Understanding the Transgender Experience
Transgender is an umbrella term for persons whose gender identity or expression (masculine, feminine, other) is different from their sex assigned at birth. Nearly 1 million people (0.3%) identify as transgender in the United States, representing a diverse community that includes transgender women, transgender men, and individuals with additional gender identities who do not identify as male, female, transgender woman, or transgender man.
Transgender people have long been subjected to pervasive stigma, discrimination, and violence across multiple institutions and social contexts. In the United States, this discrimination extends deeply into the healthcare system, creating profound barriers to accessing quality medical care and preventive services. These structural inequities have direct and devastating consequences for HIV prevention, testing, treatment, and care outcomes within transgender communities.
The intersection of anti-transgender bias with other forms of discrimination—including racism, poverty, and criminalization—creates particularly acute vulnerabilities for transgender people of color, transgender people experiencing homelessness, transgender sex workers, and transgender people involved in the criminal justice system.
The Critical Data Gap
One of the most significant challenges in addressing HIV among transgender people has been the profound lack of comprehensive, accurate data. This data invisibility is not accidental but rather reflects systematic exclusion from surveillance systems, research studies, and healthcare data collection practices. For decades, transgender people have been either completely invisible in HIV data or misclassified according to sex assigned at birth, making it impossible to understand the true scope and nature of the epidemic within transgender communities.
Recently, the CDC has begun including gender identity in addition to sex assigned at birth in HIV surveillance reporting from the National HIV Surveillance System. However, these data are known to significantly undercount HIV cases among transgender people for several structural reasons:
