Patrick Sullivan, DVM, PhD, Professor, Department of Epidemiology, Rollins School of Public Health, Emory University, and Principal Scientist for AIDSVu.
Q: A lot of your research has centered on PrEP and how to increase PrEP use among people with indications for PrEP in the U.S. Why is this an important topic to focus on right now?
Pre-Exposure Prophylaxis, or PrEP, is a frequent topic of conversation on National Gay Men’s HIV/AIDS Awareness Day. PrEP is widely accepted as an extremely effective method of preventing HIV, but PrEP use is far lower than you would expect. According to CDC, there are approximately 1.2 million people who could benefit from PrEP, yet we are nowhere near that number in the U.S. There have been significant increases in PrEP use over the years. Since 2012, PrEP use has increased by 1,700%. These increases, however, are not consistent geographically or demographically. We know that PrEP is not getting to all the communities where it is needed most, so we continue to talk about it and continue to research better ways to target PrEP-specific interventions.
The Ending the HIV Epidemic (EHE) initiative includes PrEP coverage as one of the six indicators for tracking progress towards ending the U.S. HIV epidemic by 2030, underscoring the importance of progressing towards greater PrEP use in order to end the HIV epidemic.
Q: In a recent paper in Annals of Epidemiology, Methods for county-level estimation of pre-exposure prophylaxis coverage and application to the U.S. Ending the HIV Epidemic jurisdictions, you used the PrEP-to-MSM ratio to talk about PrEP use and PrEP need in the U.S. What is the PrEP-to-MSM ratio and why is it a useful way to think about this data?
The PrEP-to-Men who have Sex with Men Ratio (PMR) compares the number of male PrEP users to the estimated number of men who have sex with men. PMR is calculated by dividing the number of male PrEP users in 2018 by the estimated number of men who have sex with men (MSM) in 2018 multiplied by 1,000. Because PrEP is a highly effective way of preventing HIV and is an important prevention method for high risk groups, including MSM, visualizing this ratio allows people to see how well PrEP is meeting the needs of MSM. Below you can see what PMR looks like across the U.S. and how widely PrEP use can range among MSM.
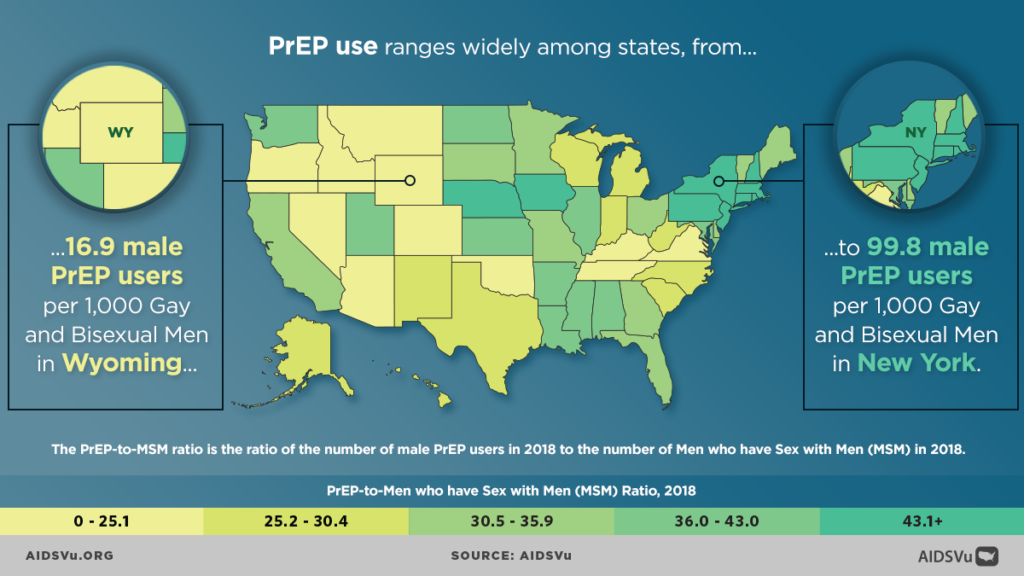
Visualizing PrEP use among MSM gives us a sense of where PrEP need is being met and where more robust PrEP interventions need to be targeted. In the graphic above, areas with darker shades of green have more coverage of PrEP protection among MSM. For instance, about 10% of all MSM in New York state are on PrEP. Compare that to a state like Wyoming, where only about 1.7% of all MSM are on PrEP. The South is a region where traditionally there is a greater unmet need for HIV services, and you can see that reflected in the Southern region’s PMR (29.9) as well.
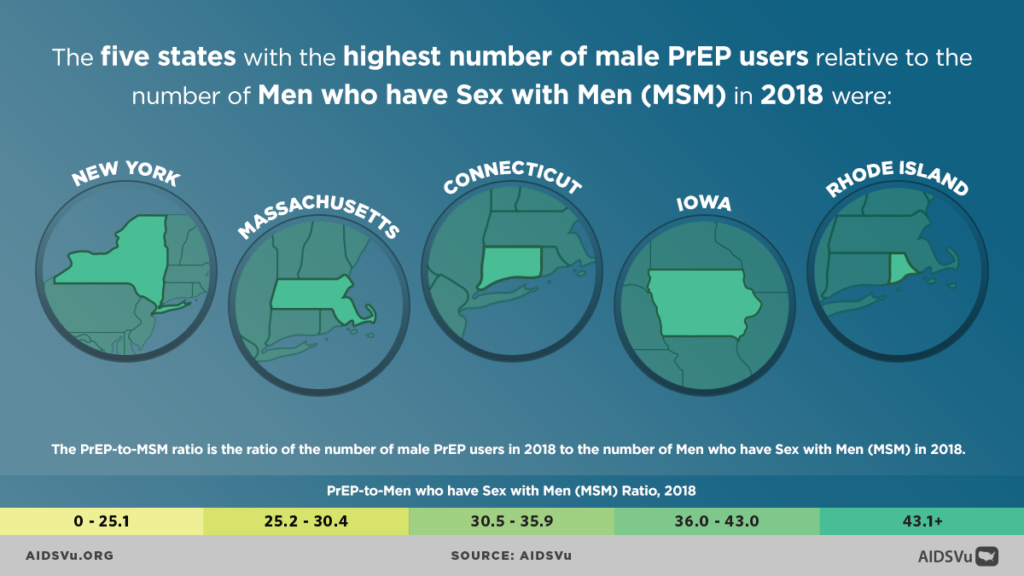
Looking at this graphic, you can see more directly that the Northeast generally has a higher PMR, although other states, like Iowa, have a high ratio as well. Looking at maps like this underscores the importance of finding unique ways to visualize HIV data. It is one thing to tell people that PrEP use varies widely across the country, but it really hits home when you can show them. This is especially true when we are visualizing the HIV epidemic among certain communities and in certain regions.
Q: September 27th is National Gay Men’s HIV/AIDS Awareness Day. What would be your message to the HIV community on this awareness day?
PrEP for gay, bisexual, and other MSM who are not living with HIV and HIV treatment for those living with HIV are the most effective interventions we have to end the HIV epidemic in America. We must continue to find ways to reach people who would benefit from PrEP, especially those most underserved, and we must keep finding innovative ways to make PrEP more available. We must strive to make HIV testing convenient, streamline pathways to care for those living with HIV, push for Medicaid expansion, and minimize barriers to HIV care for all those living with HIV. If we do these things, we will see a significant impact on new HIV diagnoses and on the health of those living with HIV.