The Current Landscape
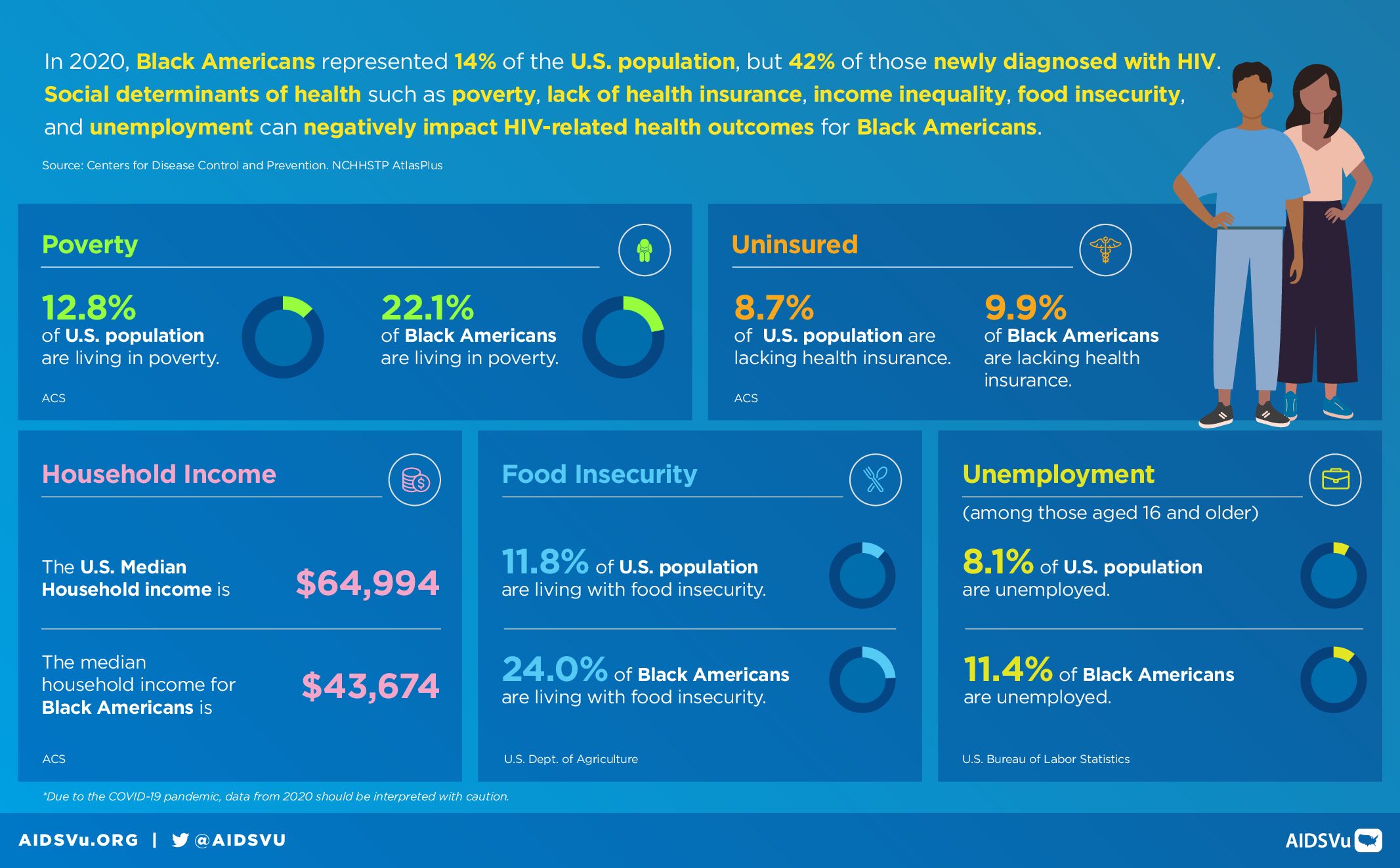
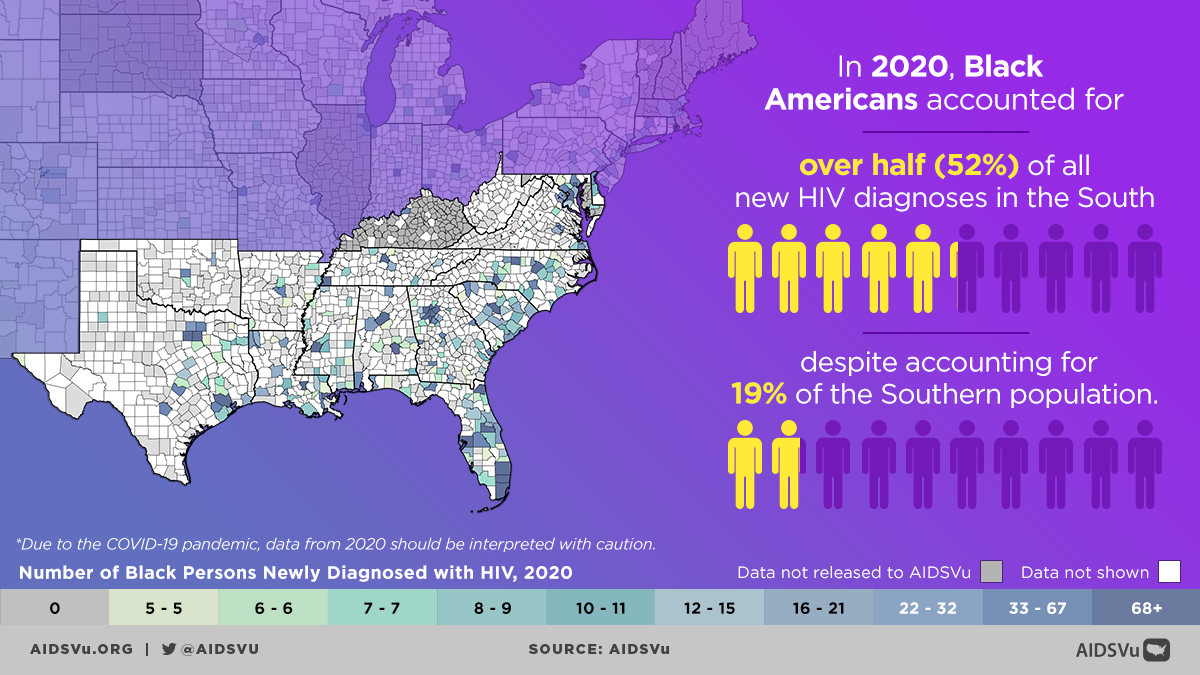
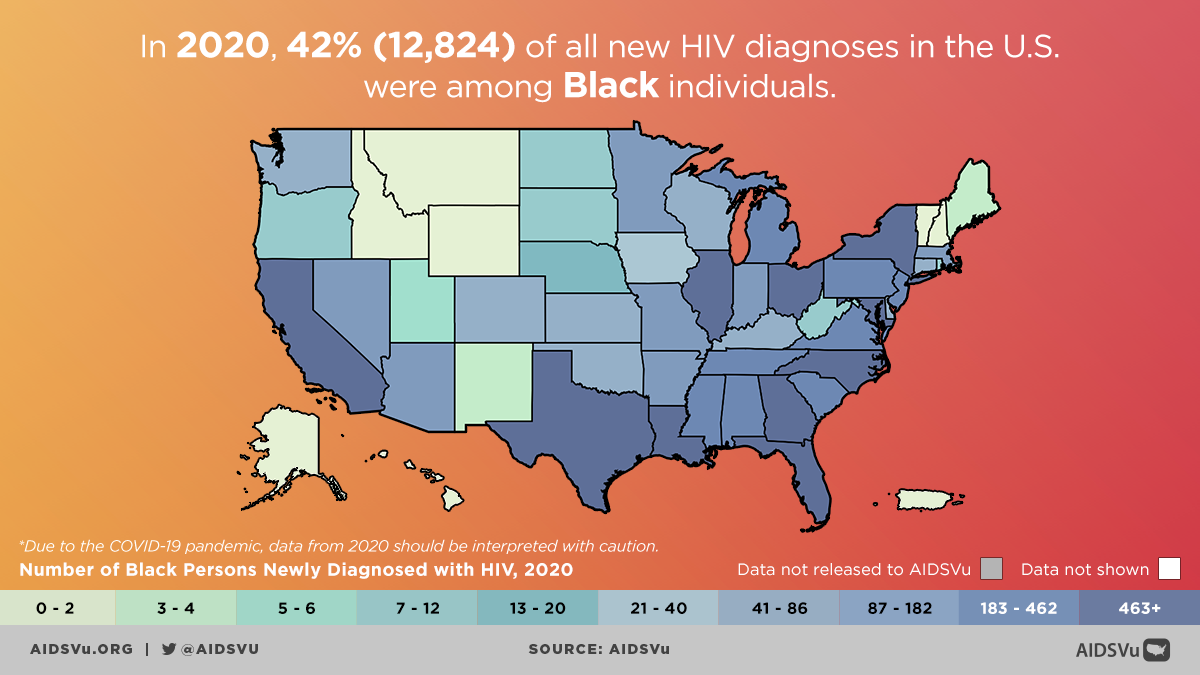
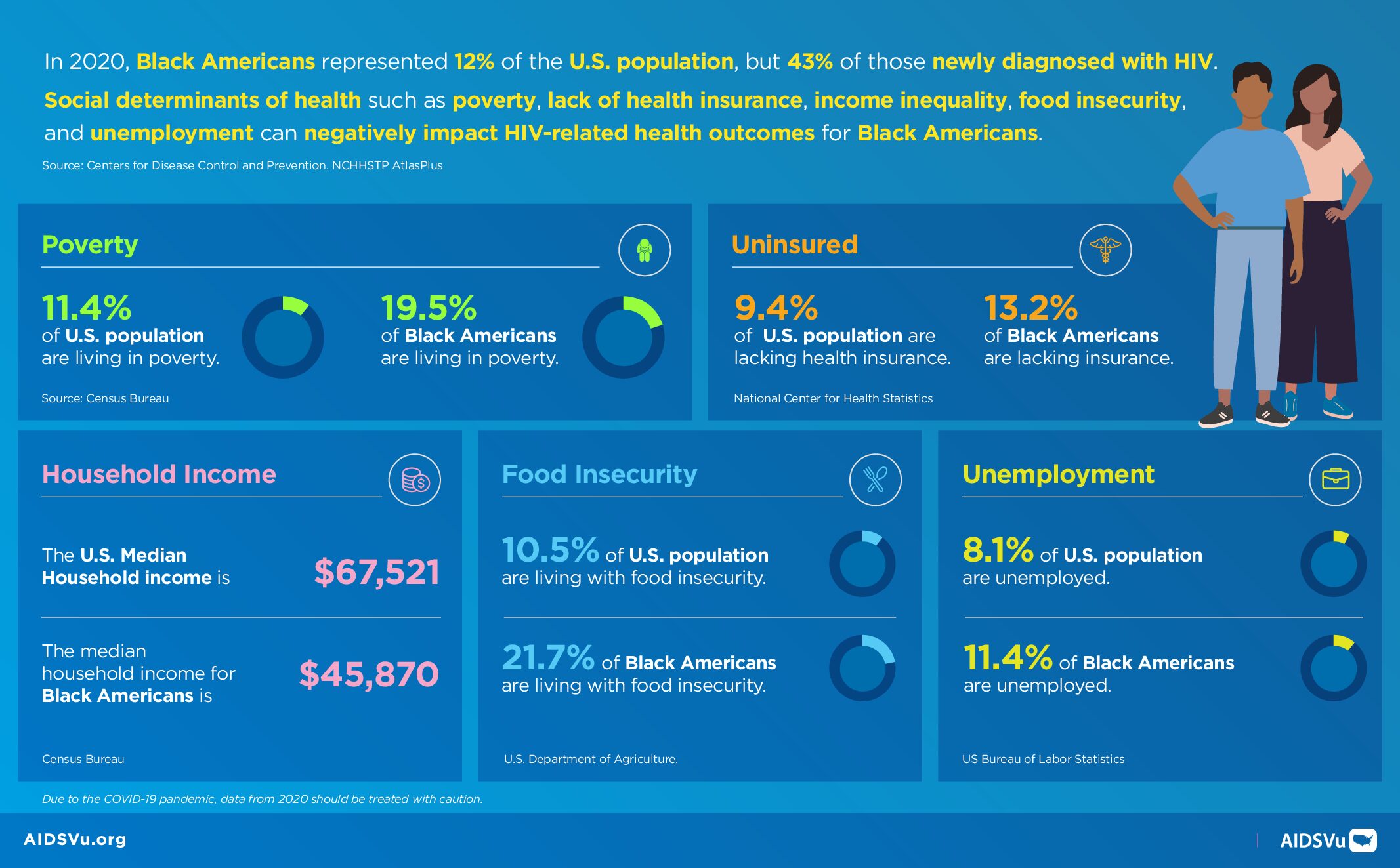
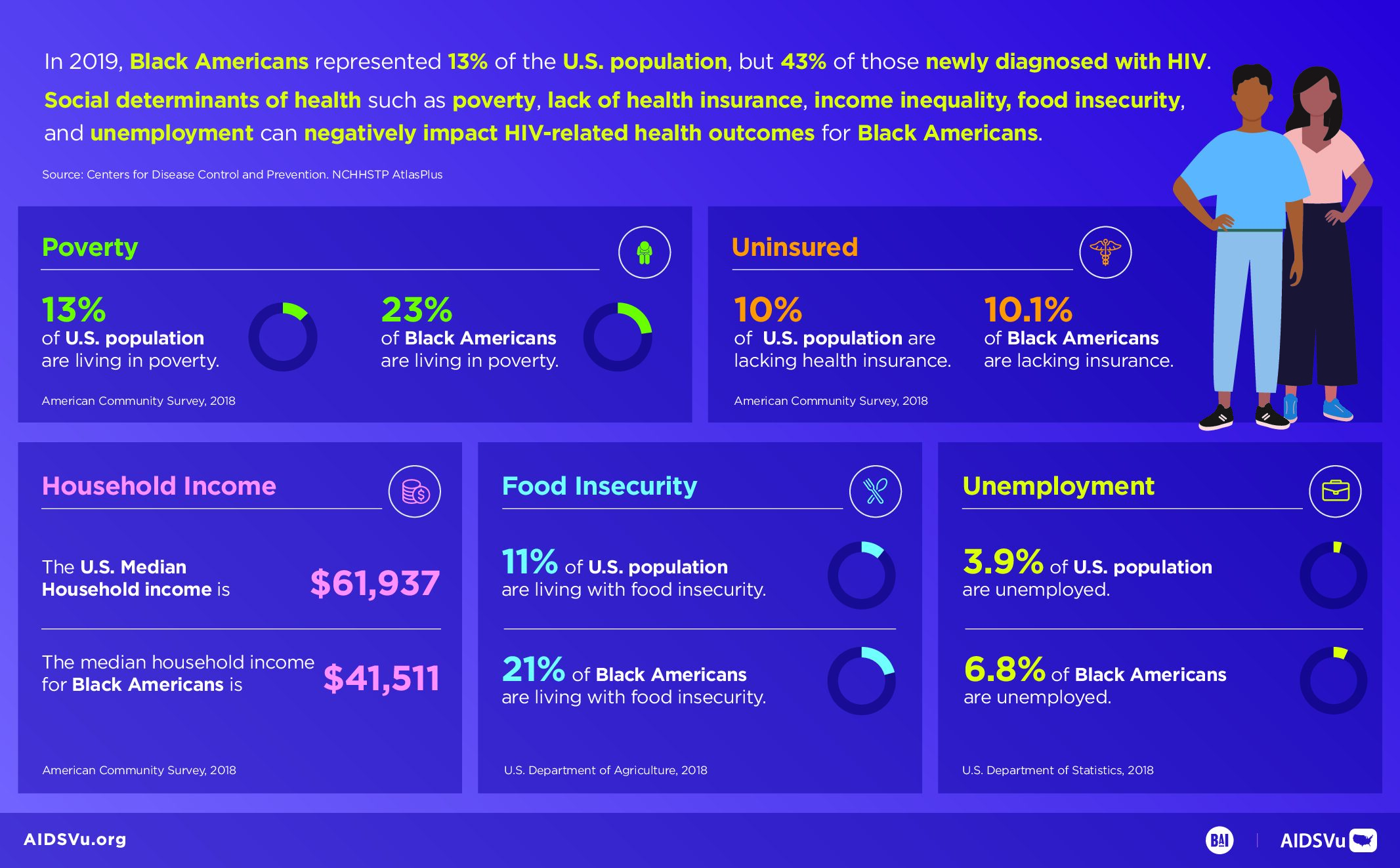
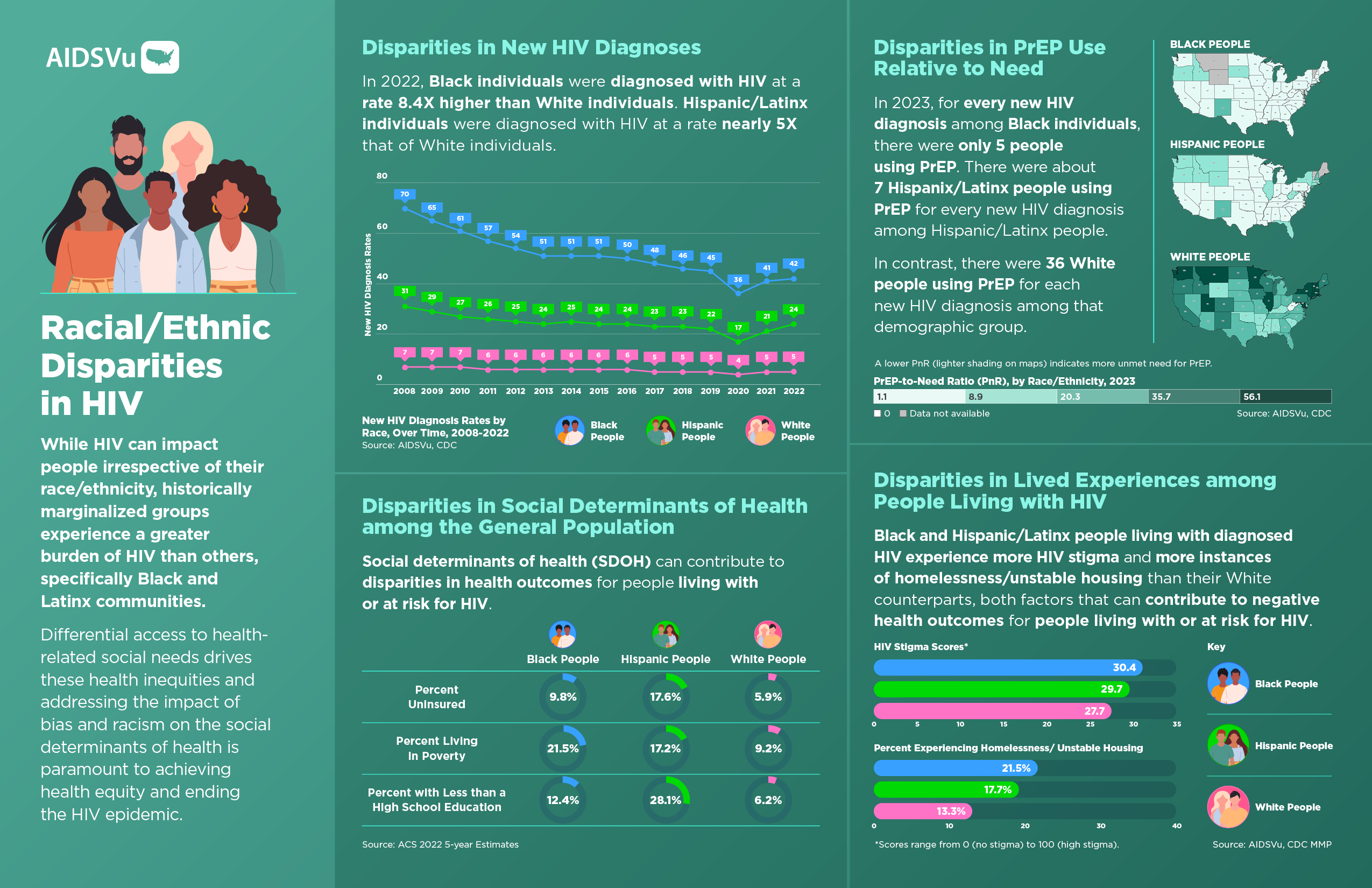
The Black community in the United States continues to face profound and persistent disparities in HIV prevention, diagnosis, treatment, and care. These disparities are not the result of individual behaviors but stem from complex, interconnected structural and societal barriers that have been decades in the making. Historical and ongoing systemic inequities in healthcare access, housing stability, economic opportunity, and education create conditions that increase HIV vulnerability while limiting access to prevention and care services.