Provider Training Gaps: The CDC states that “few health care providers receive proper training or are knowledgeable about transgender health issues and their unique needs.” This lack of competency extends to data collection practices.
Systematic Under-Collection: Most healthcare providers and facilities do not systematically collect information on both sex assigned at birth and current gender identity, leading to misclassification or complete omission of transgender individuals from surveillance data.
Healthcare Avoidance: Due to experiences of discrimination, harassment, and inadequate care, many transgender people avoid healthcare settings entirely, remaining invisible to surveillance systems.
Documentation Barriers: Inconsistencies between identity documents and lived identity can create complex barriers to accurate data collection and reporting.
This data invisibility has profound consequences for public health planning, resource allocation, program development, and policy advocacy for transgender communities affected by HIV.
The Disproportionate Impact: What We Know
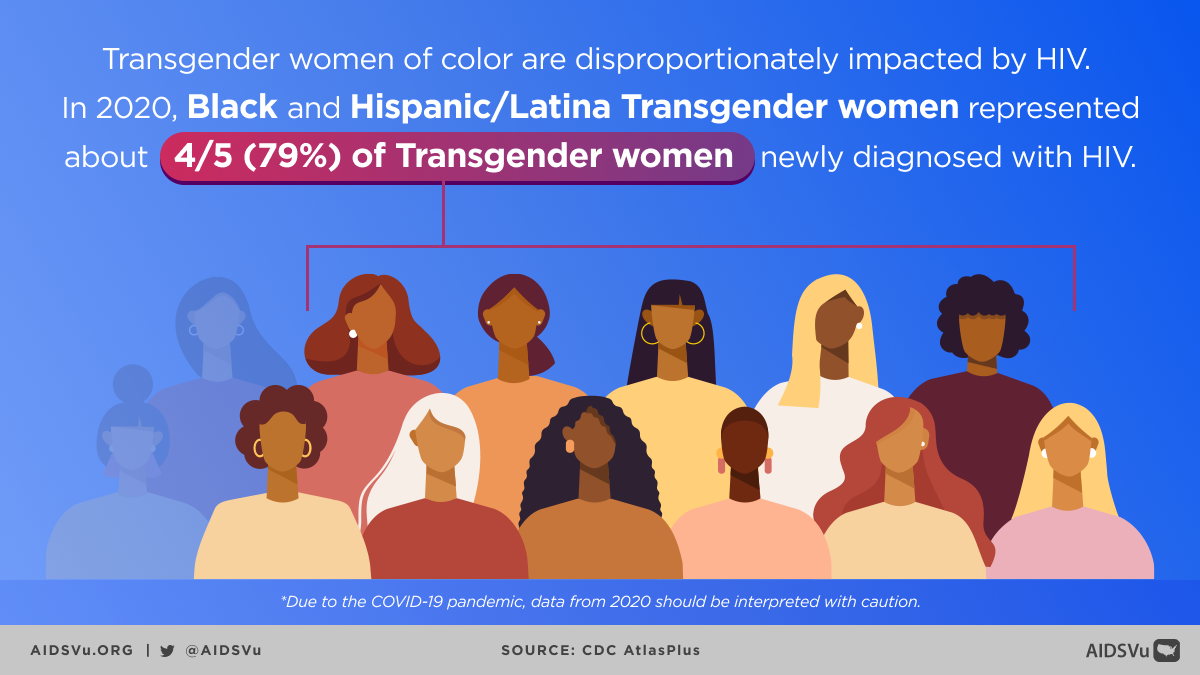
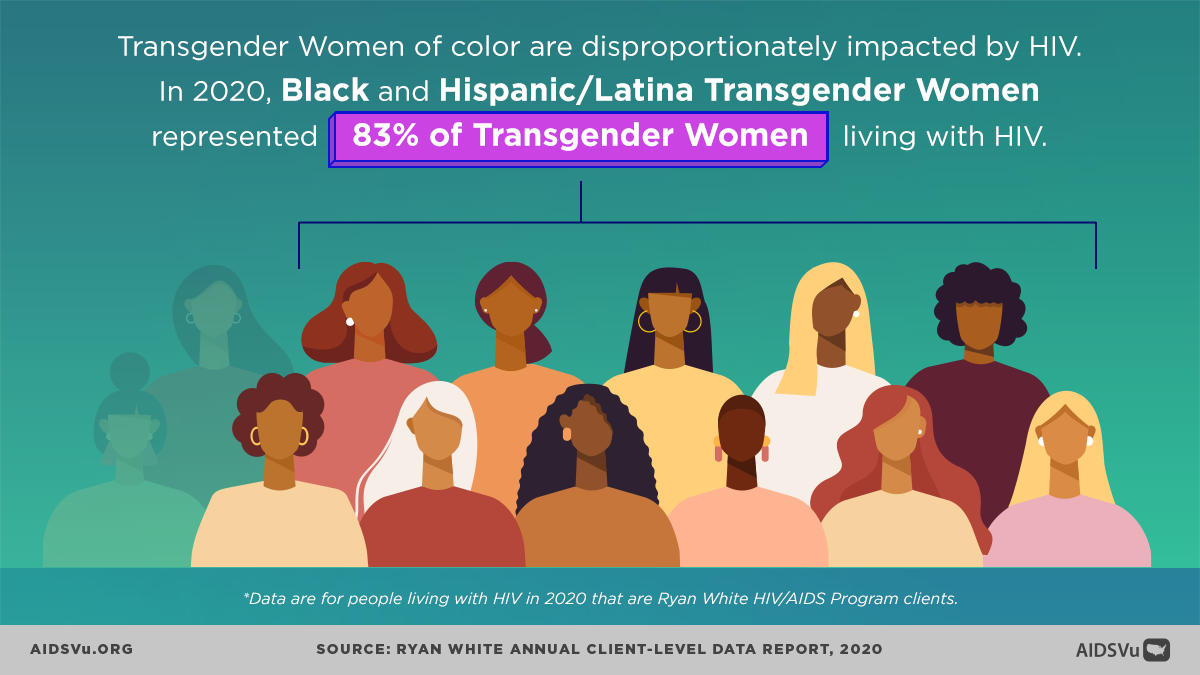
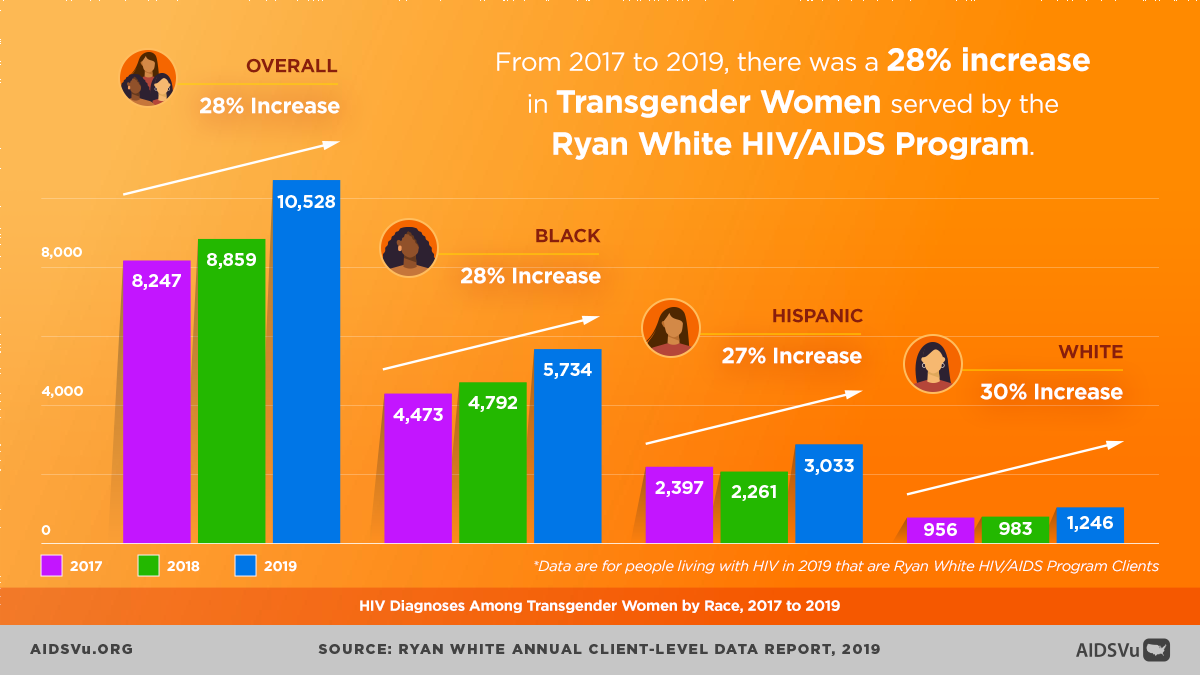
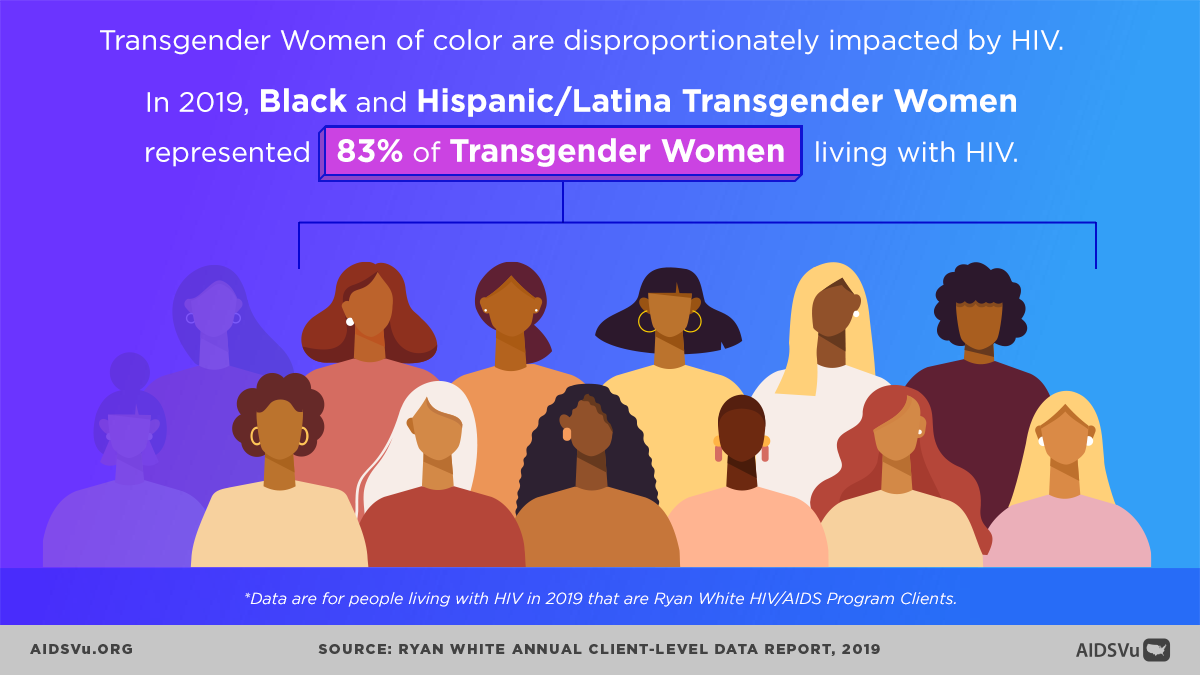
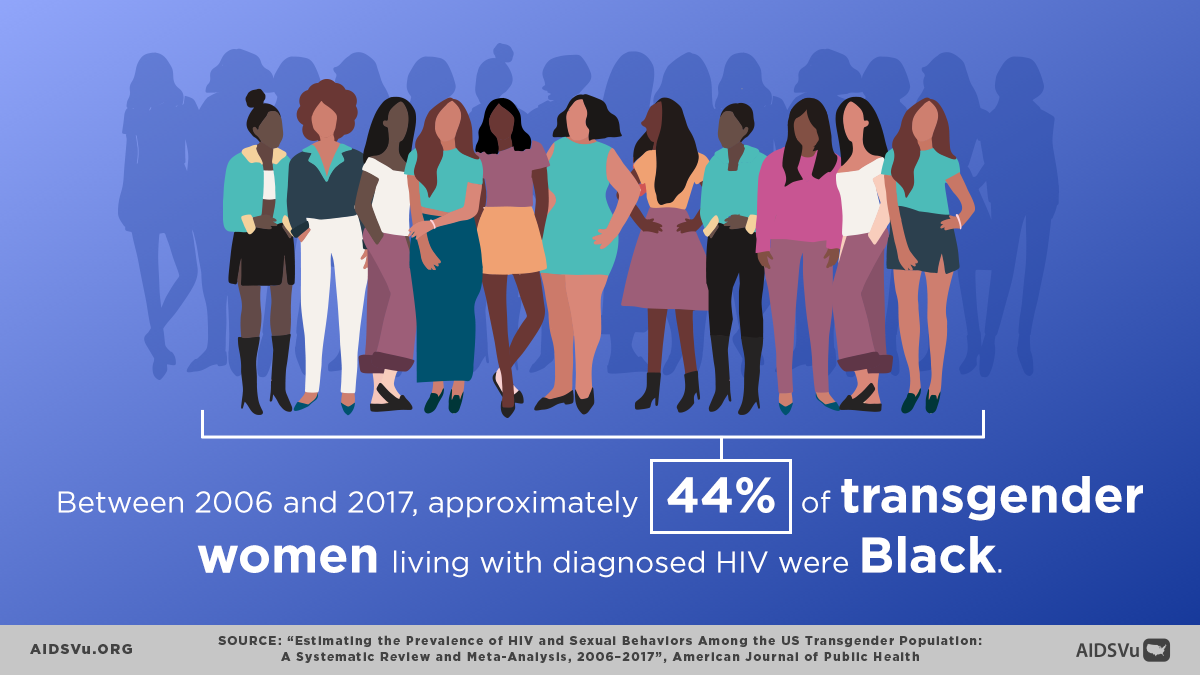
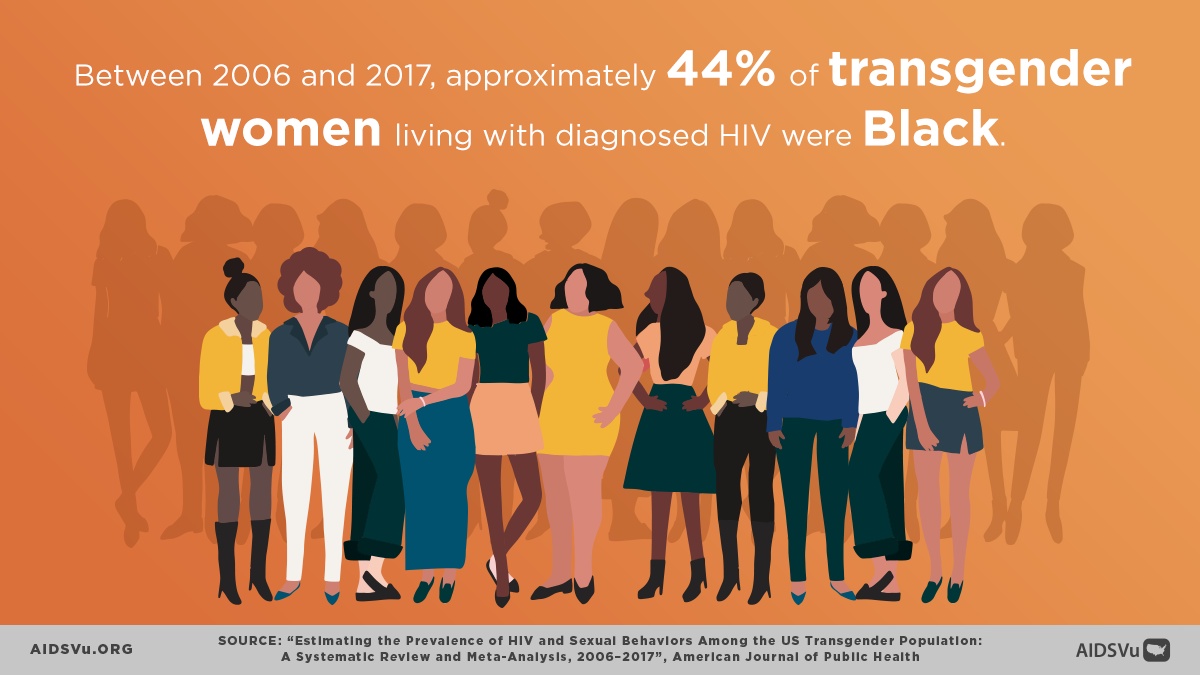
Despite data limitations, available evidence reveals that transgender people—particularly transgender women and especially Black and Latina transgender women—face extraordinarily high rates of HIV infection that far exceed those seen in the general population.
HIV Diagnoses and Demographics
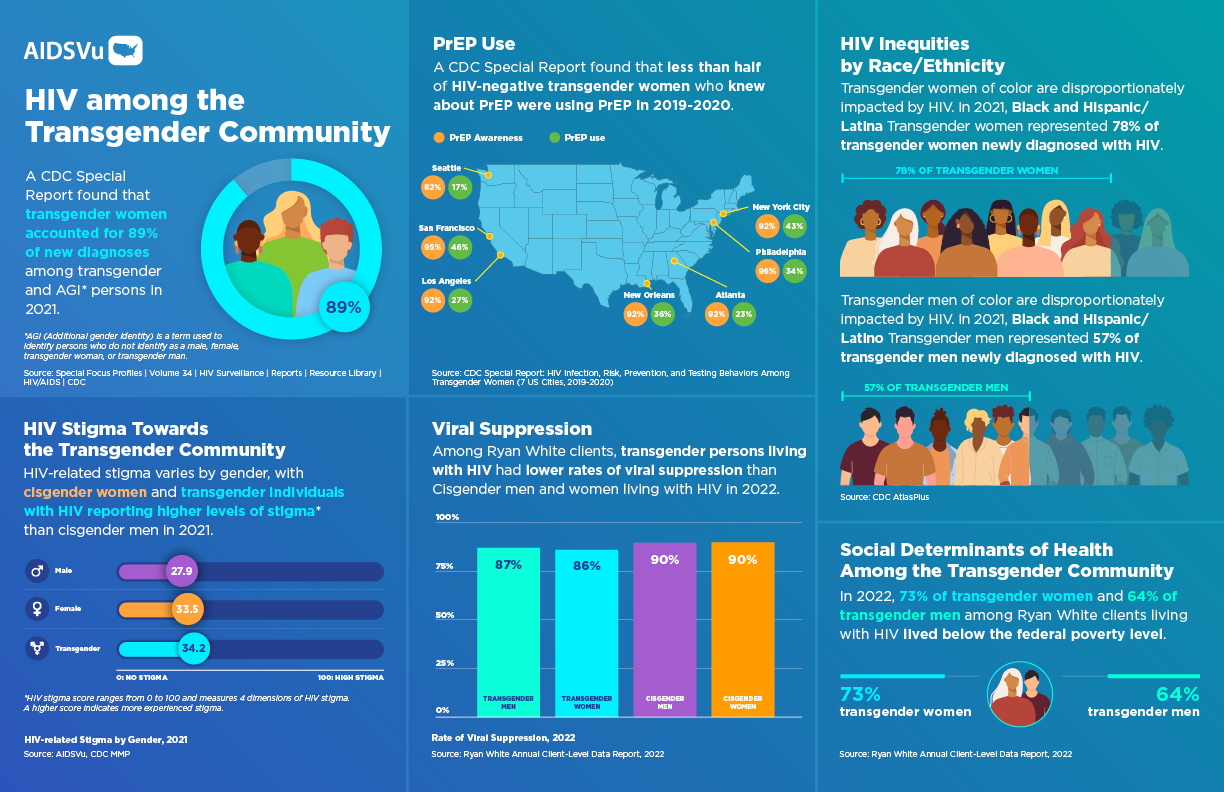
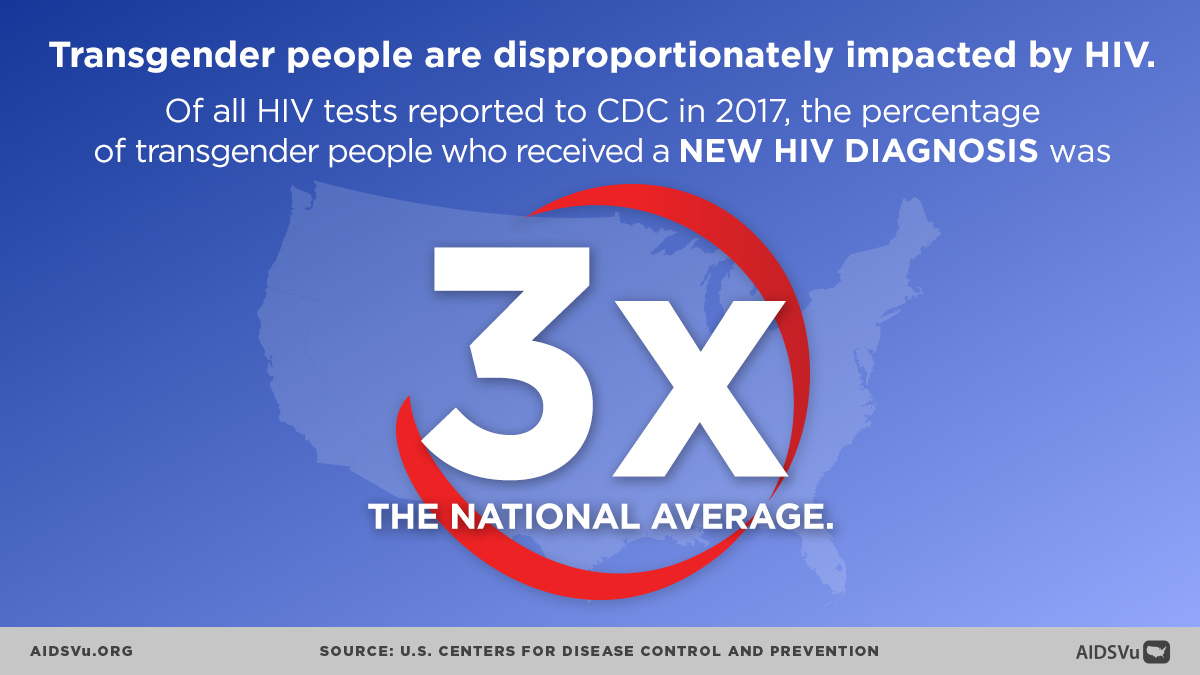
In 2022, transgender people accounted for 2% (928) of the 37,981 new HIV diagnoses, with transgender women accounting for 2% (869) of new HIV diagnoses. While transgender people represent approximately 0.3% of the U.S. population, they account for a disproportionate share of new HIV diagnoses.
