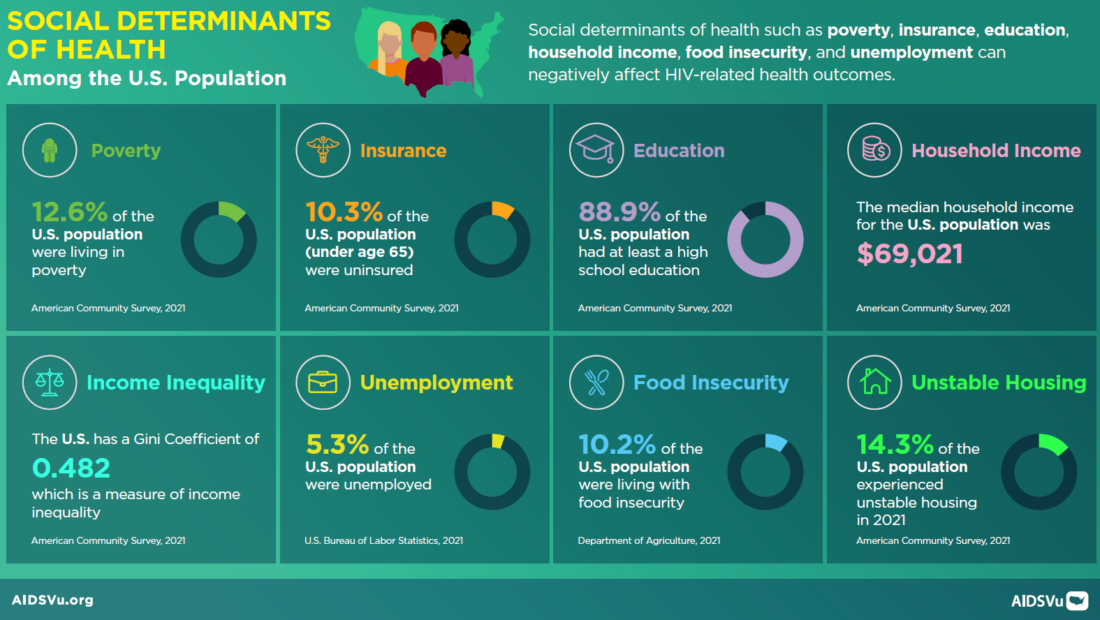
Social Determinants of Health (SDOH)
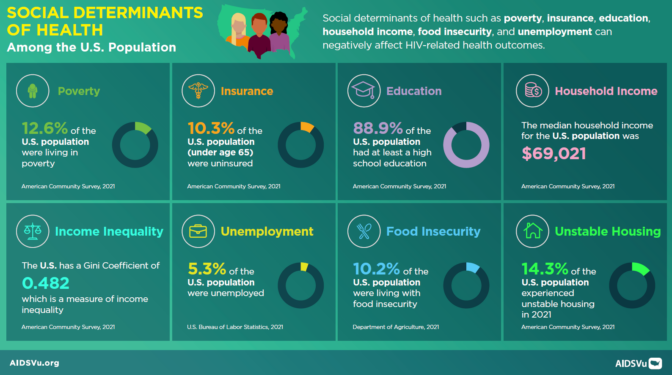
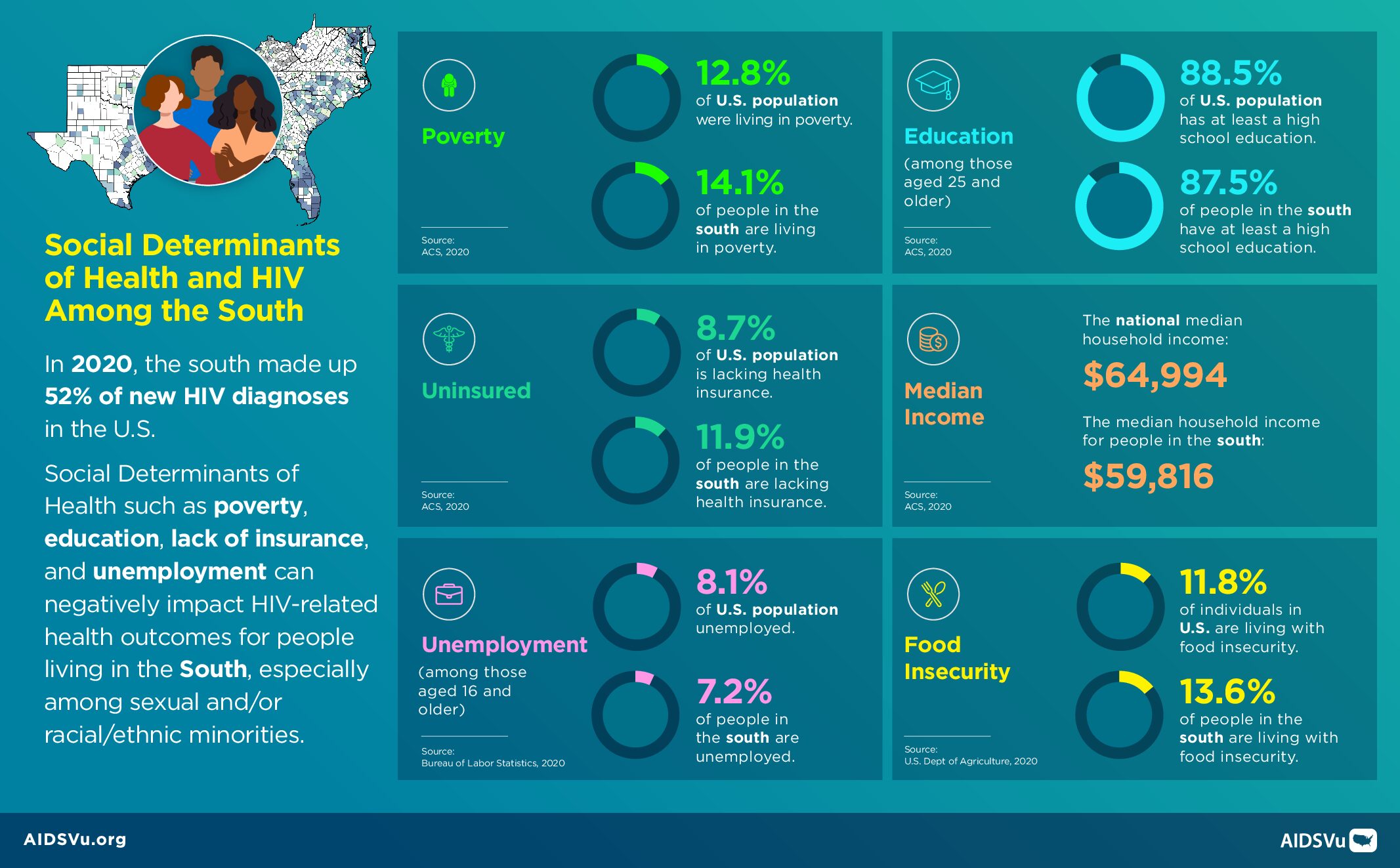
Social determinants of health are the conditions in the places where people live, learn, work, play, and worship that affect a wide range of health risks and outcomes. Long-standing inequities in six key areas of social determinants of health are interrelated and influence a wide range of health and quality-of-life risks and outcomes. Examining these layered health and social inequities can help us better understand how to promote health equity and improve health outcomes.