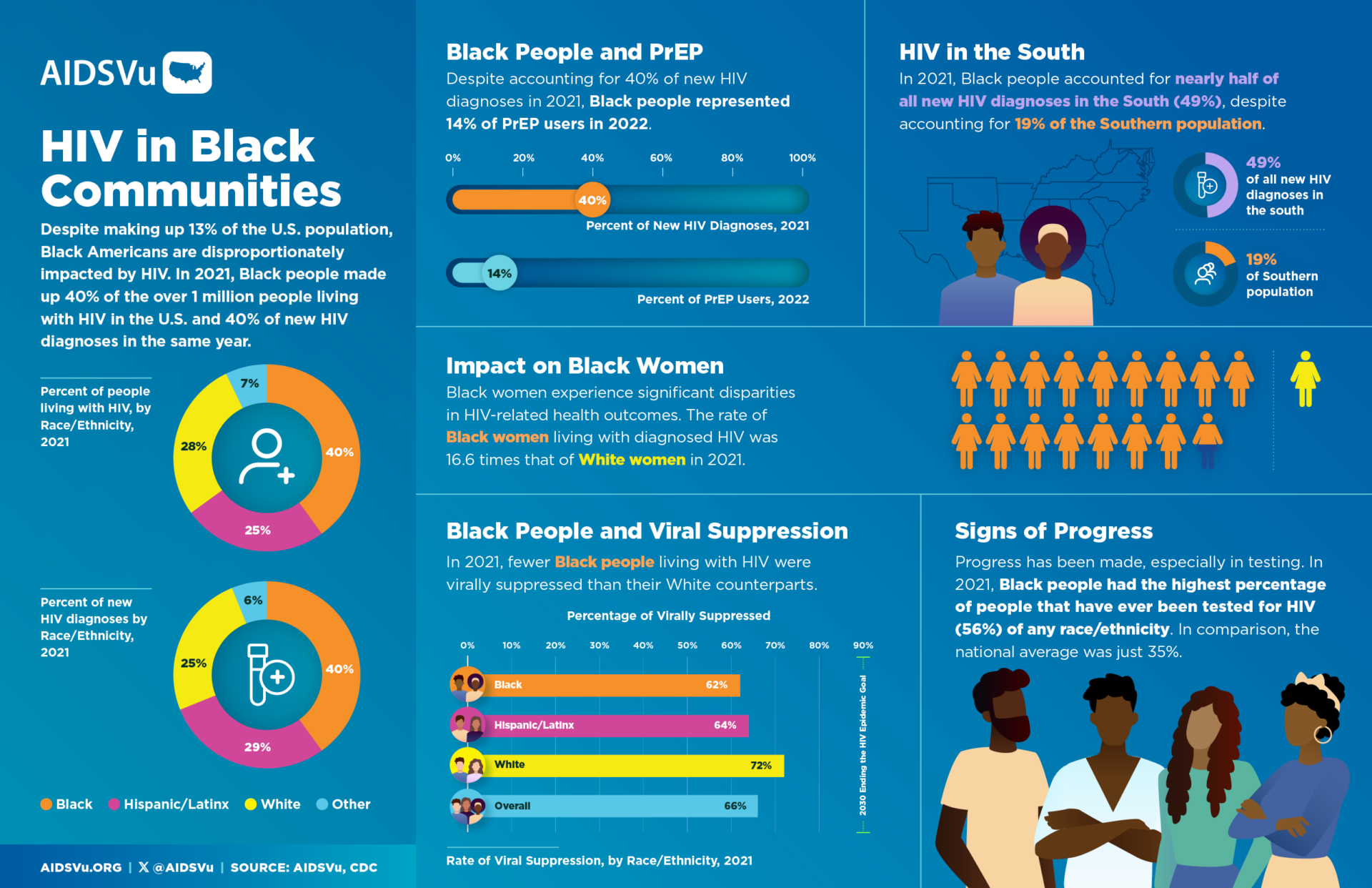
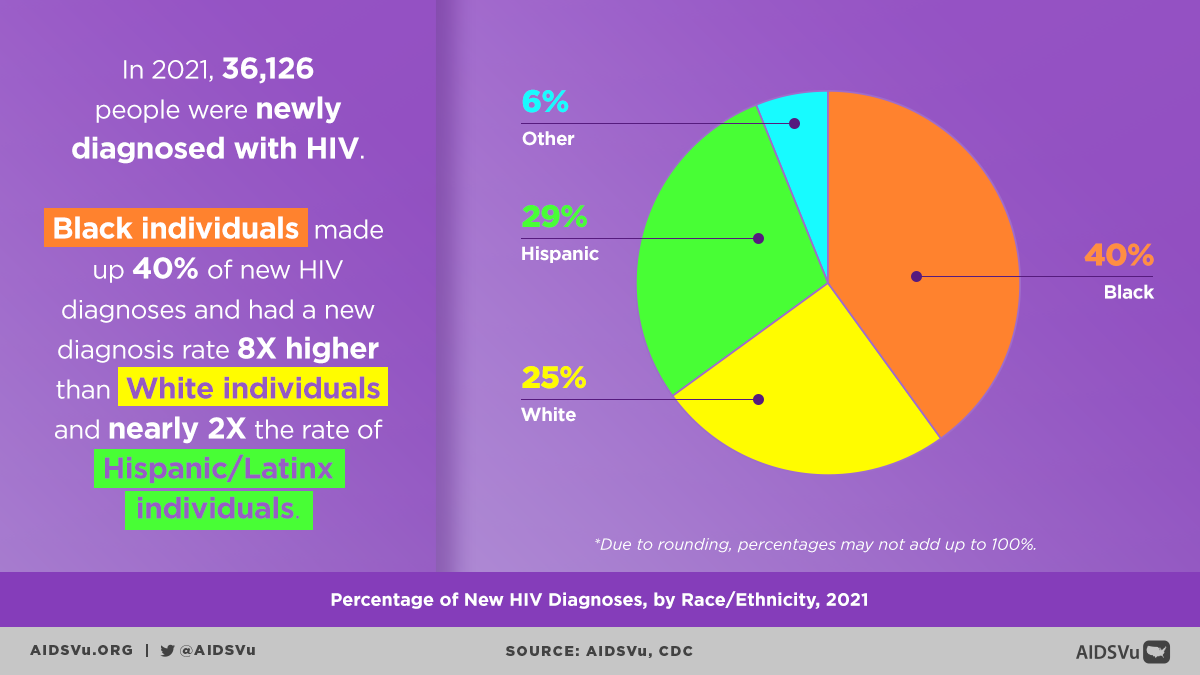
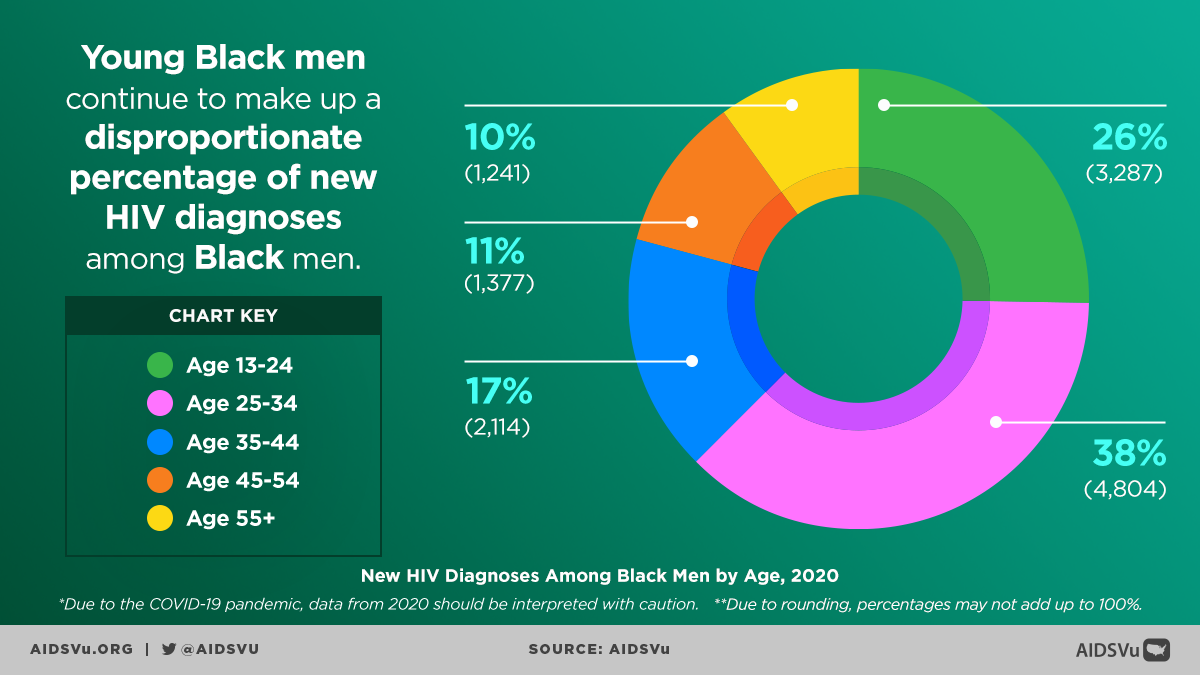
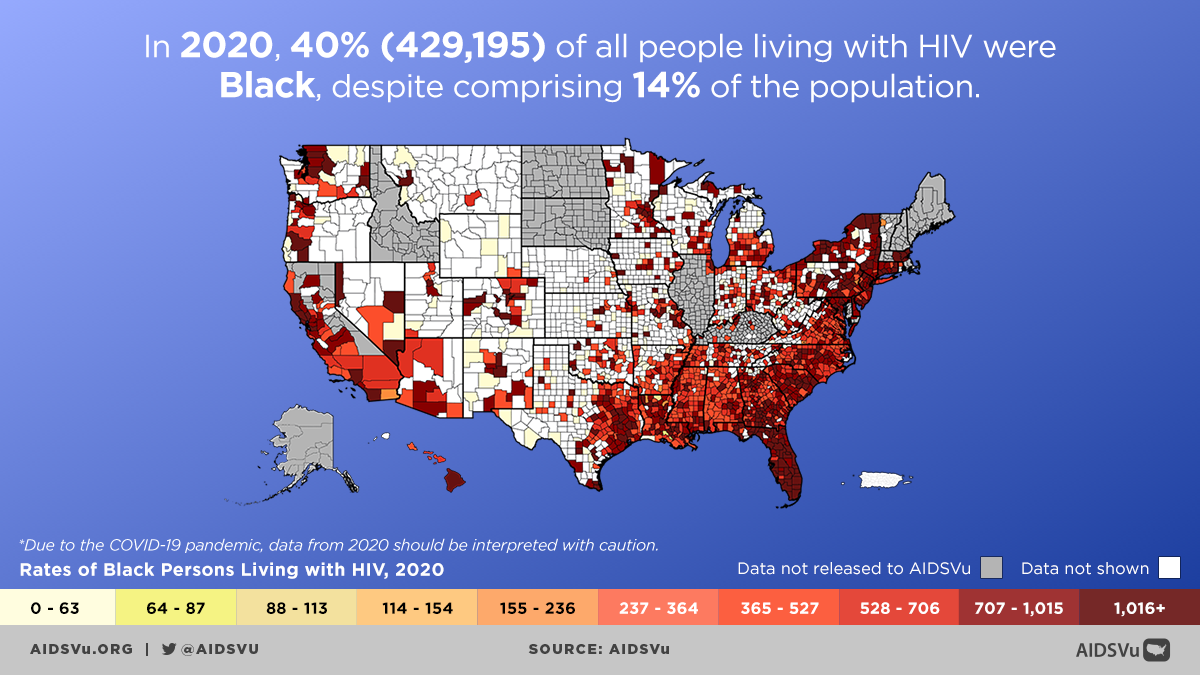
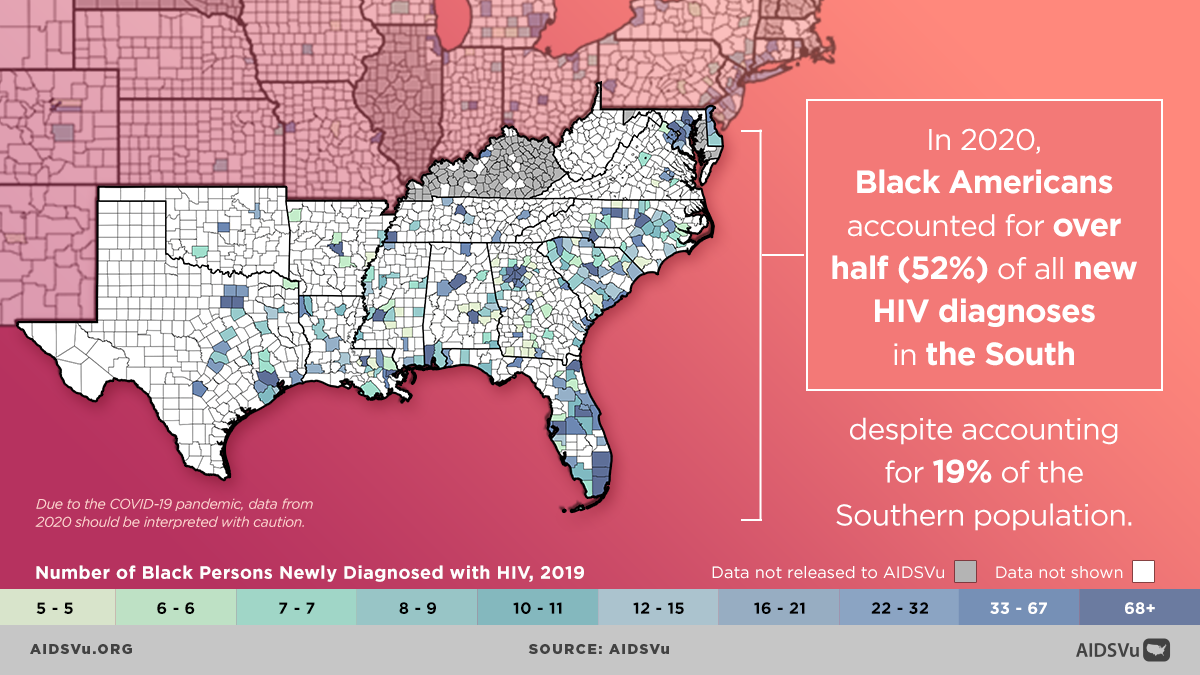
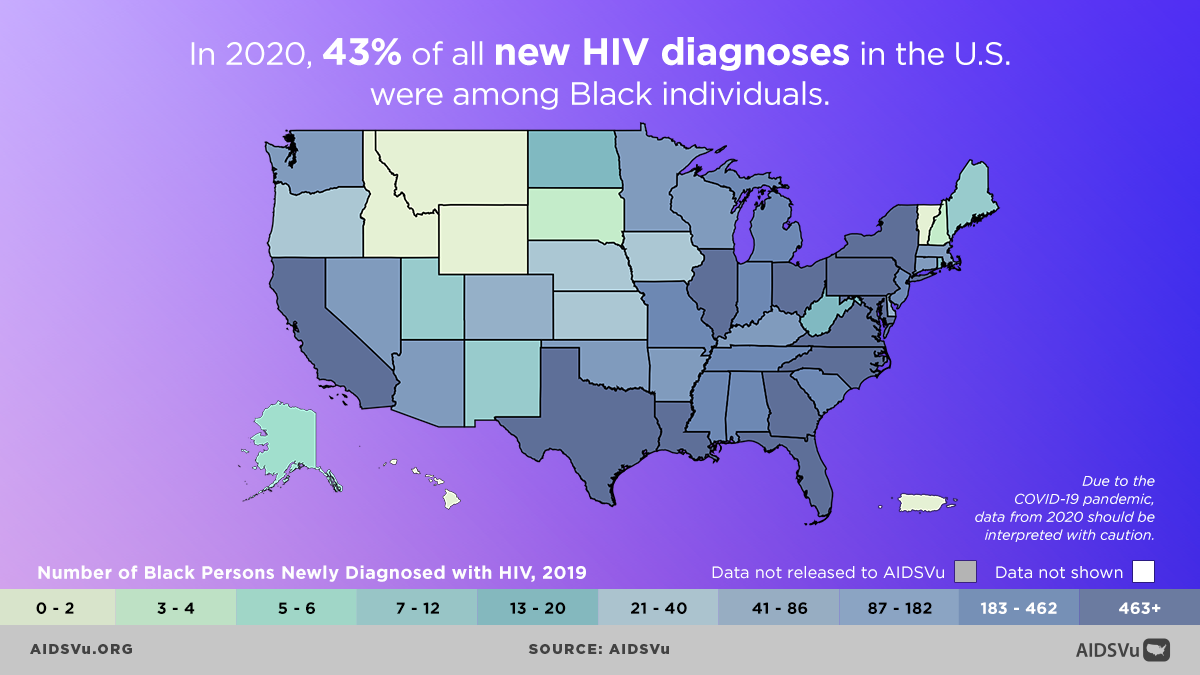
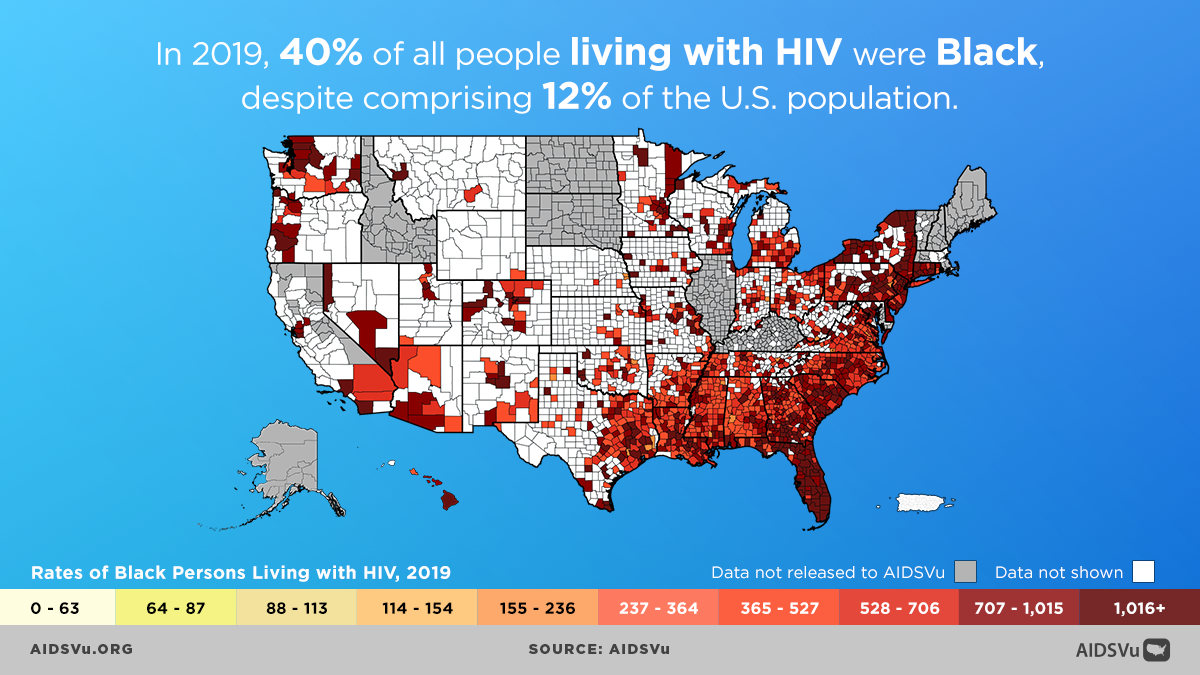