Breaking down the data from available surveillance:
- Gender Distribution: In 2021, transgender women accounted for 89% of new diagnoses among transgender and additional gender identity (AGI) individuals
- Racial Disparities: In 2021, Black and Hispanic/Latina transgender women represented 78% of transgender women newly diagnosed with HIV
- Transgender Men: In 2021, Black and Hispanic/Latino transgender men represented 57% of transgender men newly diagnosed with HIV
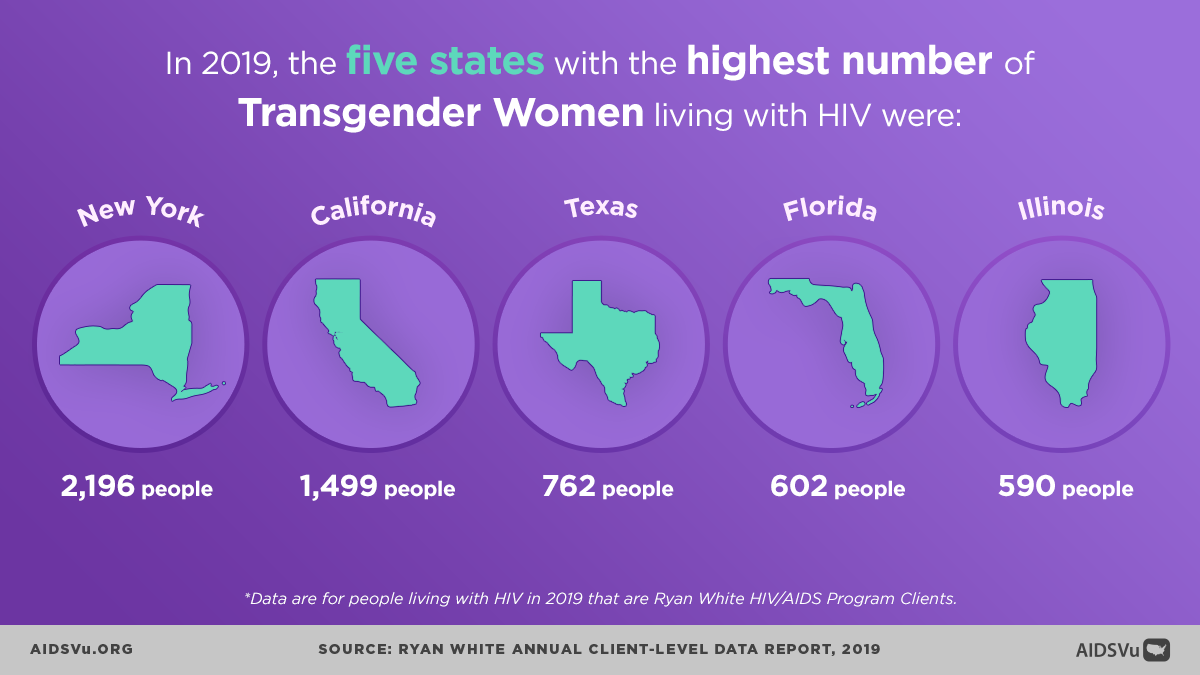
Geographic Patterns
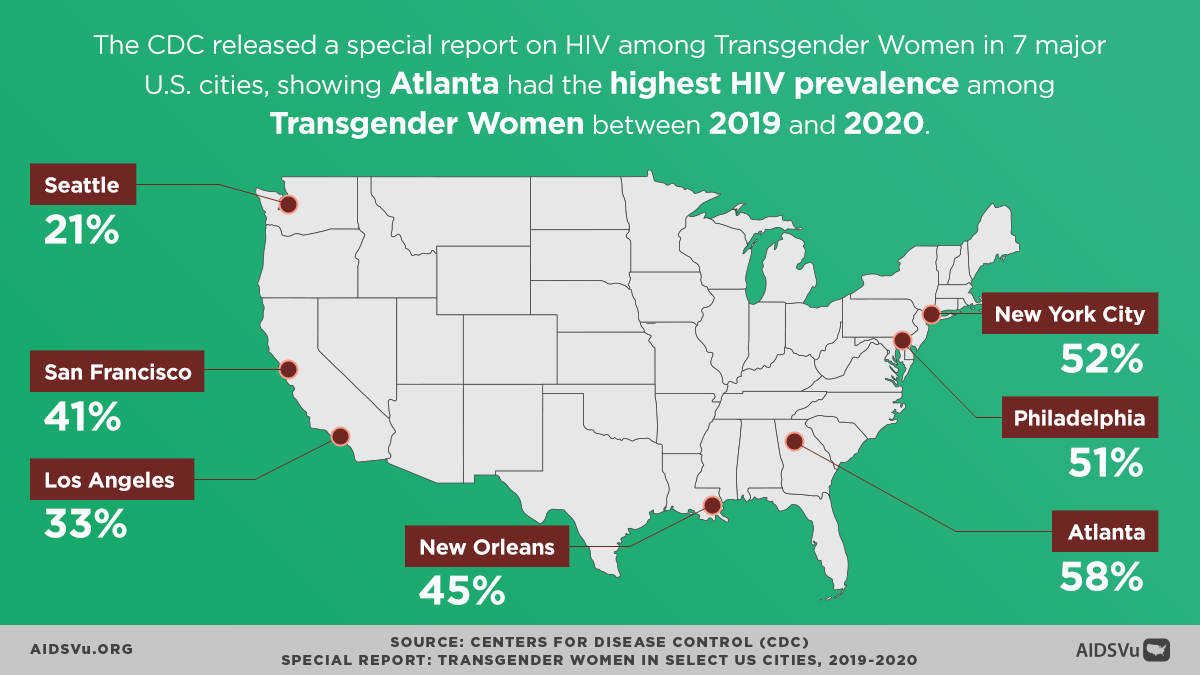
HIV diagnoses among transgender people follow distinct geographic patterns that reflect both population distribution and regional variations in stigma, healthcare access, and supportive policies. The highest number of new HIV diagnoses among transgender people were in the South, followed by the West, Northeast, and Midwest respectively.
This concentration in the South is particularly concerning given the region’s documented challenges with HIV care infrastructure, higher levels of stigma and discrimination, and more limited protections for LGBTQ+ people in general and transgender people specifically.