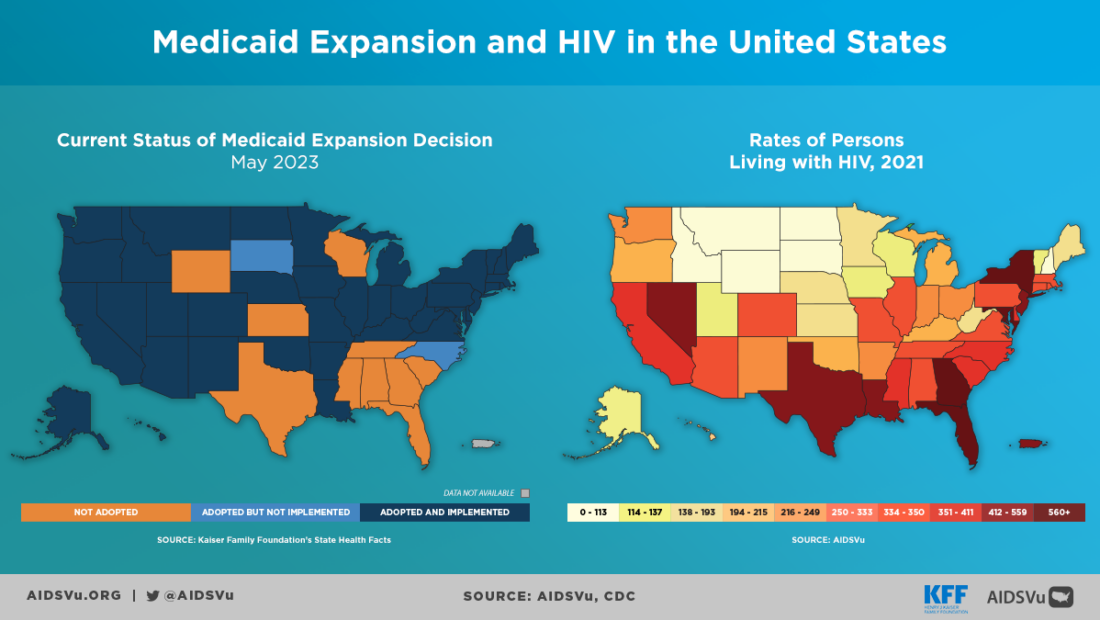
If we are going to end the HIV epidemic in the U.S., it is essential to understand why HIV has a disproportionate impact on certain groups over others and the wide array of factors that drive the disparities we see at the local-, state-, and national-level.
A complex set of individual, provider, health system, societal, and location-related factors contribute to disparities in health. (KFF).
A combination of poor SDOH and identity-related experiences can lead to insufficient HIV prevention and care