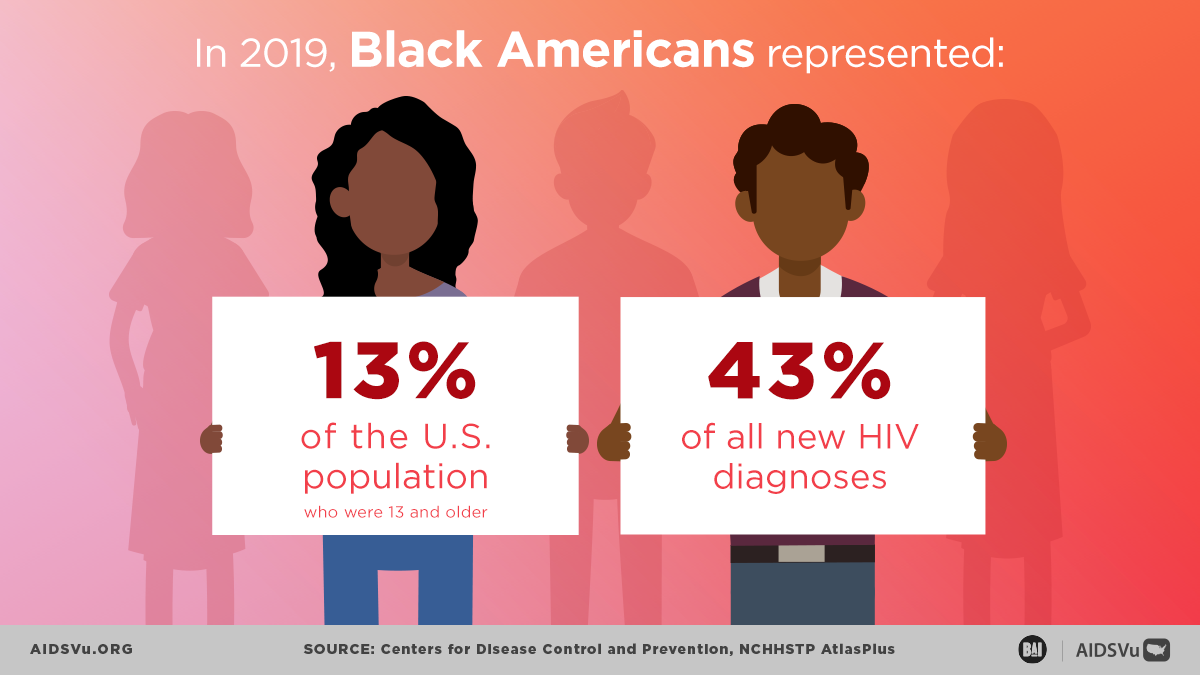
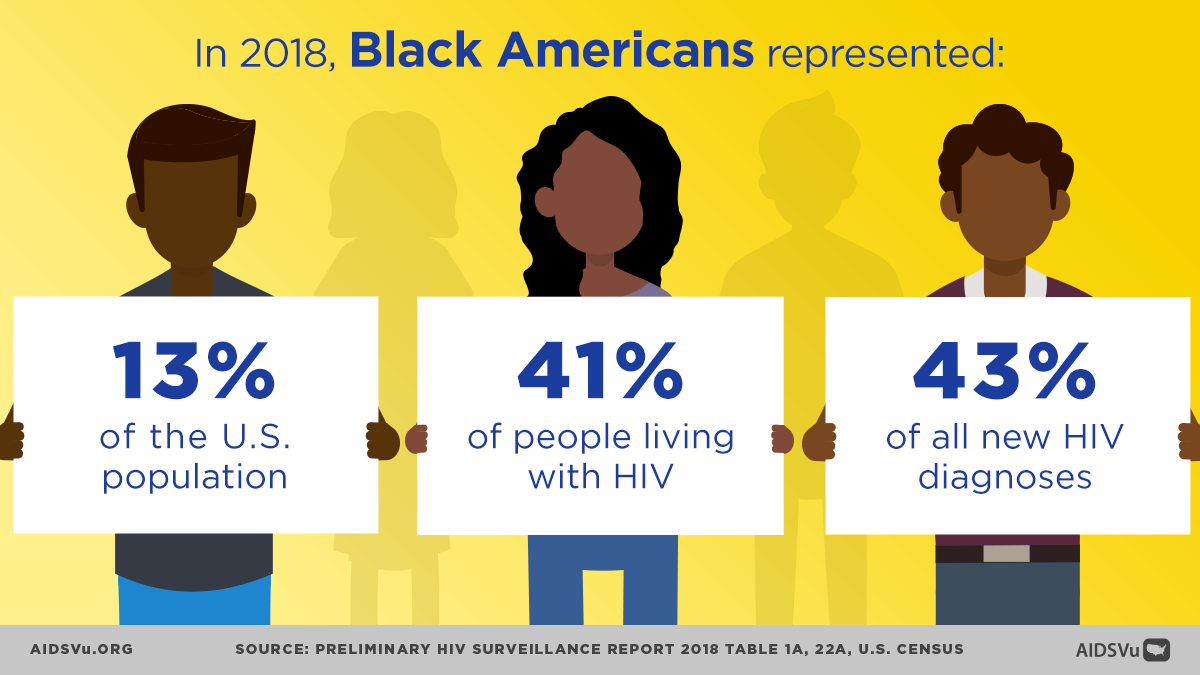
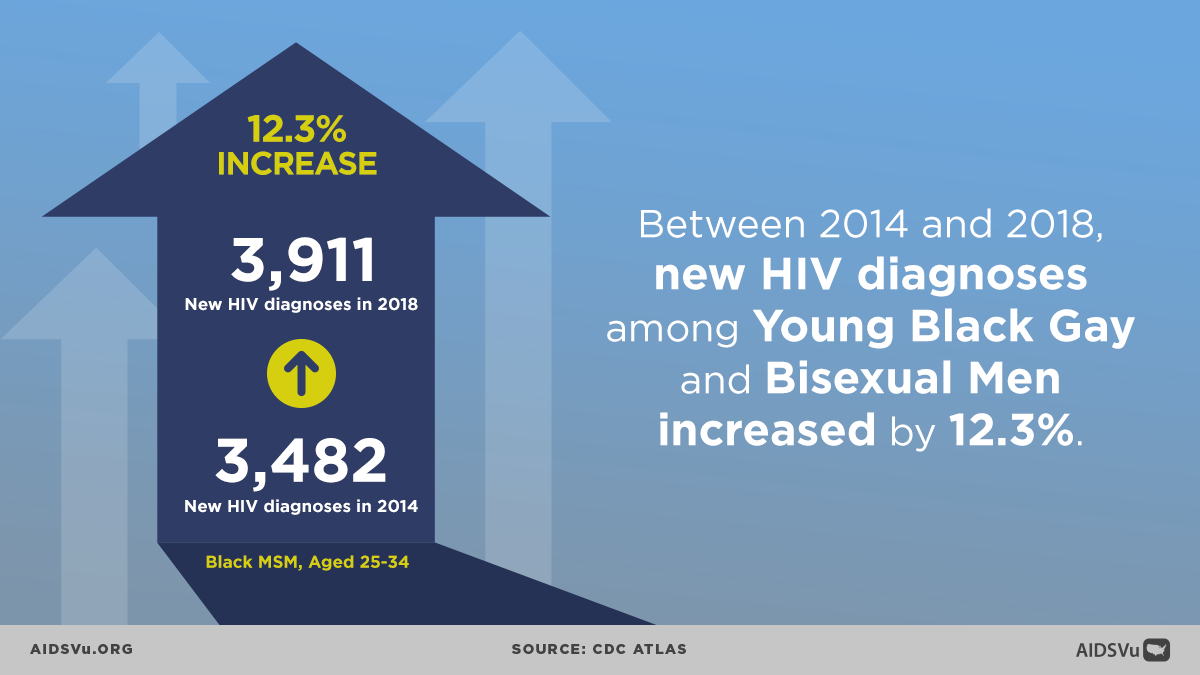
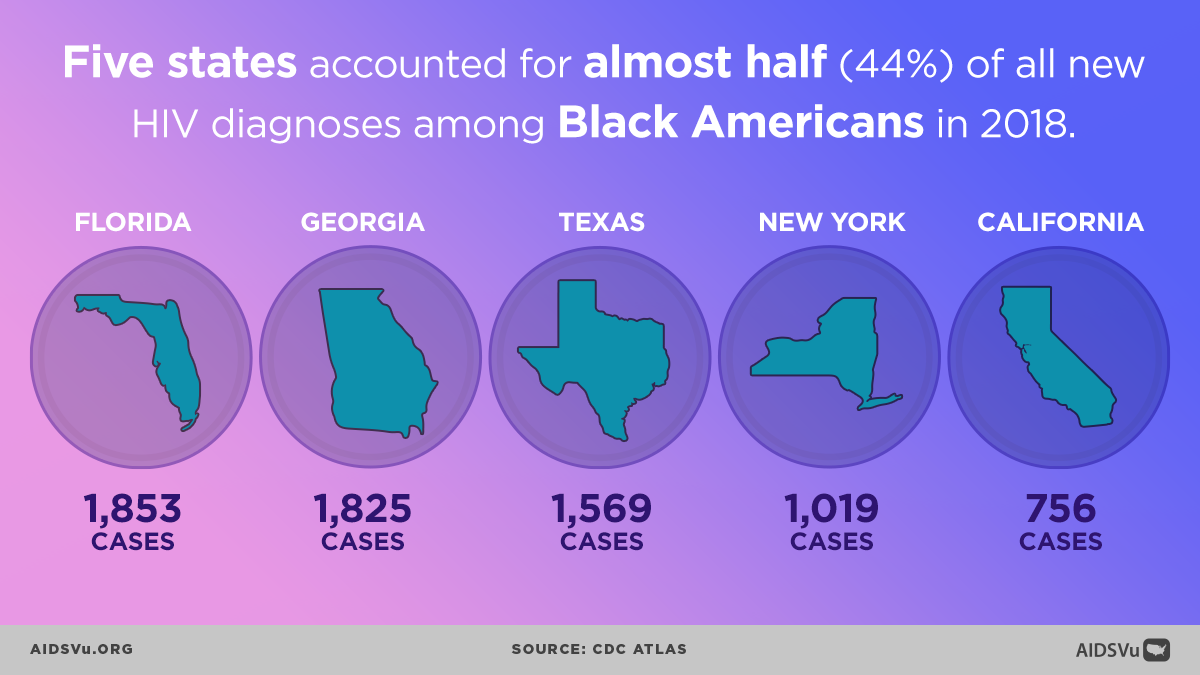
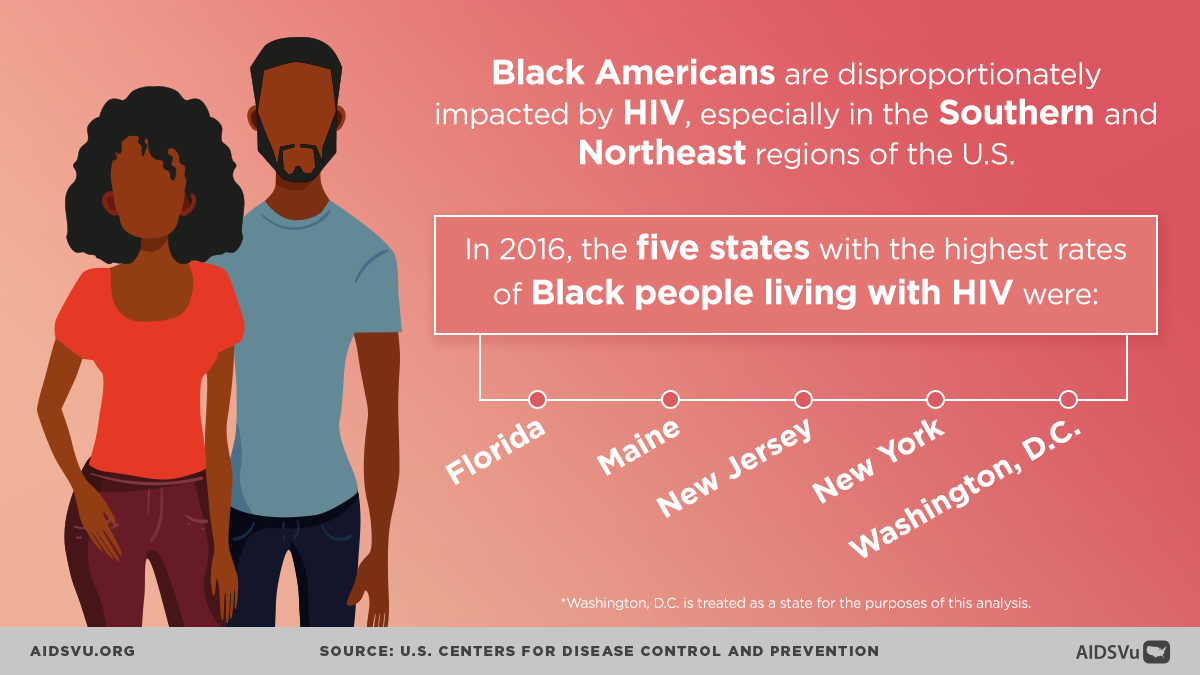
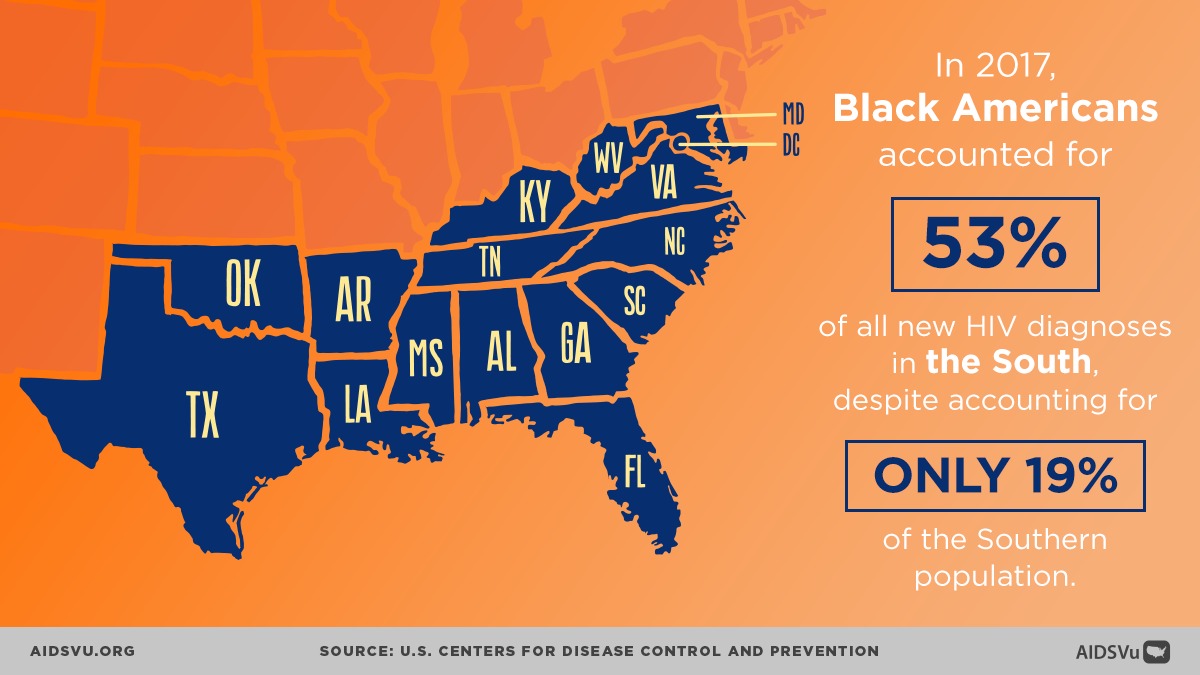