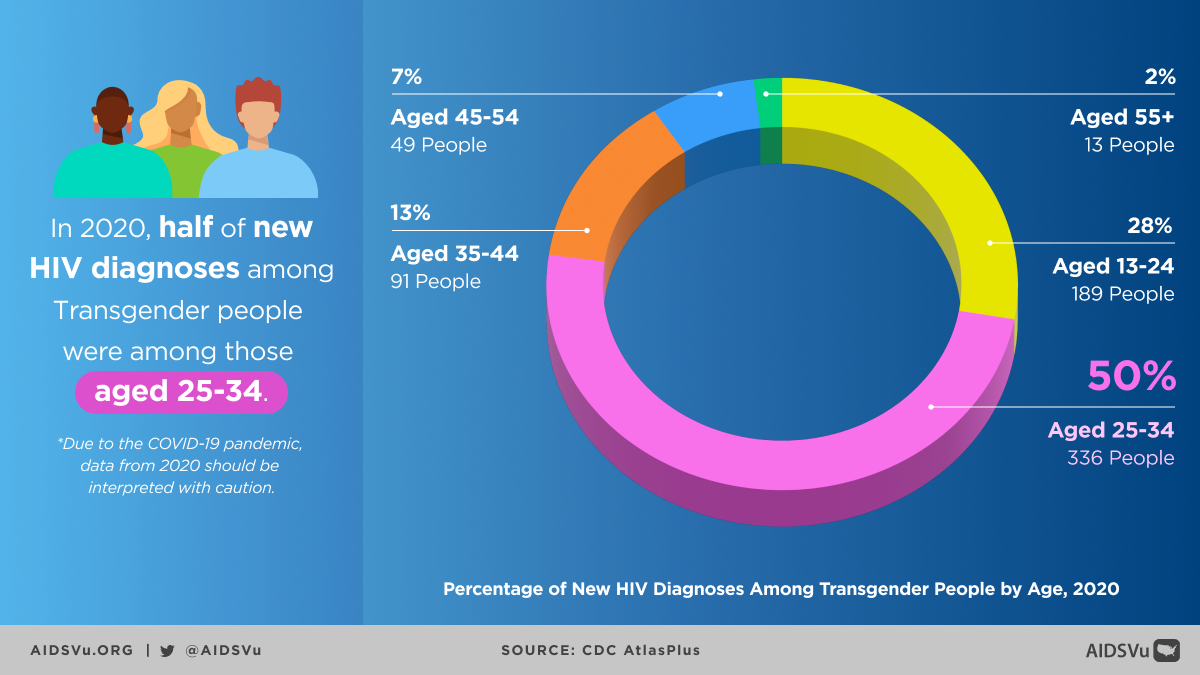
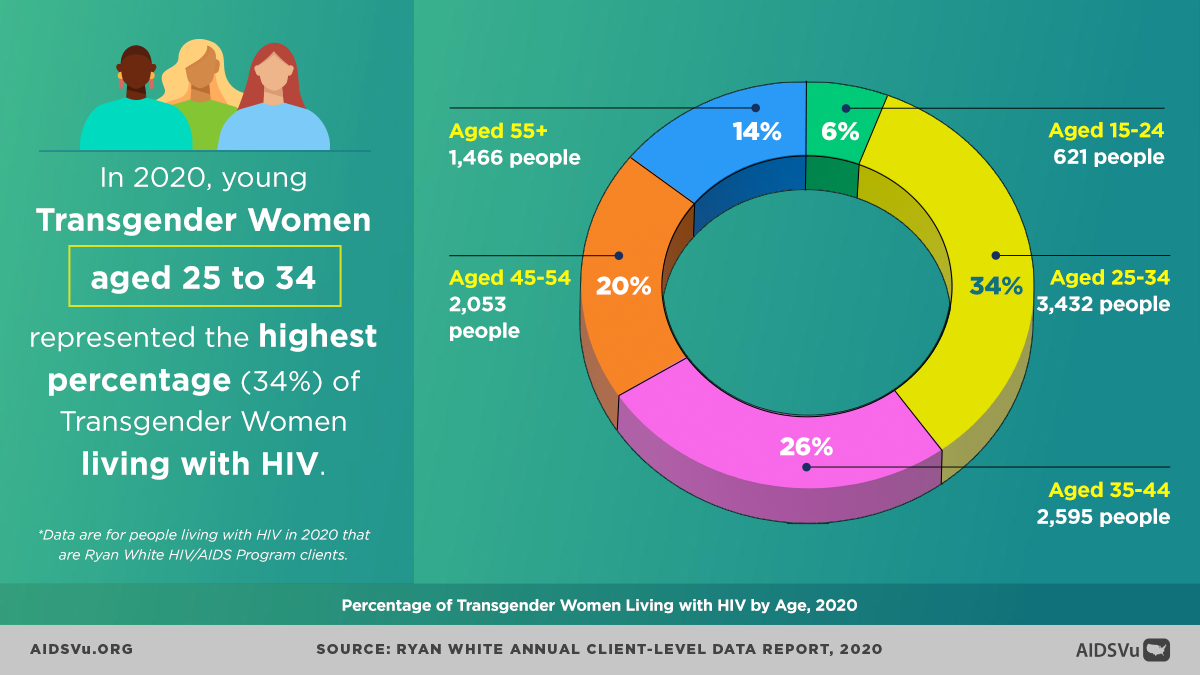
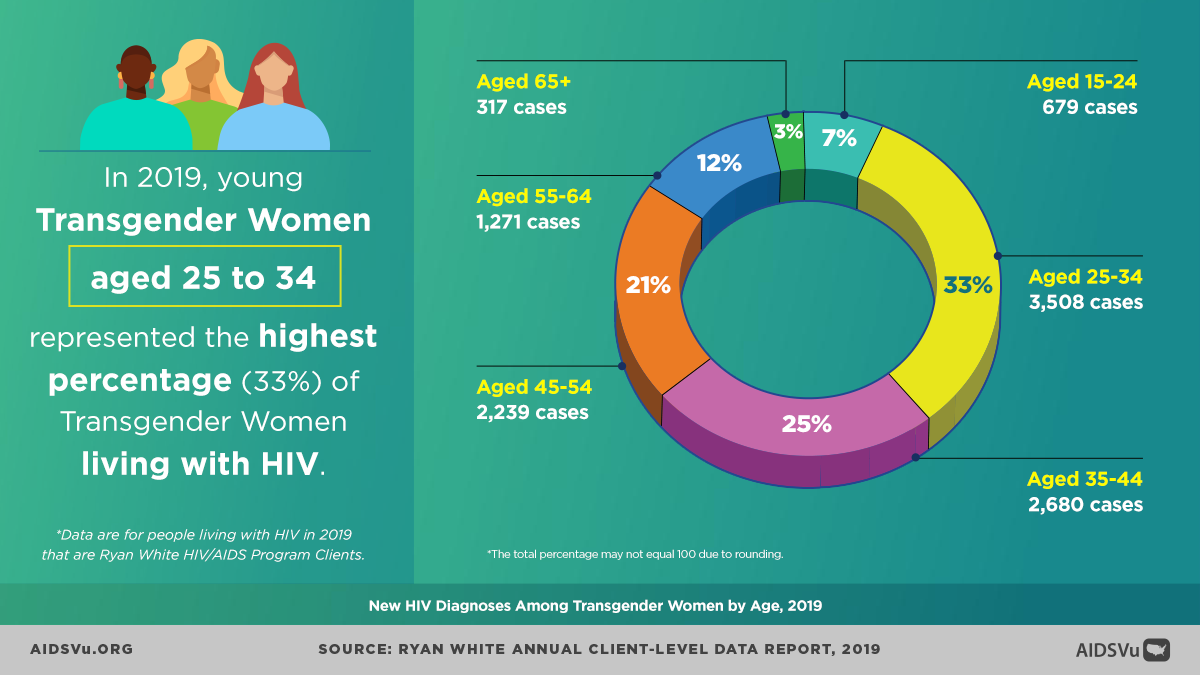
Age-Related Trends
Among transgender people, most new HIV diagnoses were among people aged 25 to 34, followed by people aged 13 to 24. However, trend data from 2015-2019 reveals concerning patterns: People 55 and older saw the largest increase in diagnoses, followed by people aged 25 to 34 and 35 to 44.
This suggests that HIV acquisition continues across the lifespan for transgender people, possibly reflecting ongoing barriers to prevention services, sustained risk factors, or cohort effects from earlier periods with even more limited HIV prevention resources.
Structural Determinants of Health: The Root Causes
The extraordinarily high rates of HIV among transgender people, particularly transgender women of color, cannot be understood without examining the structural factors that create and sustain vulnerability. These are not individual risk factors but rather systematic forms of exclusion and marginalization that operate across multiple domains of life.
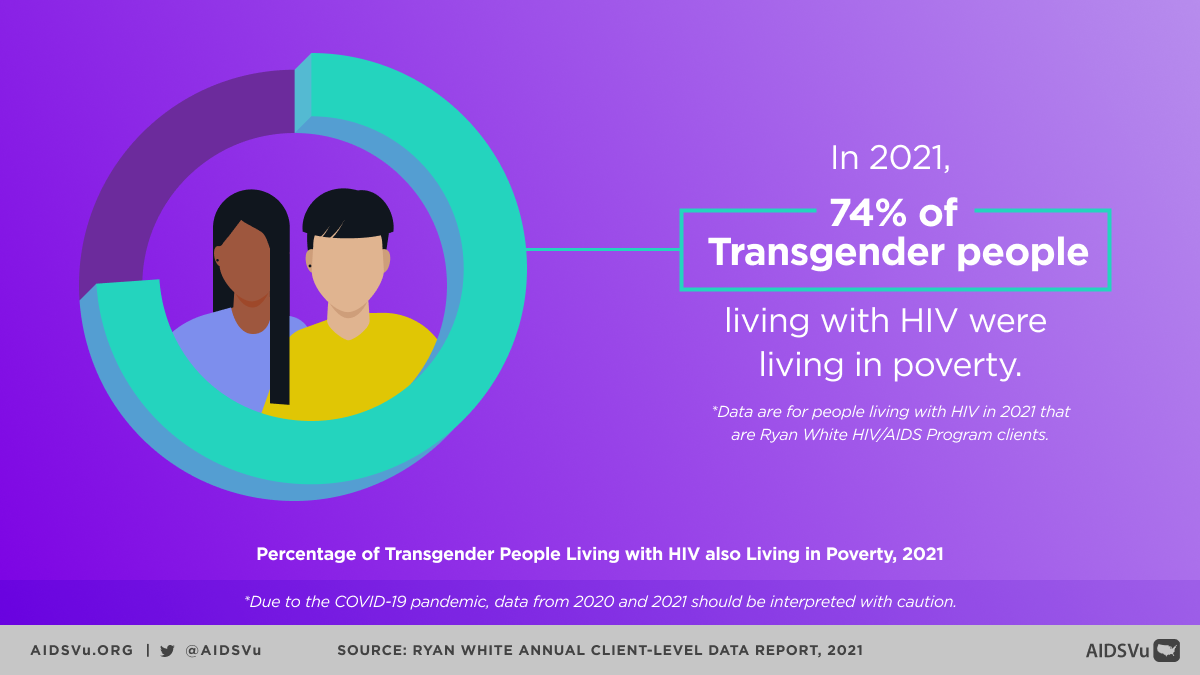