for an individual. Though these disparities are not exclusive to HIV, they should be considered in research, policymaking, and advocacy to properly target programmatic interventions and resources for those most burdened by the epidemic.
SDOH on AIDSVu
To help users better understand the association between HIV and social determinants of health (SDOH), AIDSVu provides interactive maps of SDOH indicators that can be viewed alongside maps of HIV prevalence, new diagnoses, HIV mortality, the HIV Care Continuum, and PrEP utilization. These indicators include:
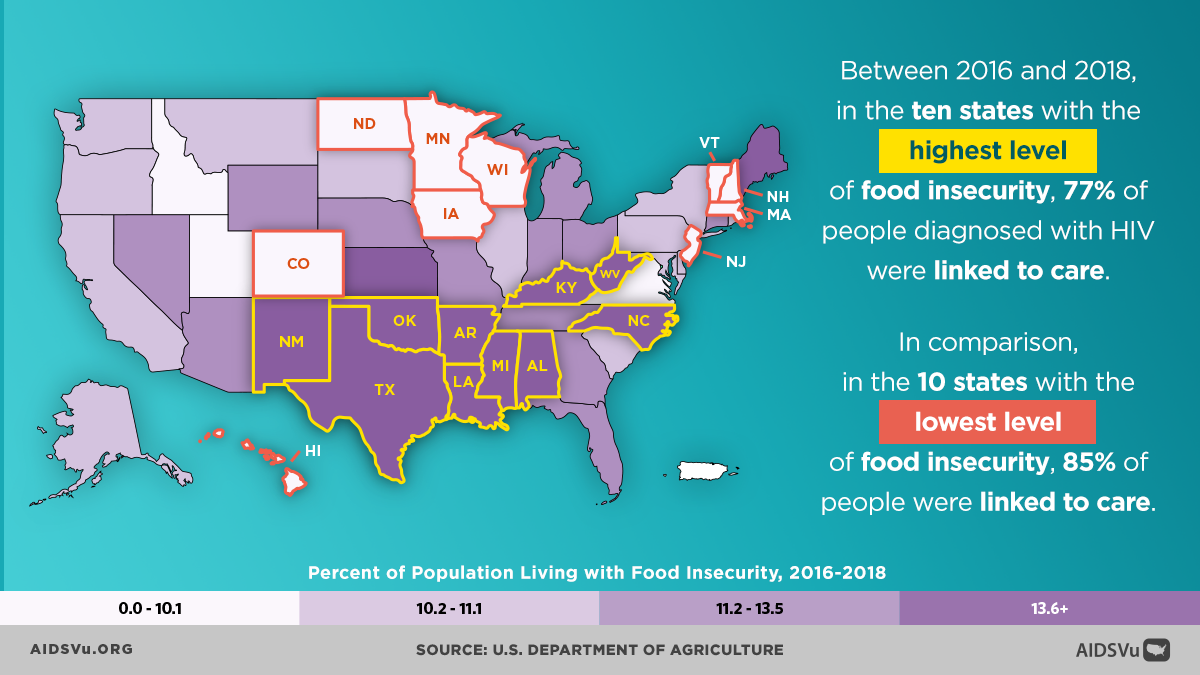
- Food insecurity (cumulative 2020 to 2022)
- High School Education (2022)
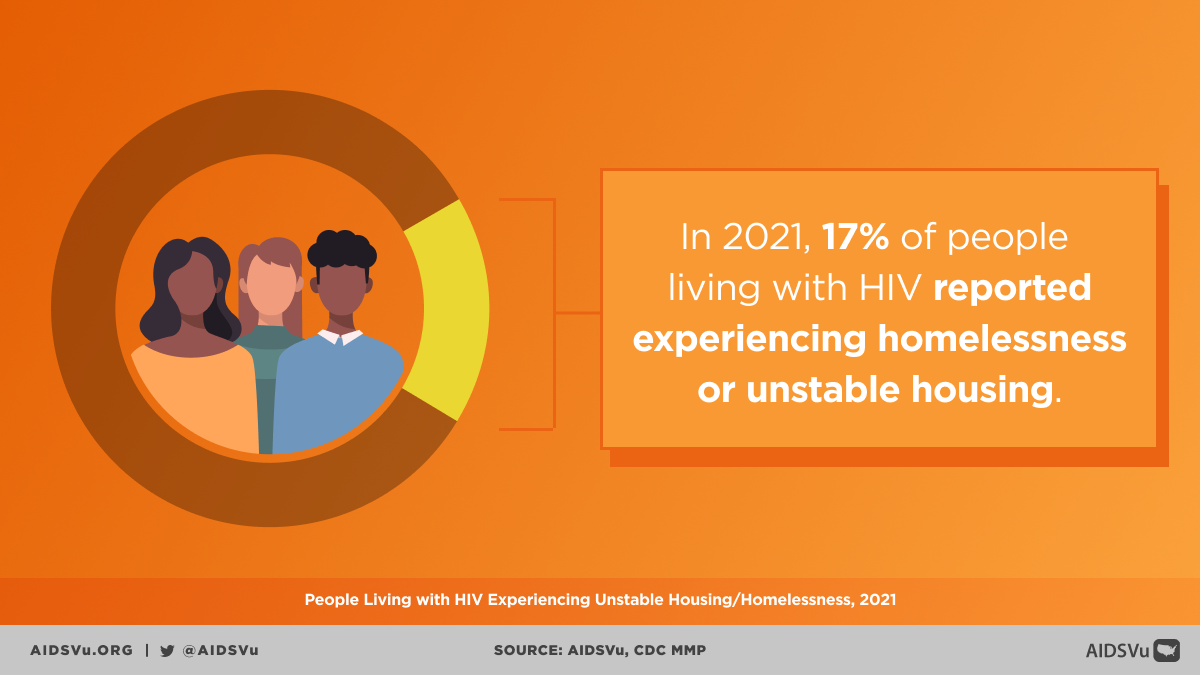
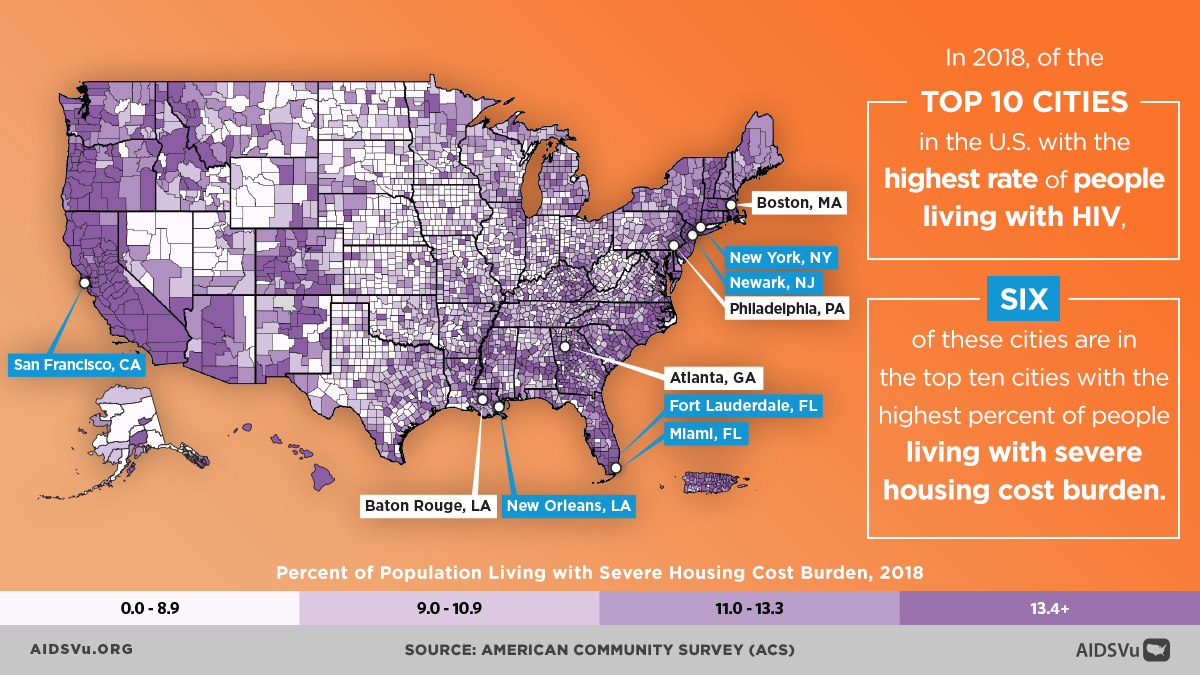
- Housing (2022)
- Income Inequality (2022)
- Median Household Income (2022)
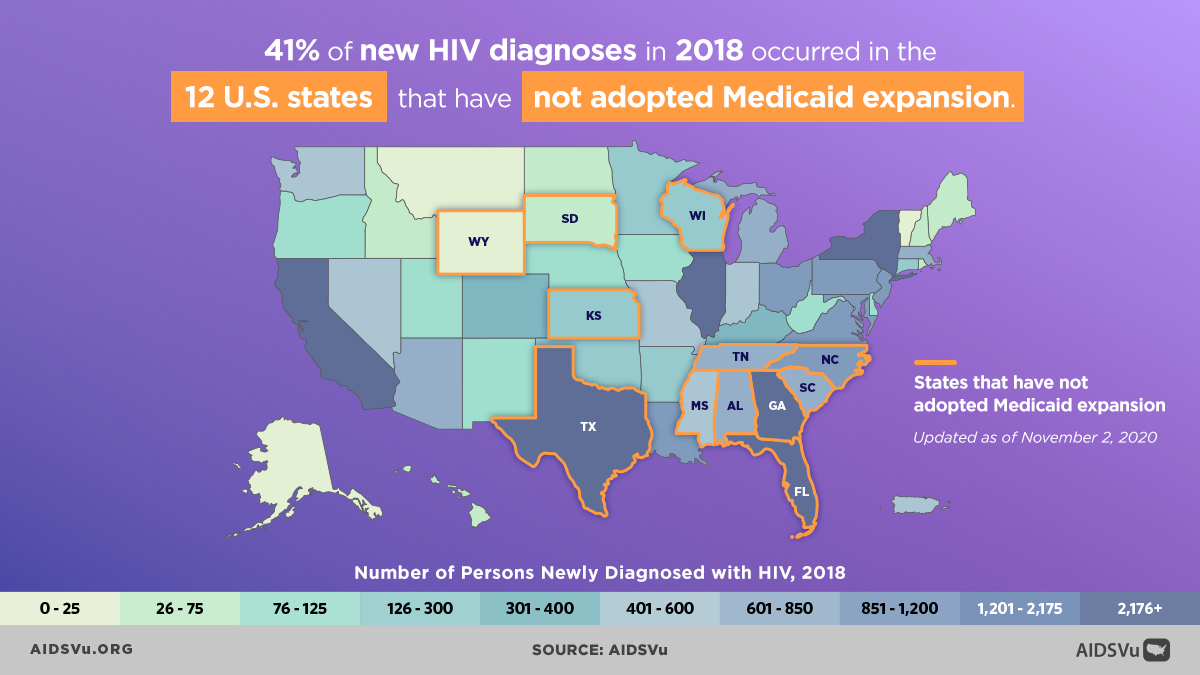
- Medicaid expansion (as of August 2024)
- People Without Health Insurance (2022)
- Poverty (2022)
- Unemployment (2022)
AIDSVu also displays maps of infectious diseases that are closely associated with HIV, including:
- Hepatitis C prevalence (cumulative 2013 to 2016)
- Primary and secondary syphilis prevalence (2022)
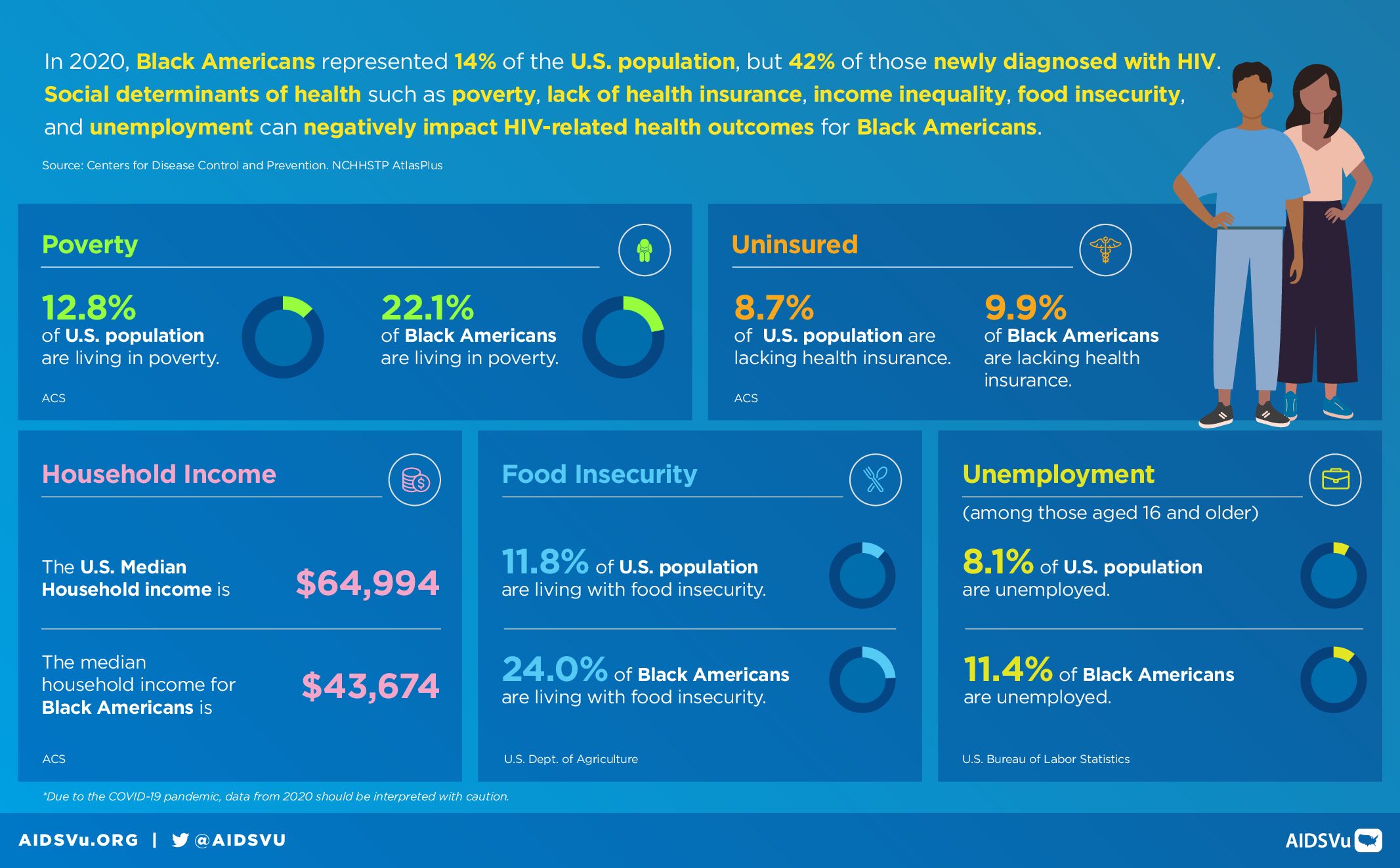
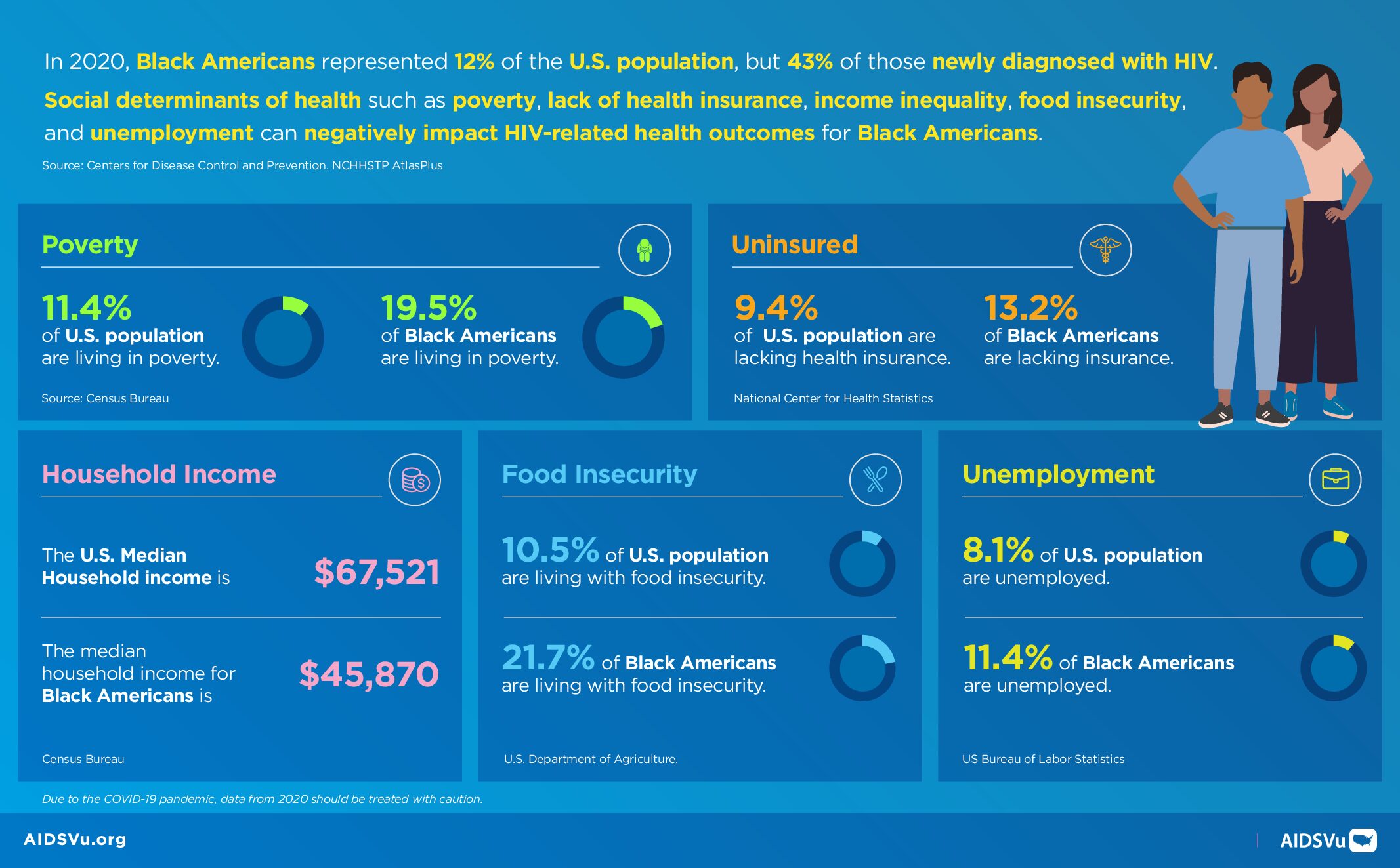
HIV-Related Health Disparities Among Racial and Ethnic Minorities
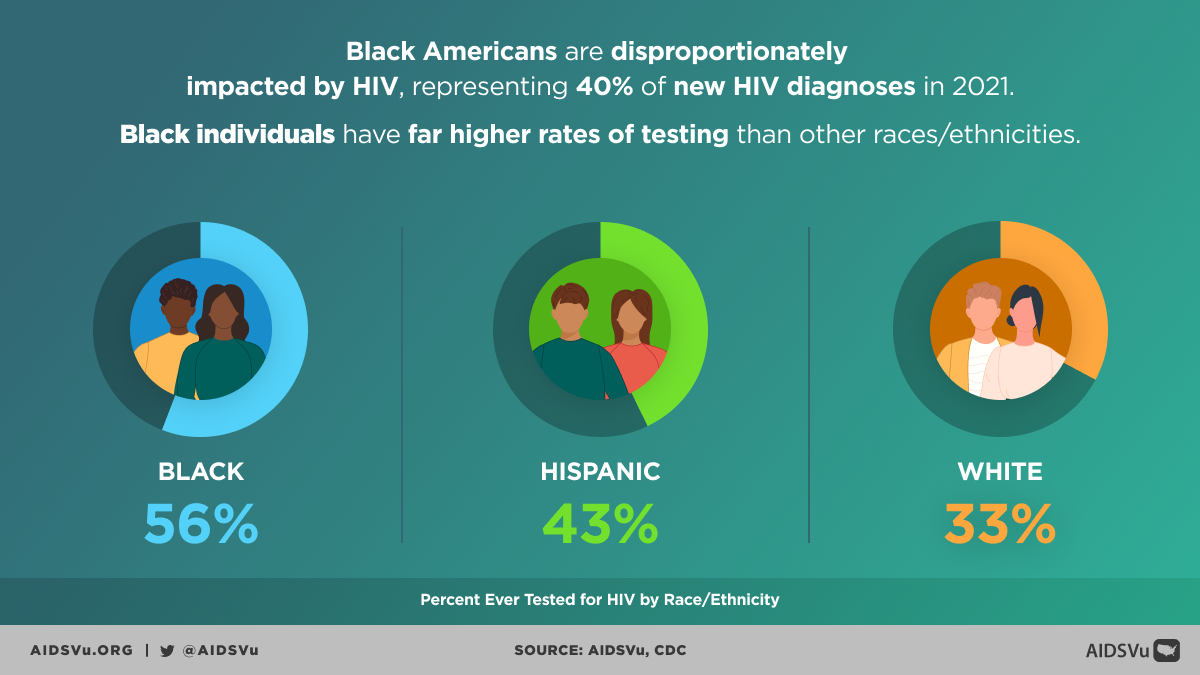
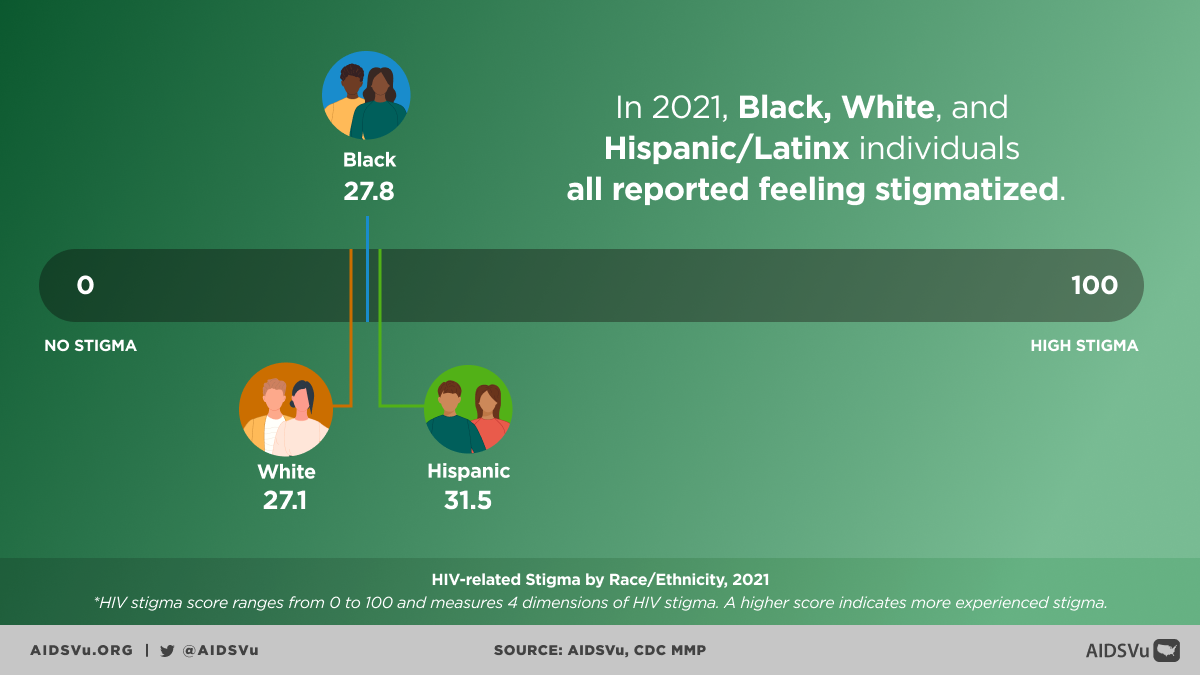
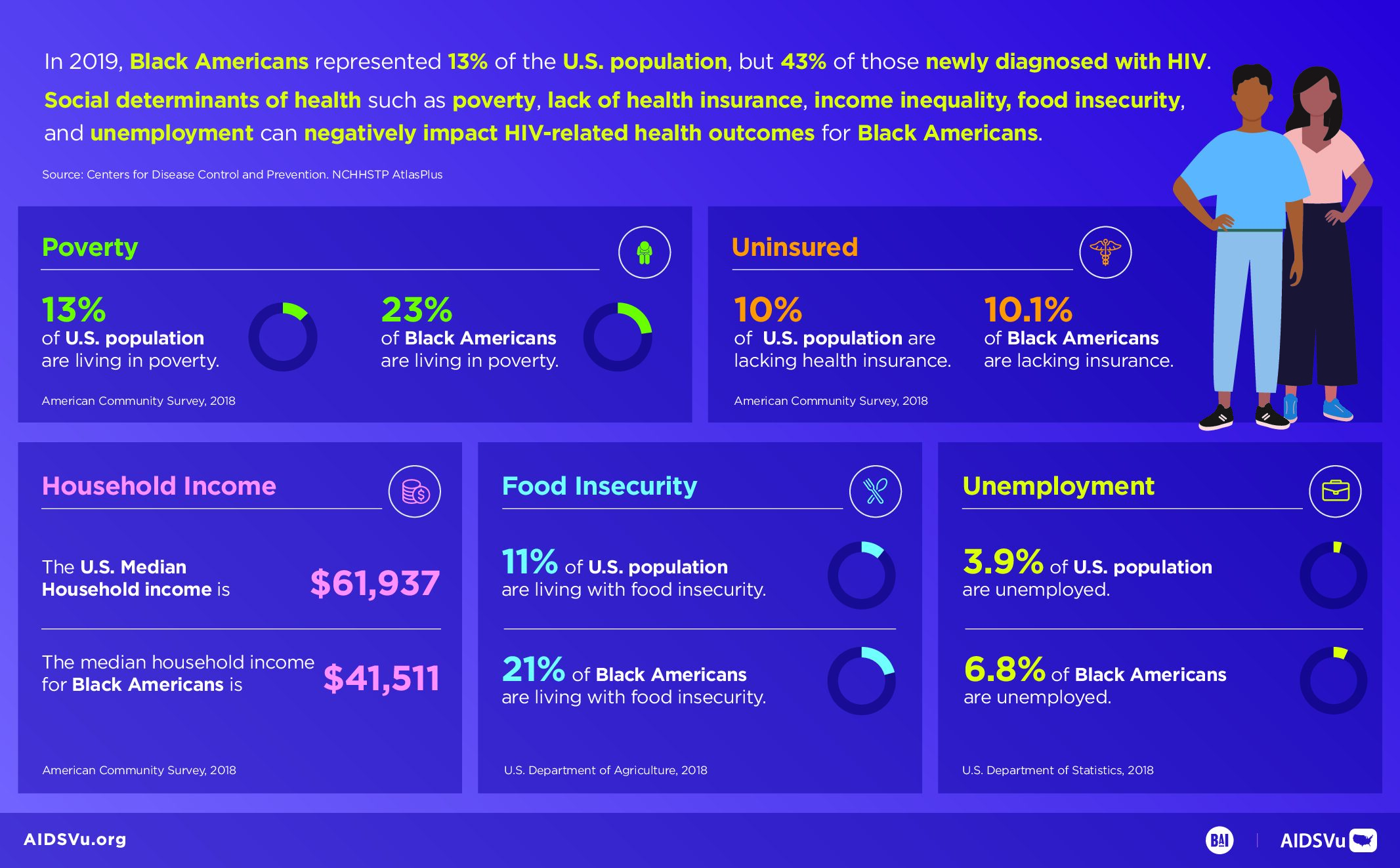
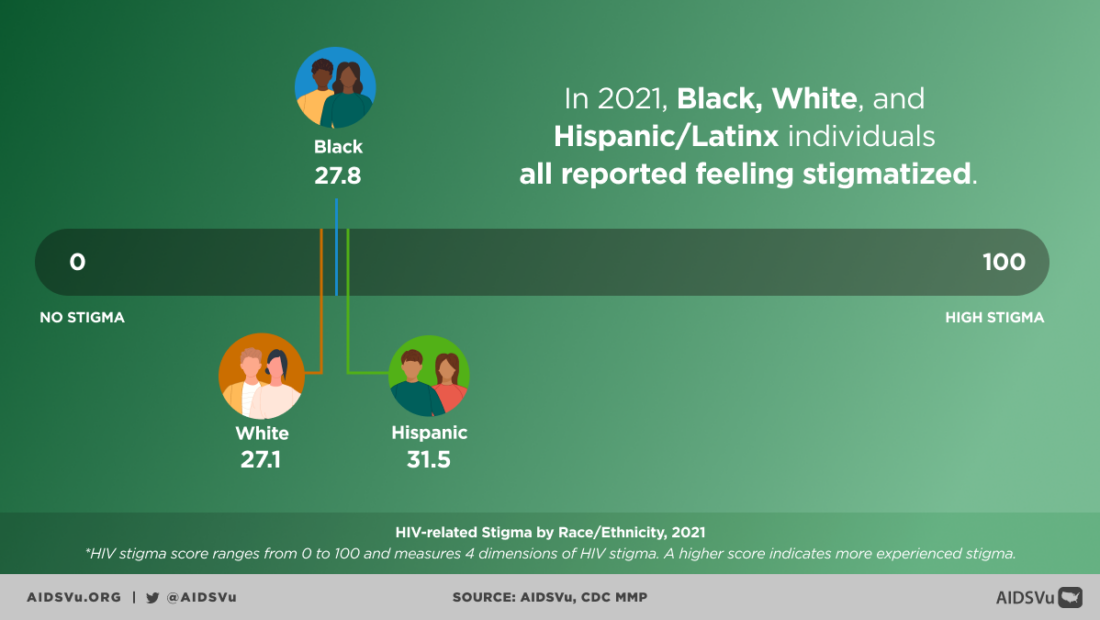
HIV-related health disparities are significant among racial and ethnic minorities. Black Americans represented 38% of all new HIV diagnoses but only 13% of the population in 2022. Not only are Black Americans disproportionately impacted by HIV, but they also experience SDOH that often lead to poorer health outcomes. This is the case with other racial and ethnic minorities as well, including Hispanic/Latinx individuals. In 2022, Hispanic/Latinx people represented 16% of the U.S. population but comprised 32% of those newly diagnosed with HIV.
Language barriers and cultural practices can also pose barriers to accessing HIV education and care. In some cultures, such as in East Asian cultures, it is a taboo to discuss illness—especially when related to sex. Cultural beliefs can contribute to stigmatized beliefs about HIV, fewer instances of seeking essential HIV medical care, significant underreporting of HIV cases, and inequitable intervention resource allocations (CDC). Additionally, concern for immigration status can place pressure on racial/ethnic minorities to avoid health services because they fear the impact that an HIV diagnosis can have on their residential security in the U.S. (CDC).