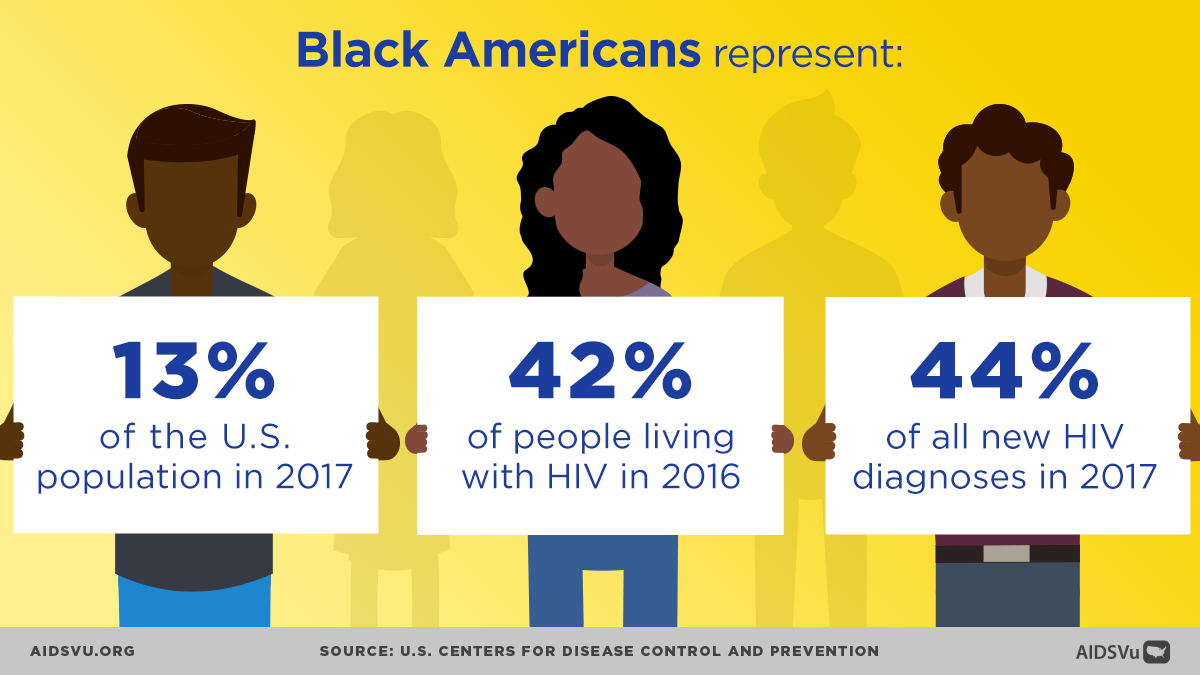
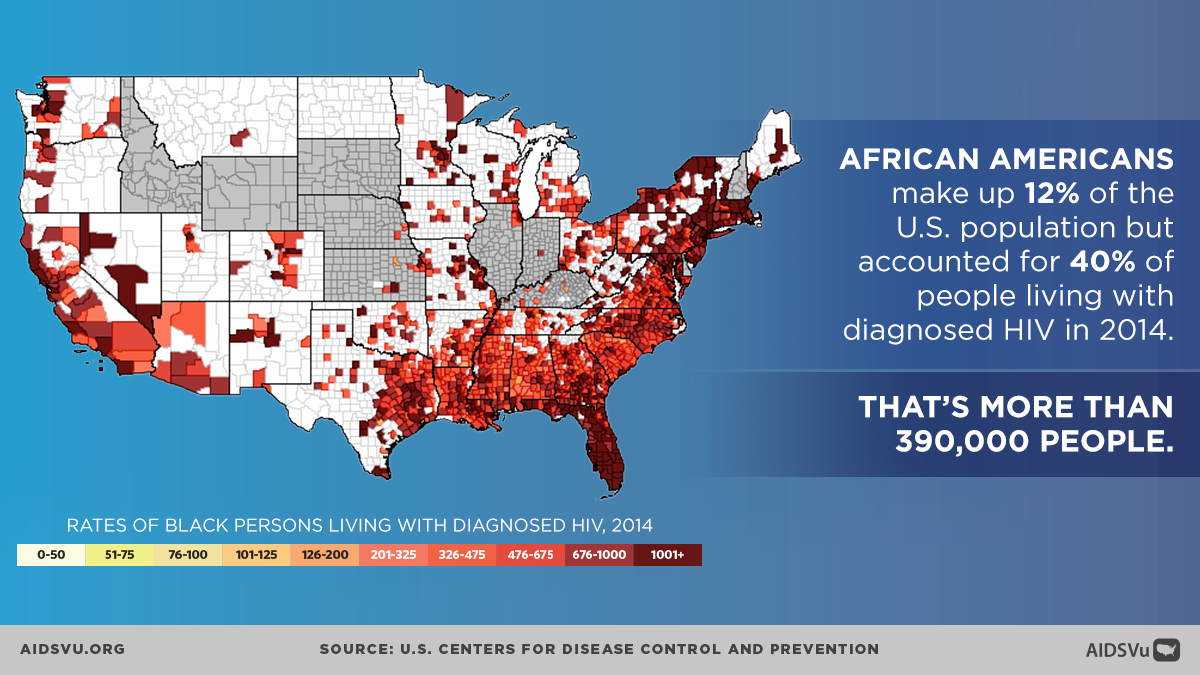
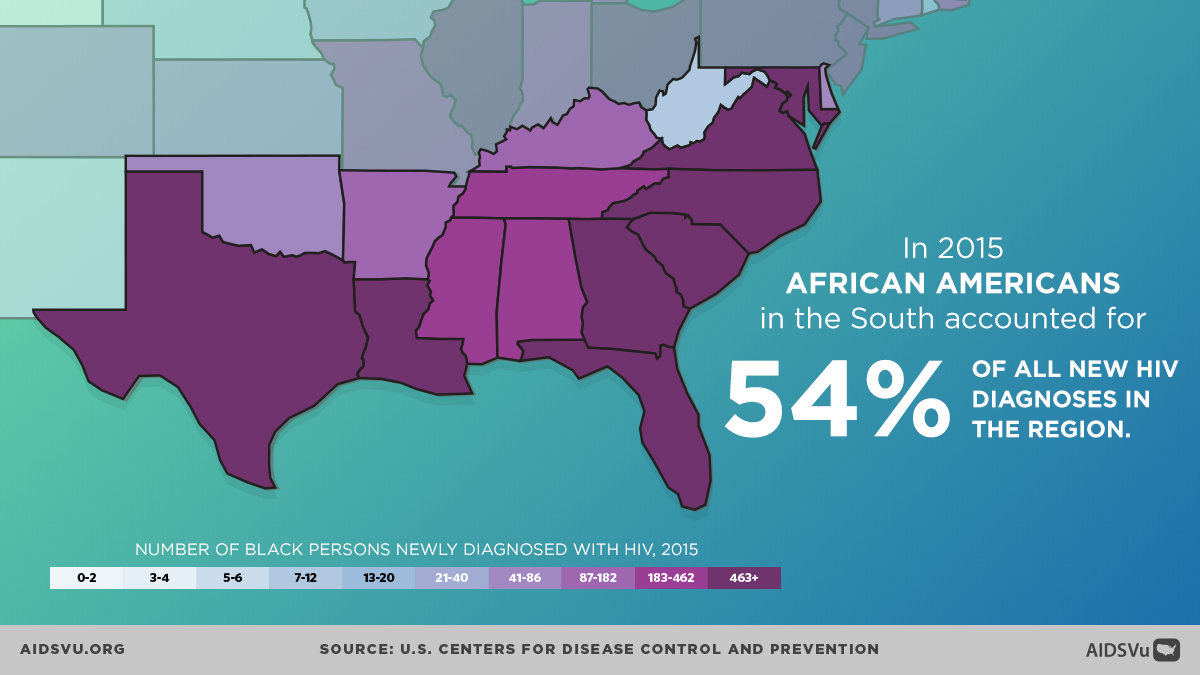
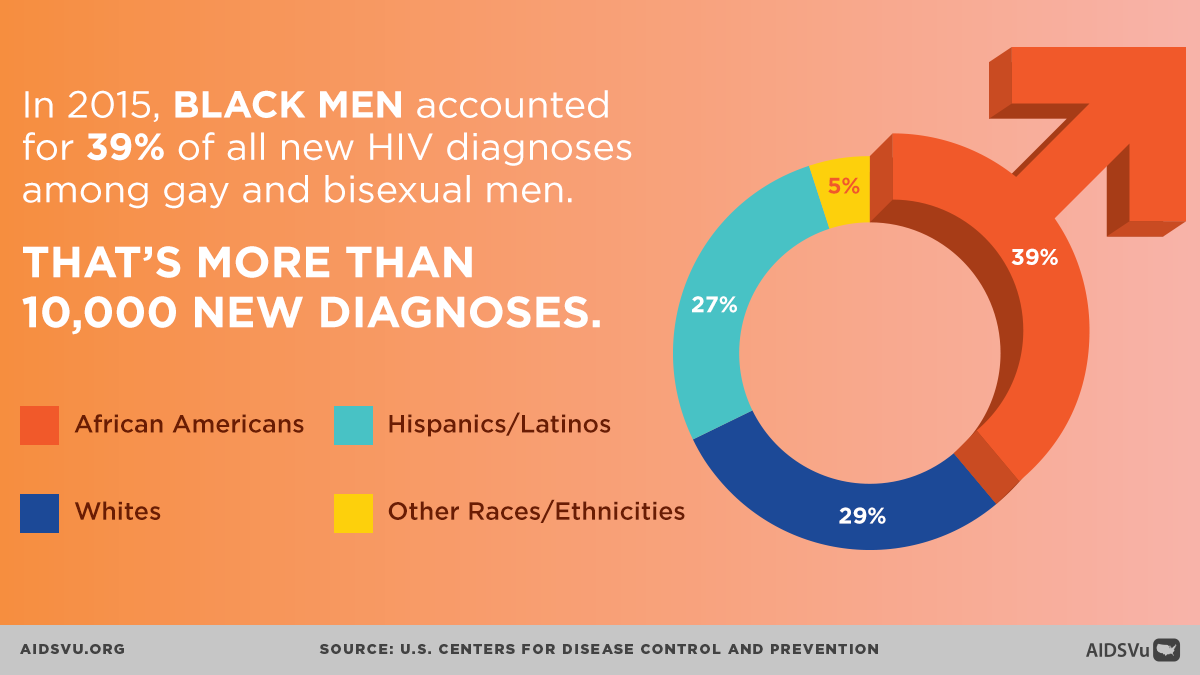
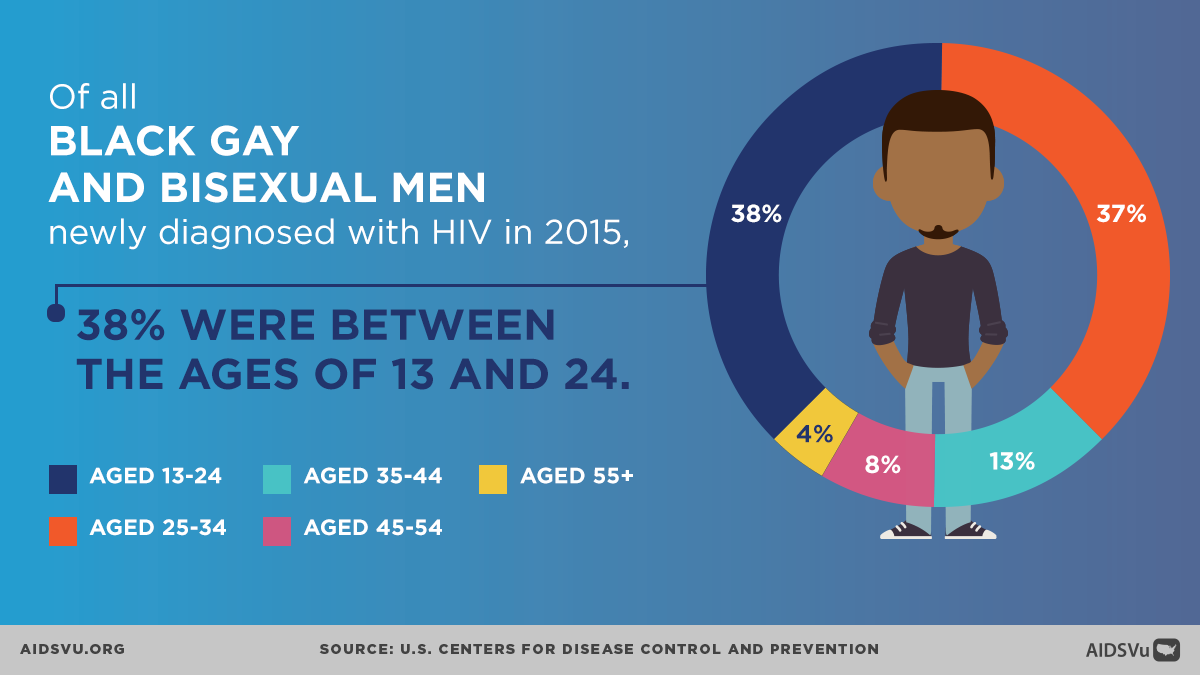
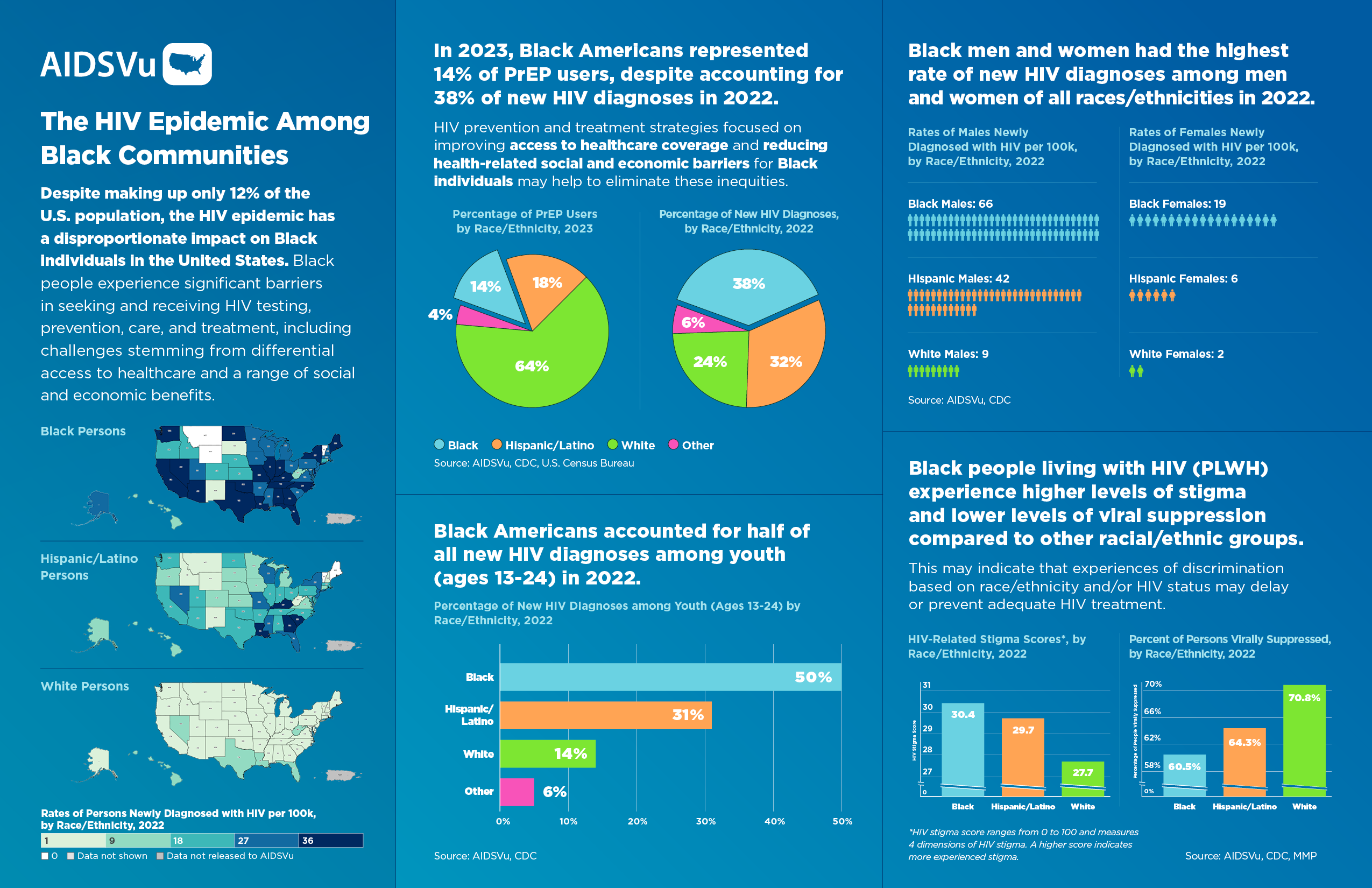
The numbers tell a stark story: In 2023, Black people represented 38% of new HIV diagnoses in the United States, despite comprising only 12% of the total population. Black people accounted for 14,754 of the 39,201 HIV diagnoses among persons aged 13 years and older, with a diagnosis rate of 41.9 per 100,000—about eight times higher than white Americans. The disparity is equally pronounced in HIV prevalence—39% of all people living with HIV in the U.S. (438,749 of 1,132,739 people) were Black in 2023, highlighting the cumulative impact of decades of unequal HIV burden.