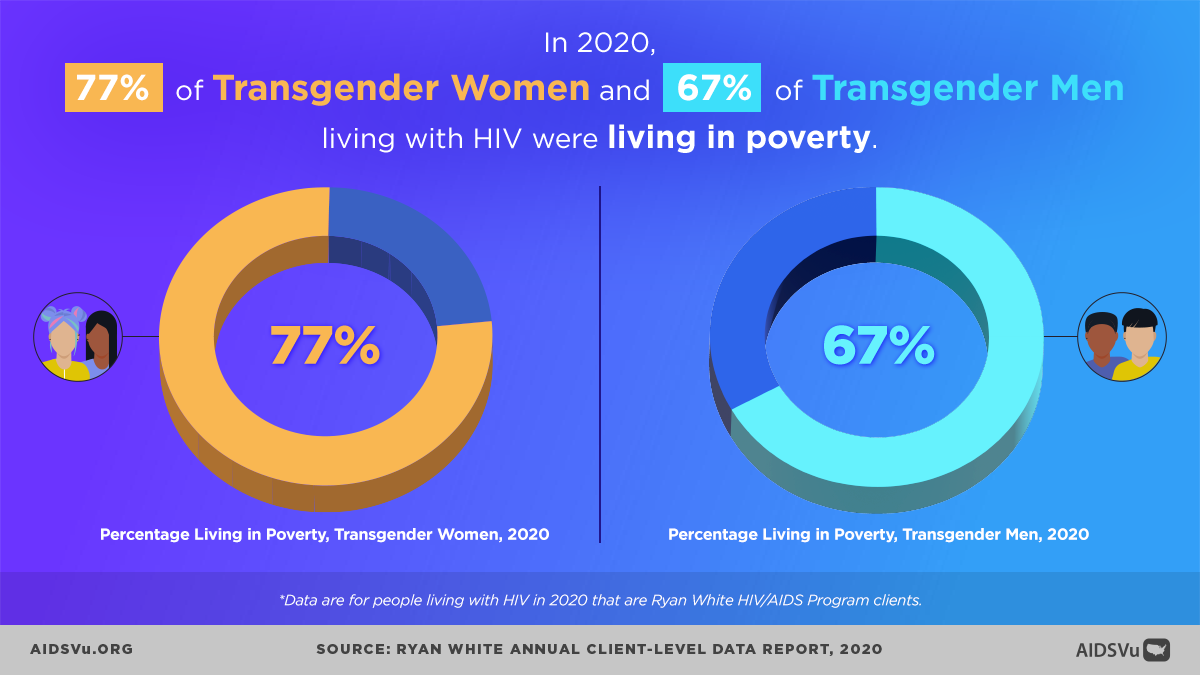
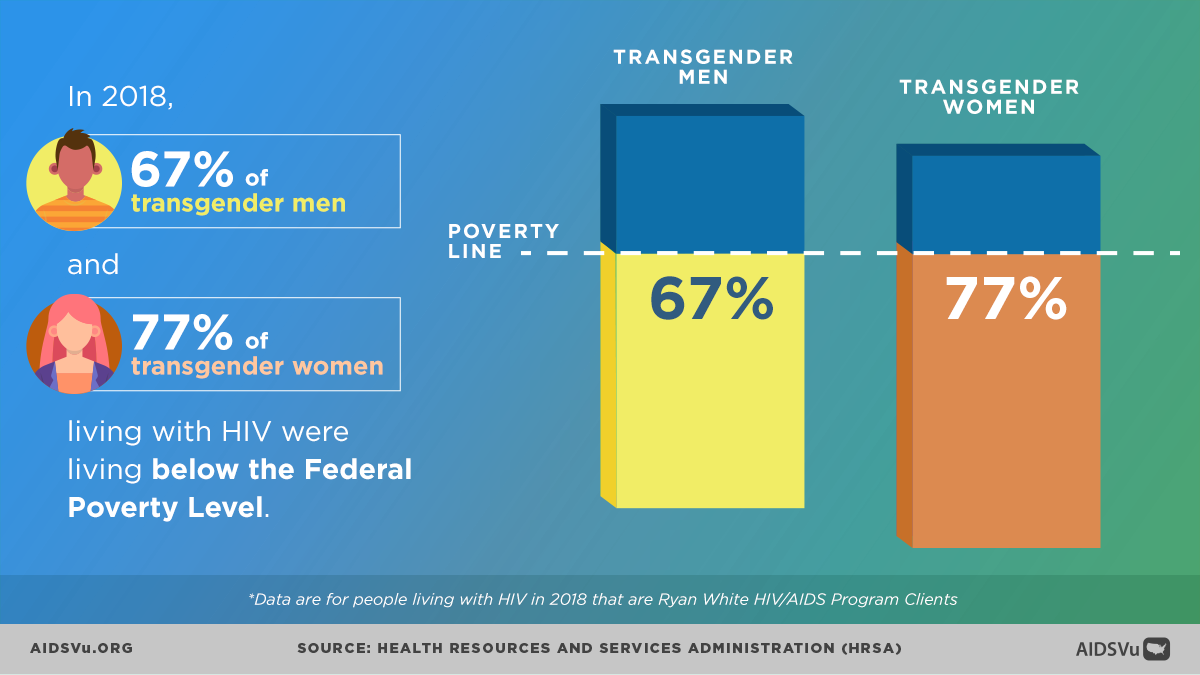
Economic Marginalization
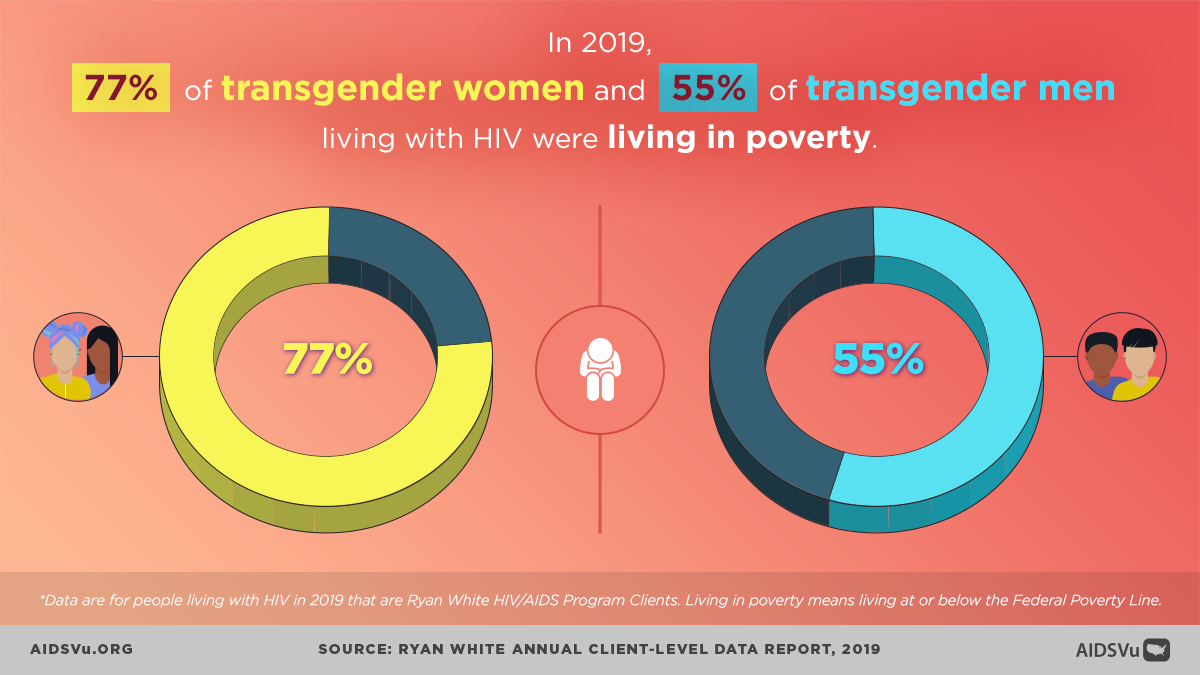
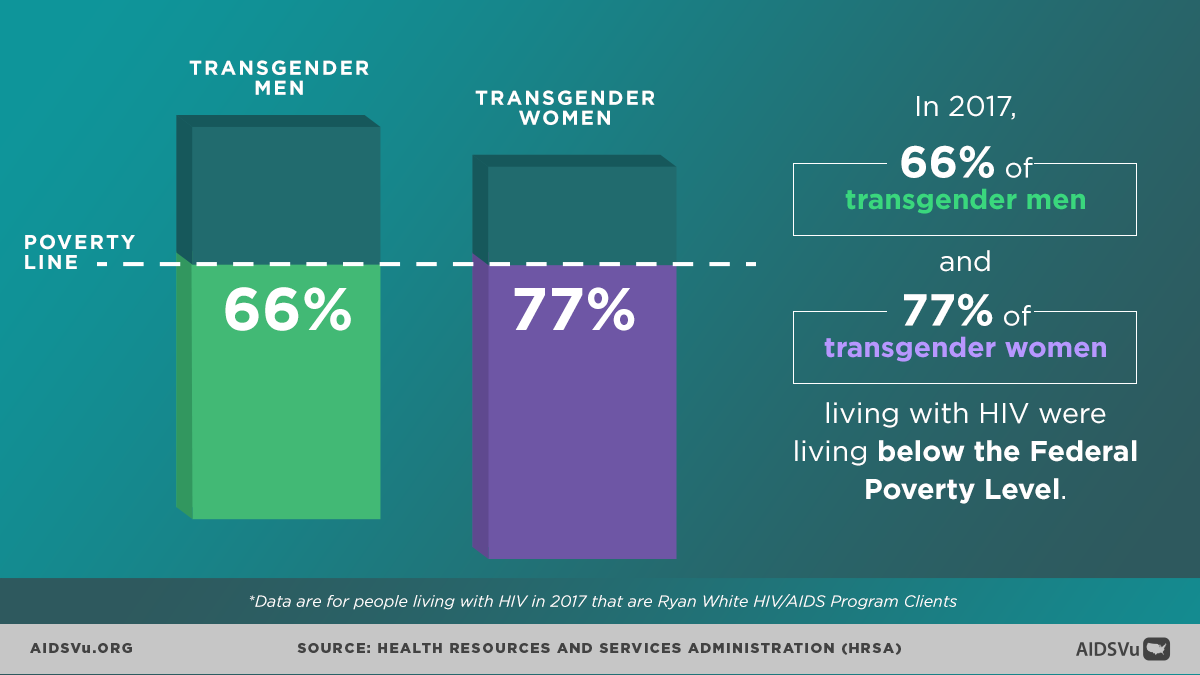
According to data from the Ryan White HIV/AIDS Program, in 2022, 73% of transgender women and 64% of transgender men living with HIV lived below the federal poverty level. This economic marginalization stems from:
- Employment discrimination that pushes transgender people out of formal employment sectors
- Educational barriers resulting from harassment and exclusion in schools and higher education
- Family rejection leading to loss of economic support networks
- Criminal justice involvement that further limits employment opportunities
Housing Instability and Homelessness
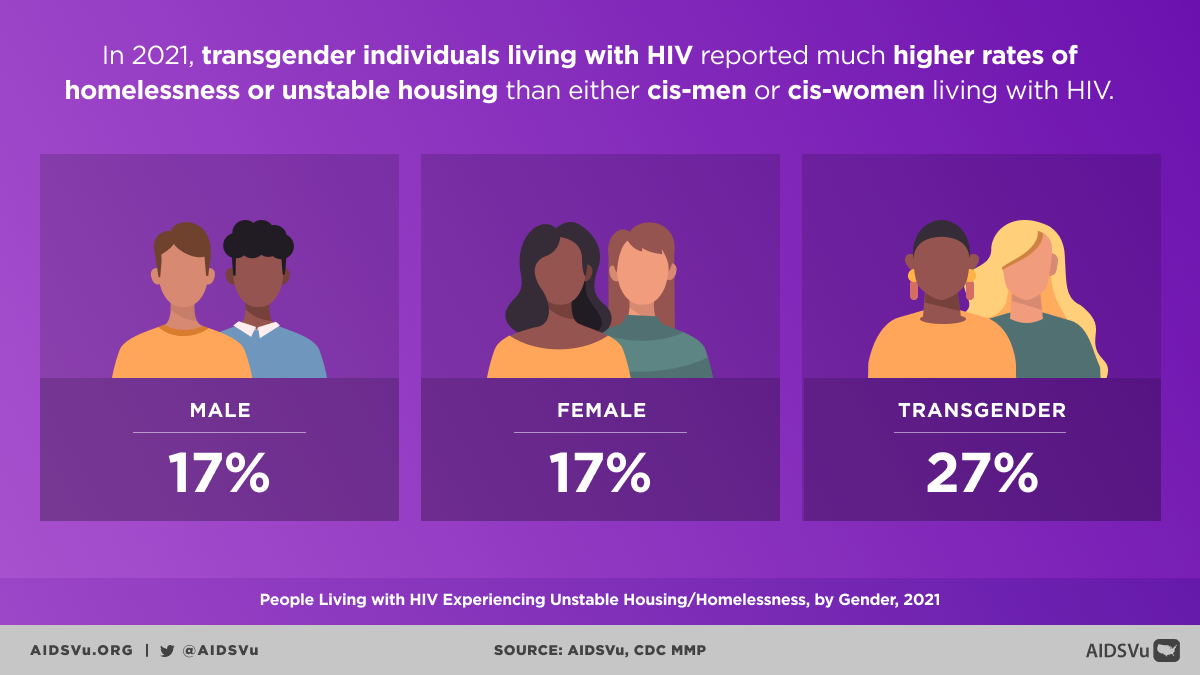
In 2021, 27% of transgender individuals living with HIV were homeless or experienced unstable housing according to Ryan White data. Additional CDC data shows that 29 percent of transgender people with HIV reported homelessness in the past 12 months, compared to 8 percent of all people with HIV.