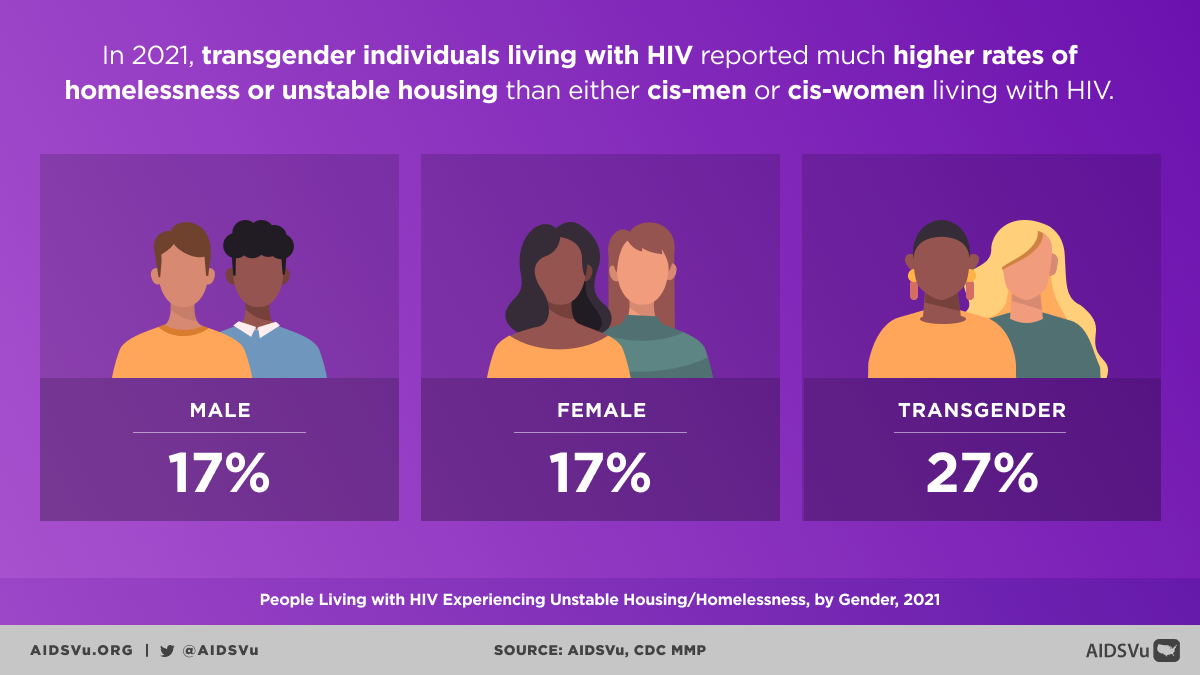
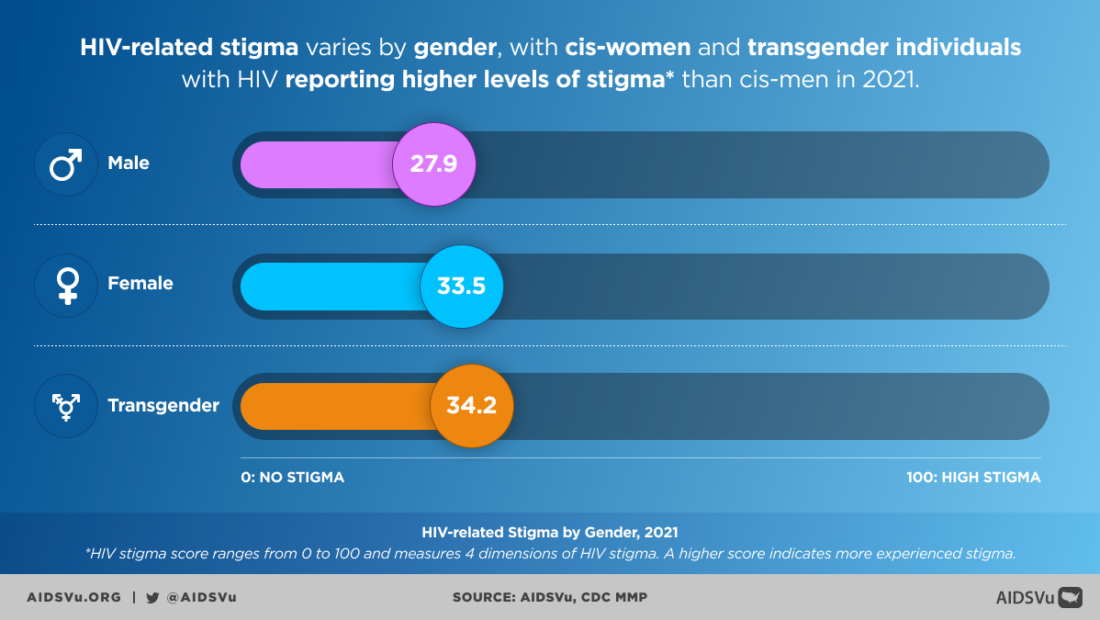
HIV-Related Health Disparities Among Sexual and Gender Identity Minorities
For the LGBTQ community, and other minority groups, HIV stigma has been ever-present since the 1980s when the epidemic first began (CDC). Confusion and fear about how the virus spread led to blaming much of the LGBTQ community, which reinforced existing stigma and fueled traumatic experiences for many individuals. Discrimination bled into many essential spaces in society, including the workplace, the justice system, and health care centers, which complicated efforts to live as a healthy and economically stable individual. This discrimination is still in effect today, leading to high levels of medical mistrust for many LGBTQ individuals.
2/3 of all new HIV diagnoses in 2022 were among Gay and Bisexual Men, despite comprising 2% of the U.S. population.
Newer changes in policy, like the Affordable Care Act and same-sex marriage legalization, have reduced some barriers to accessing health insurance (HIV.gov); however, many LGBTQ individuals still experience difficulty paying for medical treatment (Center for American Progress).
Understanding health disparities related to race, gender, sexuality, age, ZIP Code, and other factors and how they impact HIV prevention, diagnoses, and care can help inform research, policies, and programs.
AIDSVu has several resources to help understand the intersection of social determinants of health, the HIV epidemic in the U.S., and PrEP use across multiple geographic locations and different demographic groups.
5 Ways to Use AIDSVu
View local statistics
National-, state-, and city-level profiles including data on social determinants of health.
Learn MoreExplore maps
Interactive maps including social determinants of health and other comparison maps.
Learn MoreShare infographics
Infographics presenting insights on the social determinants of health mapped on AIDSVu.
Learn MoreFor More Information
Learn more about the health disparities and HIV with these resources.