Housing instability creates cascading risks for HIV acquisition and poor health outcomes by:
- Forcing individuals into survival situations that may increase HIV risk
- Disrupting continuity of healthcare and treatment
- Limiting ability to store medications safely
- Increasing exposure to violence and exploitation
Healthcare Discrimination and Barriers
The healthcare system represents a critical site where transgender people experience discrimination that directly affects HIV outcomes. Key barriers include:
Provider Bias and Incompetence: Many healthcare providers lack training in transgender health and may demonstrate explicit or implicit bias, leading to inadequate or inappropriate care.
Insurance and Coverage Barriers: Many transgender people lack health insurance, and even those with coverage may find that transgender-specific health needs are excluded.
Geographic Access: In many areas, particularly rural regions, there are no healthcare providers trained in transgender health or HIV care.
Intersectional Discrimination: Transgender people of color, transgender people experiencing homelessness, and transgender people involved in sex work may face multiple forms of discrimination in healthcare settings.
HIV Prevention: PrEP Access and Utilization
Pre-exposure prophylaxis (PrEP) represents a crucial HIV prevention tool, but access and utilization among transgender people remain inadequate despite high awareness levels.
PrEP Awareness vs. Utilization Gap
Data from the CDC’s National HIV Behavioral Surveillance system reveals both encouraging and concerning trends regarding PrEP among transgender women:
92 percent of transgender women without HIV were aware of PrEP, but only 32 percent used PrEP. This dramatic gap between awareness and utilization points to significant structural barriers beyond simple knowledge deficits.
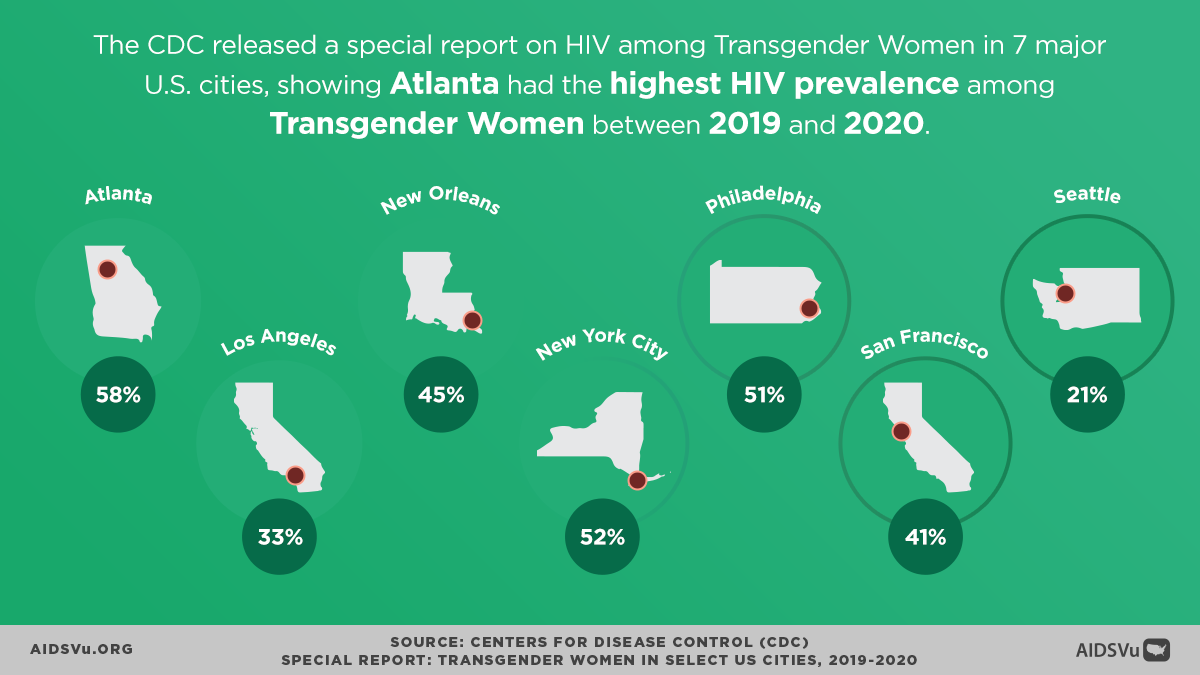
Looking at city-specific data from the CDC’s seven-city study provides additional context:
- High awareness across cities: PrEP awareness ranged from 82% in Seattle to 96% in Philadelphia
- Varied utilization: PrEP use ranged from 17% in Seattle to 46% in San Francisco
- Geographic disparities: The variation in utilization across cities suggests that local factors—including provider availability, insurance coverage, stigma levels, and supportive services—significantly influence PrEP access
Barriers to PrEP Access
Several factors contribute to low PrEP utilization among transgender women despite high awareness:
Provider Knowledge and Competency: Many healthcare providers lack training in both transgender health and HIV prevention, creating barriers to appropriate PrEP prescribing and monitoring.
Insurance and Cost Barriers: Coverage limitations and out-of-pocket costs can make PrEP inaccessible, particularly for transgender people experiencing economic marginalization.
Healthcare Discrimination: Previous experiences of discrimination in healthcare settings may deter transgender people from seeking PrEP services.
Intersectional Stigma: The intersection of HIV stigma and anti-transgender bias can create additional barriers to accessing HIV prevention services.
Medical Mistrust: Historical and ongoing mistreatment by medical institutions may contribute to reluctance to engage with HIV prevention services.
The HIV Care Continuum: Persistent Disparities
While transgender people face significant challenges in HIV prevention, those who acquire HIV continue to experience disparities throughout the HIV care continuum, from diagnosis through viral suppression.
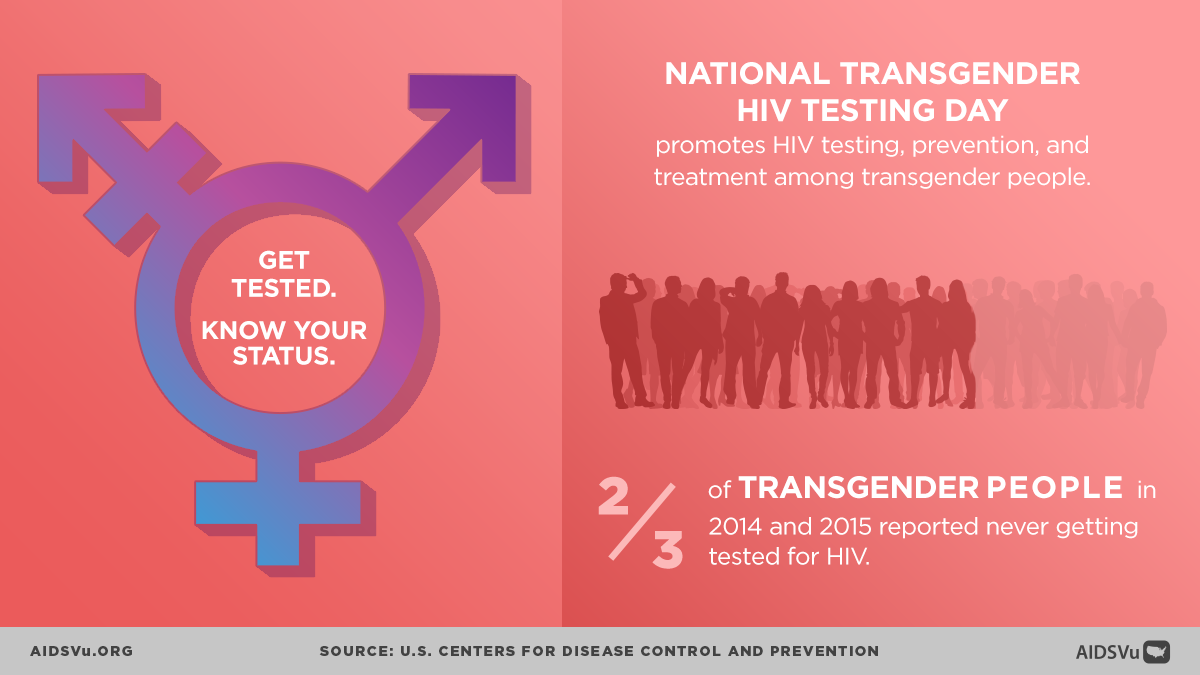
Testing and Diagnosis
96 percent of transgender women had ever tested for HIV, and 82 percent were tested for HIV in the past 12 months, indicating high levels of testing behavior. However, high testing rates among transgender women may also reflect the high prevalence of HIV in this community and the need for frequent monitoring.
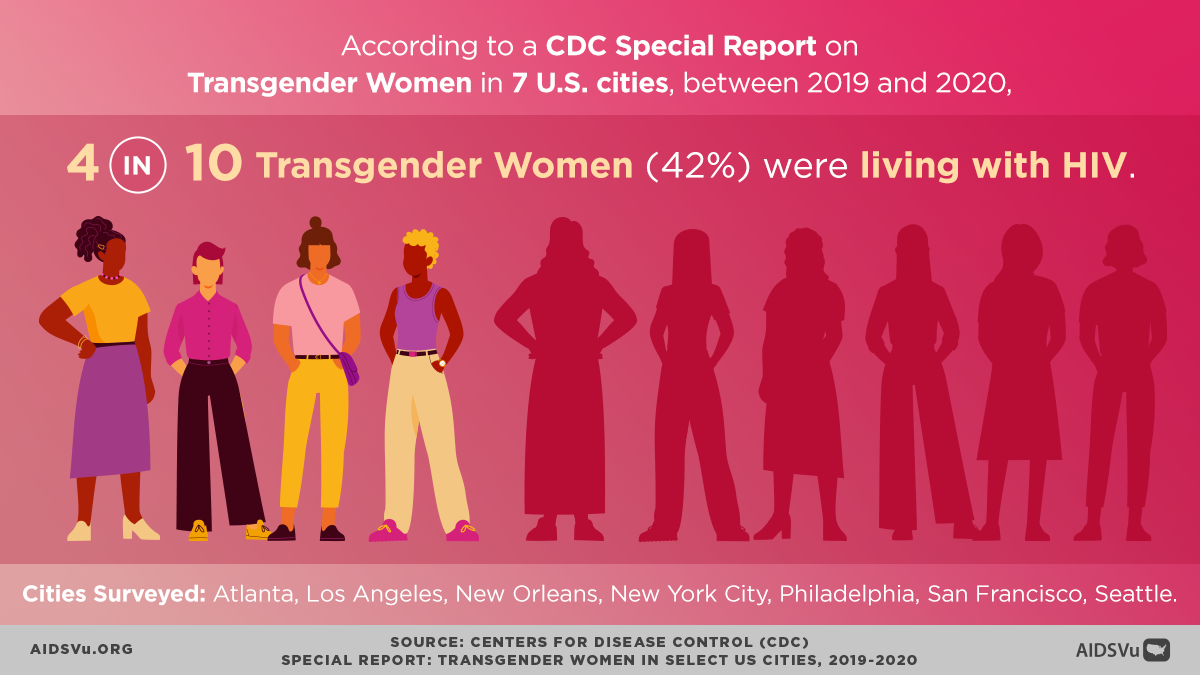
HIV Prevalence
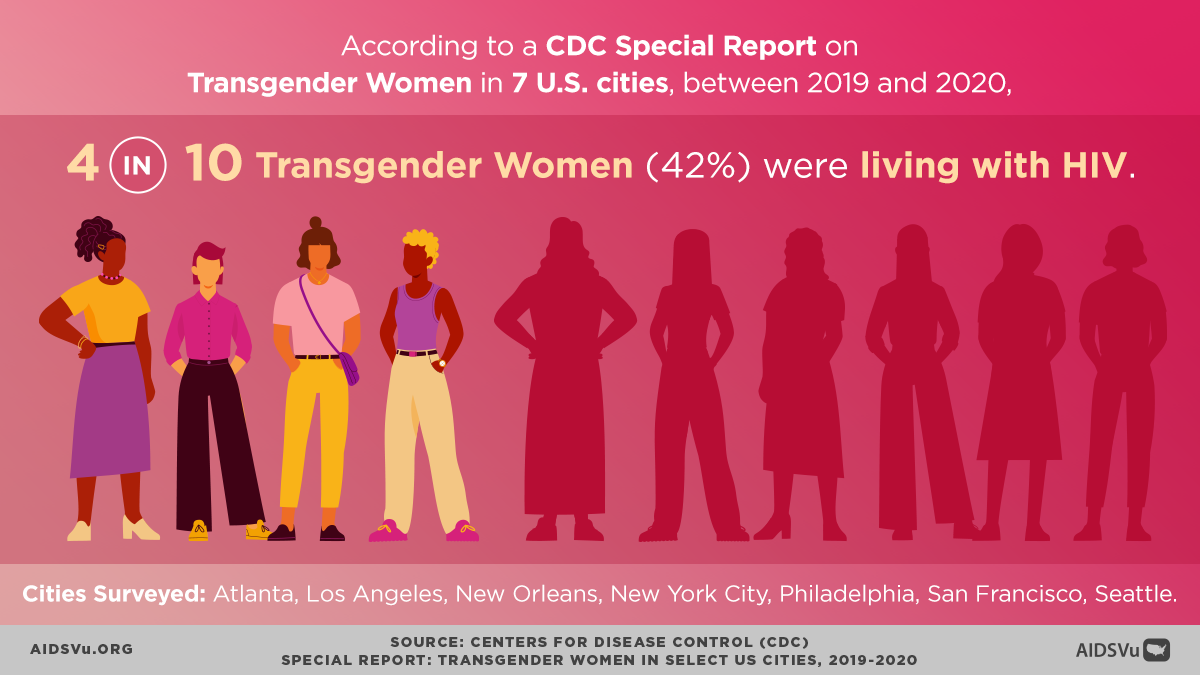
Data from the CDC’s seven-city study reveals stark racial disparities in HIV prevalence among transgender women: Among transgender women interviewed, 42 percent had HIV, with 62 percent of Black/African American transgender women having HIV, 35 percent of Hispanic/Latina transgender women, and 17 percent of White transgender women.
These dramatic differences highlight how racism intersects with transphobia to create particular vulnerability for transgender women of color.
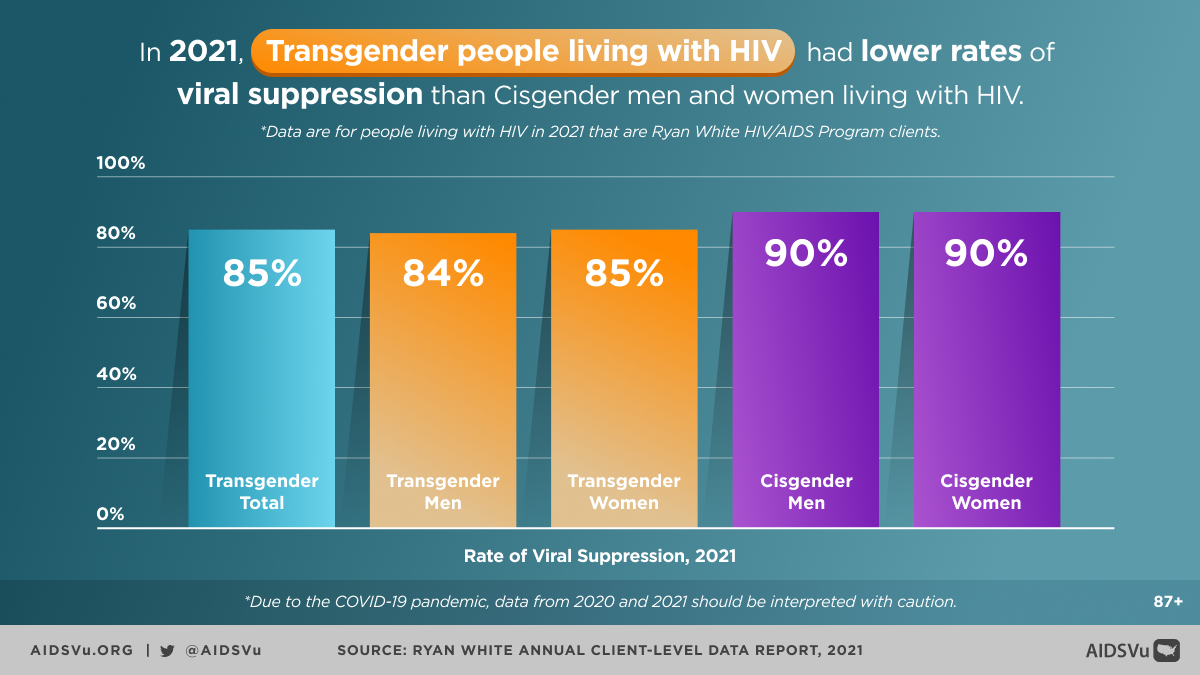
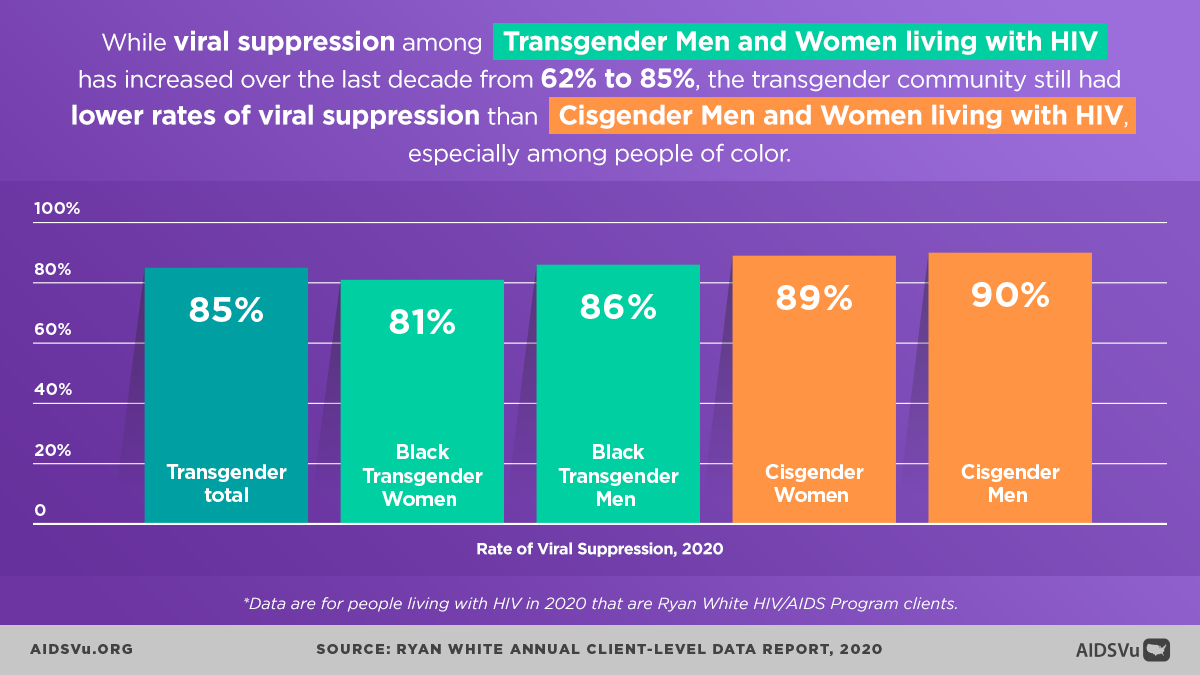
Engagement in Care and Viral Suppression
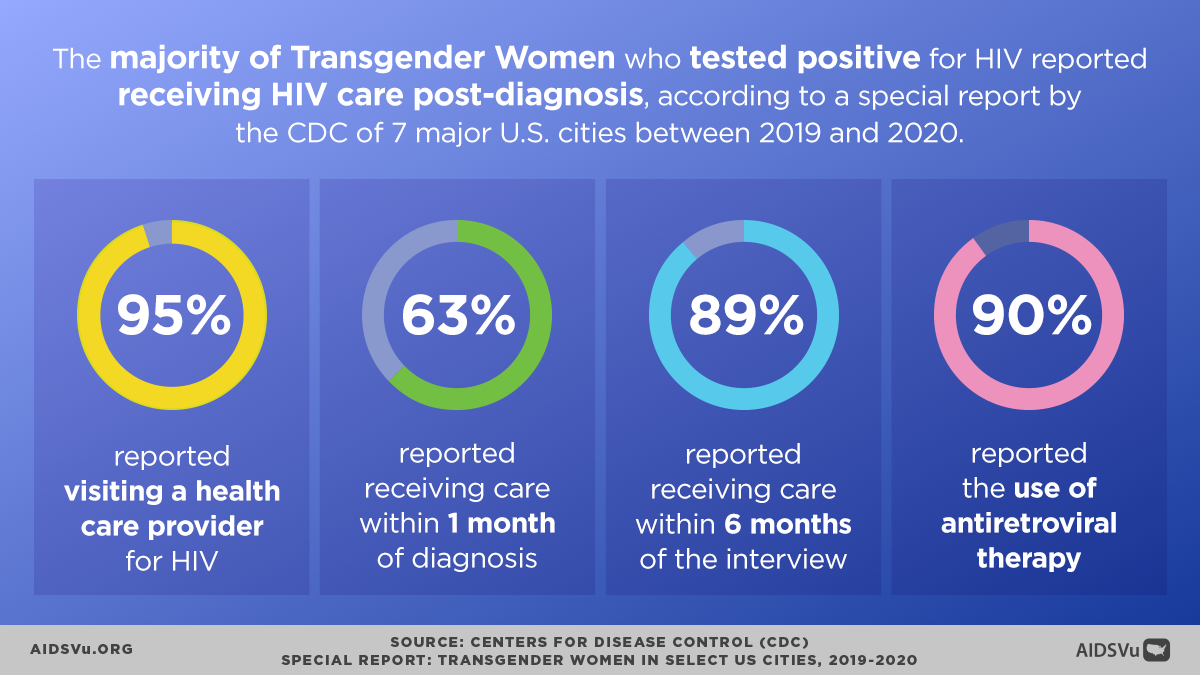
Despite facing significant barriers, transgender people demonstrate relatively strong engagement with HIV care once connected to services:
For every 100 transgender women with diagnosed HIV in 2019, 84 received some HIV care, 67 were retained in care, and 67 were virally suppressed. For every 100 transgender men with diagnosed HIV in 2019, 85 received some HIV care, 65 were retained in care, and 68 were virally suppressed.
Interestingly, these rates are actually higher than the general population of people with HIV, where for every 100 people overall with diagnosed HIV, 76 received some HIV care, 58 were retained in care, and 66 were virally suppressed.
However, data from the Medical Monitoring Project reveals concerning disparities in treatment adherence and care continuity:
- Treatment Adherence: 35 percent of transgender people with HIV reported taking all of their doses of HIV medicine over the last 30 days, compared to 62 percent of all people with HIV
- Missed Appointments: 31 percent of transgender people with HIV missed at least 1 medical appointment in the past 12 months, compared to 20 percent of all people with HIV
These disparities in adherence and care engagement likely reflect the ongoing structural barriers that transgender people face even after entering care.
Mental Health and Psychosocial Challenges
The intersection of HIV and transgender identity occurs within a context of significant mental health challenges stemming from minority stress, discrimination, and social exclusion.
Depression and Anxiety
26 percent of transgender people with HIV experienced symptoms of depression or anxiety in the past 12 months, compared to 19 percent of all people with HIV. This elevated rate of mental health challenges likely reflects:
- Minority stress from anti-transgender stigma and discrimination
- Intersectional stigma from both HIV and transgender-related stigma
- Social isolation due to family rejection and community exclusion
- Trauma from experiences of violence, harassment, and discrimination
HIV Stigma
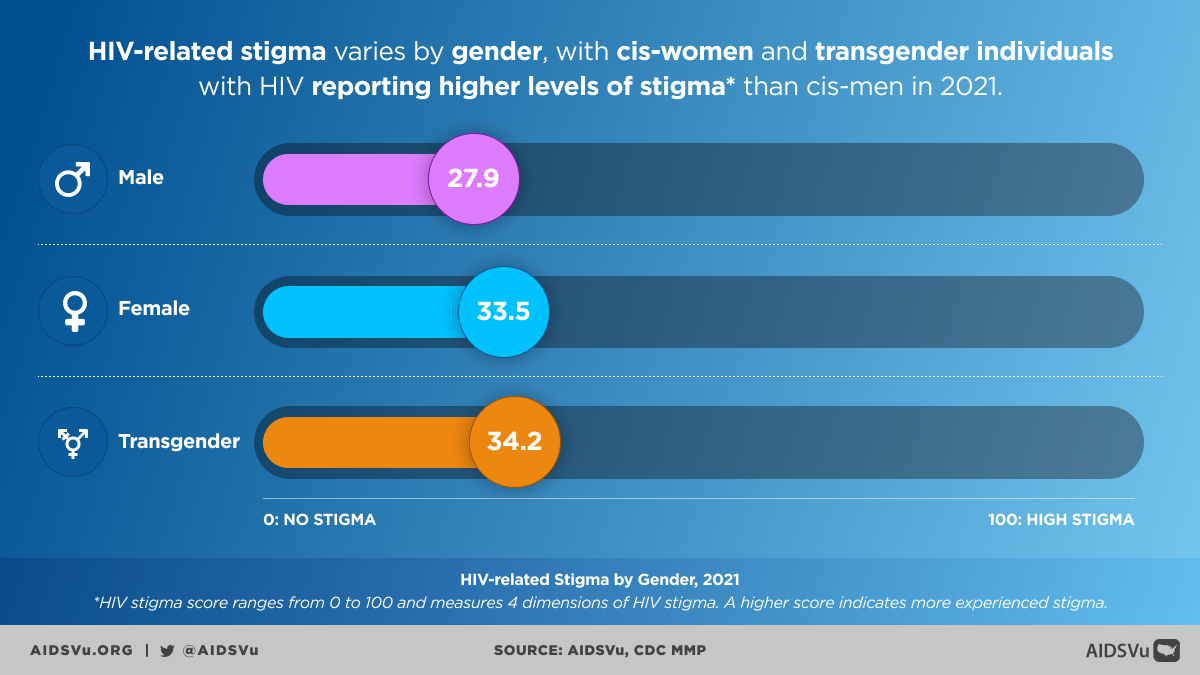
Transgender people with HIV experienced higher levels of HIV stigma, with a median score of 34 on a scale of 1 to 100, compared to 28 for all people with HIV. This elevated stigma may reflect the compounding effects of both HIV-related and transgender-related stigma, creating particularly challenging psychosocial environments.
Service Needs
The top service transgender people with HIV reported needing in 2020 was dental care, with 17 percent saying they needed but did not receive it. The need for comprehensive support services extends beyond medical care to include:
- Mental health services
- Substance use treatment
- Housing assistance
- Legal services
- Peer support programs
- Gender-affirming care
Working Toward Better Data and Surveillance
Recognizing the critical importance of accurate data for effective public health response, CDC and local health departments have implemented several initiatives to improve HIV surveillance data for transgender and gender non-conforming populations:
Data Collection Improvements
Revised Data Collection Procedures: Updates to surveillance systems to capture information on gender identity separate from sex assigned at birth.
Technical Guidance: Comprehensive guidance to health departments on collecting, interpreting, and presenting HIV surveillance data for transgender populations.
Training and Technical Assistance: Ongoing support for health departments to implement best practices in transgender data collection.
Quality Assessment: Regular evaluation of data quality and completeness to identify areas for improvement.
Remaining Challenges
Despite these improvements, significant challenges remain:
Provider Training: Continued need for comprehensive training of healthcare providers in transgender health and appropriate data collection practices.
System Integration: Many electronic health records and surveillance systems still lack adequate fields for collecting and transmitting gender identity information.
Standardization: Need for consistent definitions and categories across different surveillance systems and jurisdictions.
Community Trust: Building trust with transgender communities to encourage participation in surveillance and research activities.
Enhanced Surveillance Through Behavioral Studies
Beyond routine surveillance, the CDC has implemented specialized behavioral surveillance studies that provide more detailed information about HIV-related behaviors, experiences, and needs among transgender people.
National HIV Behavioral Surveillance (NHBS)
The NHBS transgender women component provides critical data on:
- HIV testing behaviors and outcomes
- Sexual and drug use behaviors
- Access to and utilization of prevention services
- Experiences of discrimination and stigma
- Social and structural factors affecting HIV risk
Medical Monitoring Project (MMP)
The MMP provides detailed information about the experiences of people with diagnosed HIV, including transgender people, covering:
- Engagement in care and treatment outcomes
- Barriers to care and unmet service needs
- Psychosocial factors affecting health outcomes
- Quality of life and social support
Transgender HIV Data on AIDSVu
AIDSVu recognizes both the importance of transgender data and the current limitations in data availability. The platform currently includes:
Current Data Availability
- Limited city-level data on transgender people with HIV, acknowledging that this represents an undercount
- Geographic analysis where data are available to identify areas of particular concern
- Integration with other HIV-related data to provide context for understanding transgender-specific patterns
Ongoing Commitments
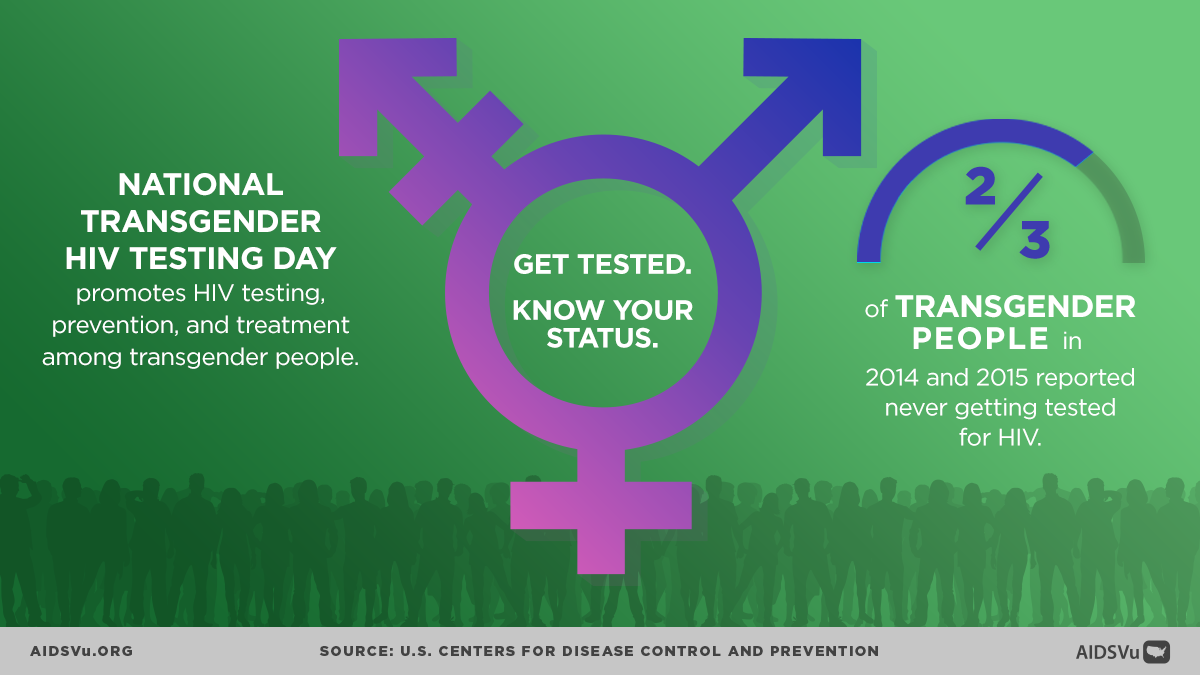
- Annual recognition of Transgender HIV Testing Day on April 18th through expert interviews and updated data visualizations
- Advocacy for improved data collection and surveillance practices
- Partnership with transgender advocacy organizations and researchers to promote better data
Future Directions
- Expanded data integration as more comprehensive surveillance data become available
- Community partnership in data interpretation and presentation to ensure cultural competency and accuracy
- Policy advocacy to support improved data collection practices at state and local levels
Moving Forward: A Public Health Imperative
Addressing HIV among transgender people requires recognizing that current disparities are not inevitable but rather the result of systematic exclusion and discrimination that can be addressed through targeted interventions and structural changes.
Priority Areas for Action
Comprehensive Anti-Discrimination Protections: Legal and policy changes to protect transgender people from discrimination in healthcare, employment, housing, and education.
Healthcare System Transformation: Training programs for healthcare providers, policy changes to ensure coverage of transgender health needs, and development of transgender-competent HIV care models.
Community-Centered Prevention Programs: HIV prevention programs designed by and for transgender communities, with particular attention to the needs of transgender women of color.
Data and Surveillance Improvements: Continued investment in surveillance system improvements and research studies that center transgender experiences and needs.
Structural Interventions: Programs that address poverty, housing instability, and other structural determinants of health that increase HIV vulnerability.
Intersectional Approaches: Recognition that transgender people exist at the intersection of multiple identities and face compounding forms of discrimination that must be addressed comprehensively.
The HIV epidemic among transgender people represents both a public health crisis and a civil rights issue. Effective response requires not only biomedical interventions but also fundamental changes to the social, economic, and political conditions that create vulnerability. Only through such comprehensive approaches can we hope to achieve HIV prevention and care outcomes for transgender people that reflect their inherent dignity and worth.
5 Ways to Use AIDSVu
View local statistics
National-, state-, and city-level profiles including transgender data at the city level.
Learn MoreShare infographics
Infographics presenting insights on HIV in the transgender population.
Learn MoreExpert blogs
Stay up to date with the latest Q&As from experts on transgender data and more.
Learn More