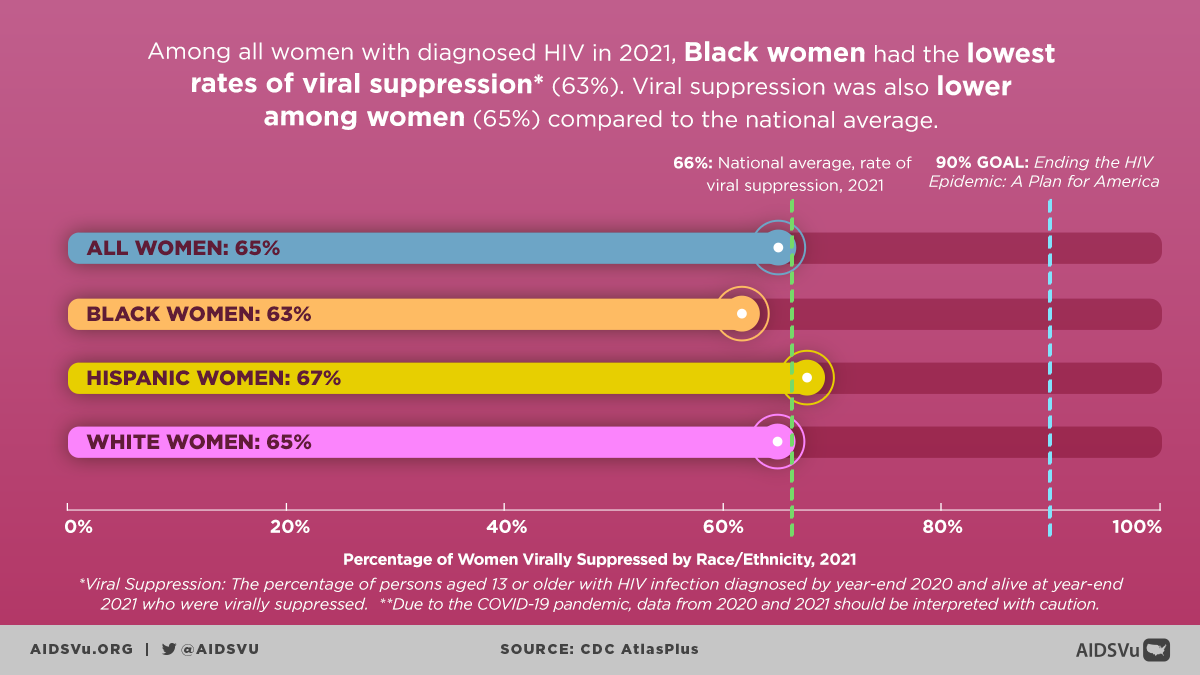
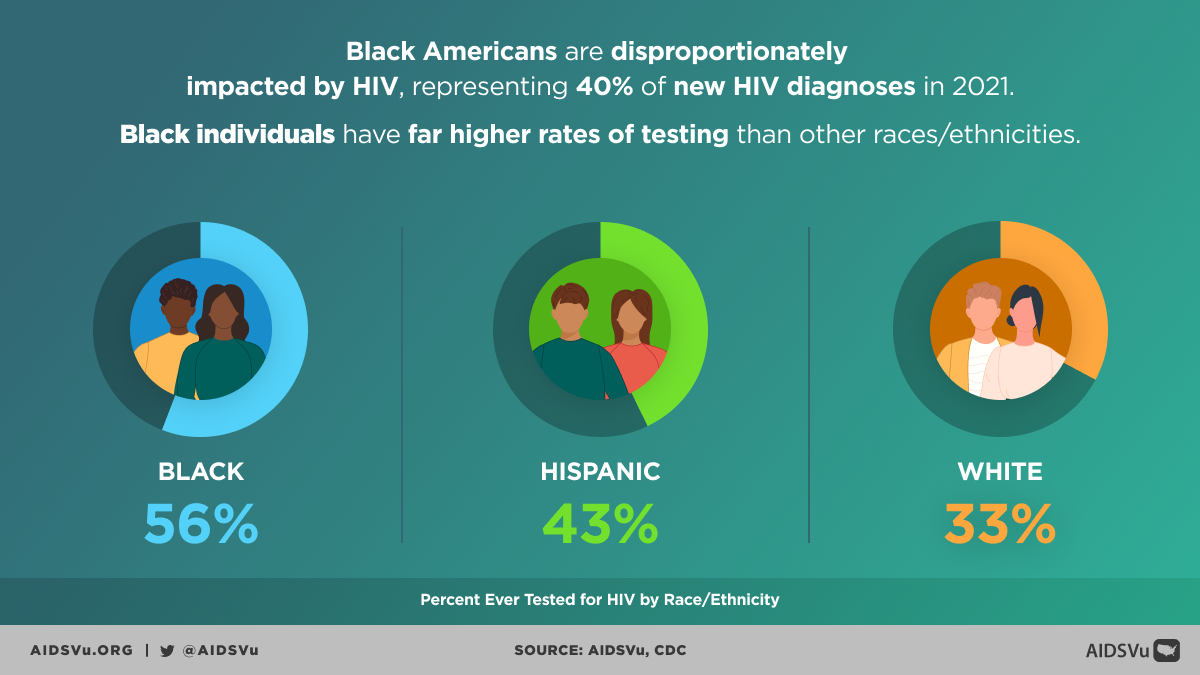
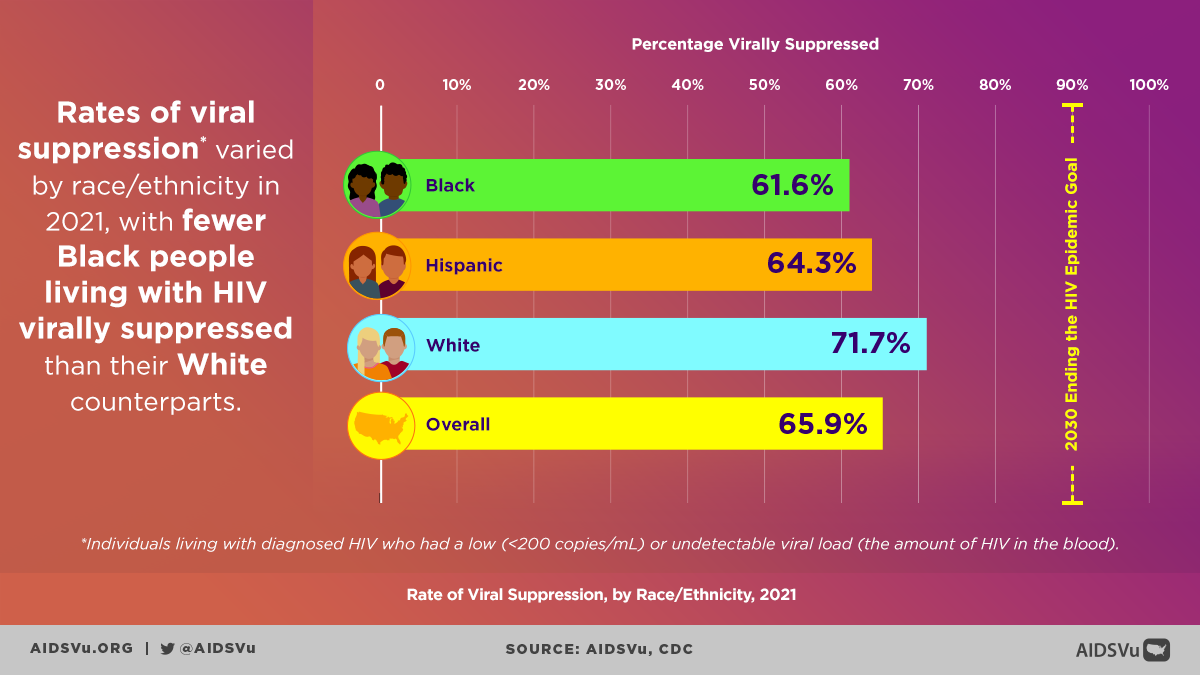
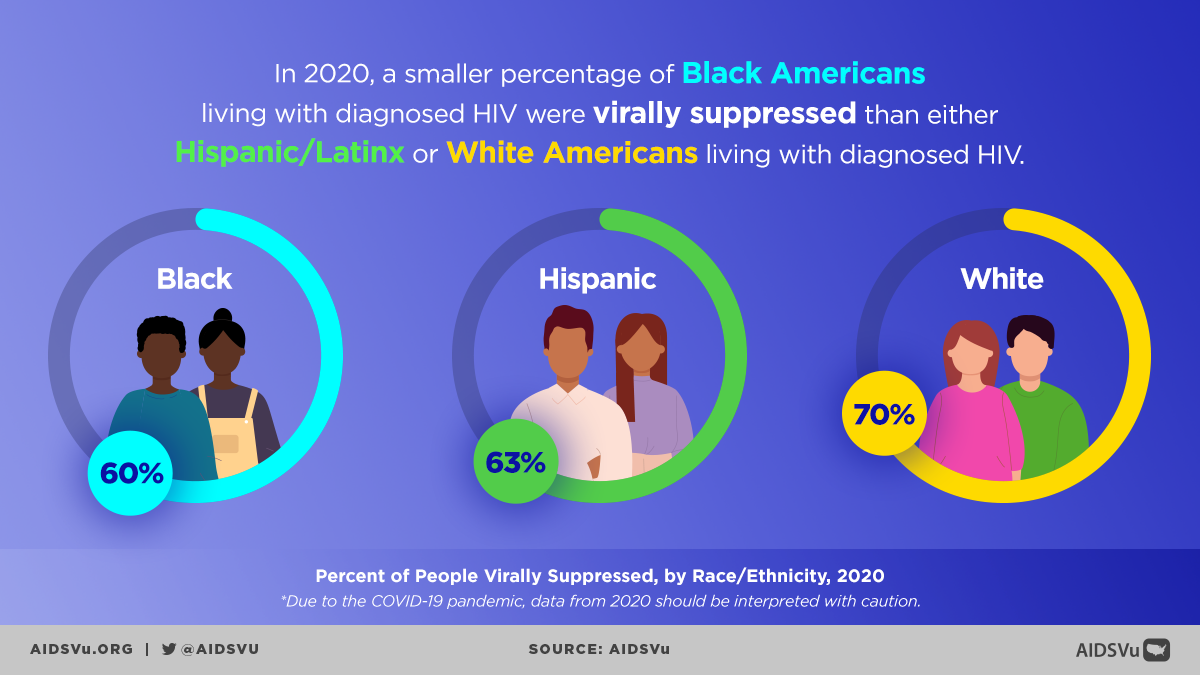
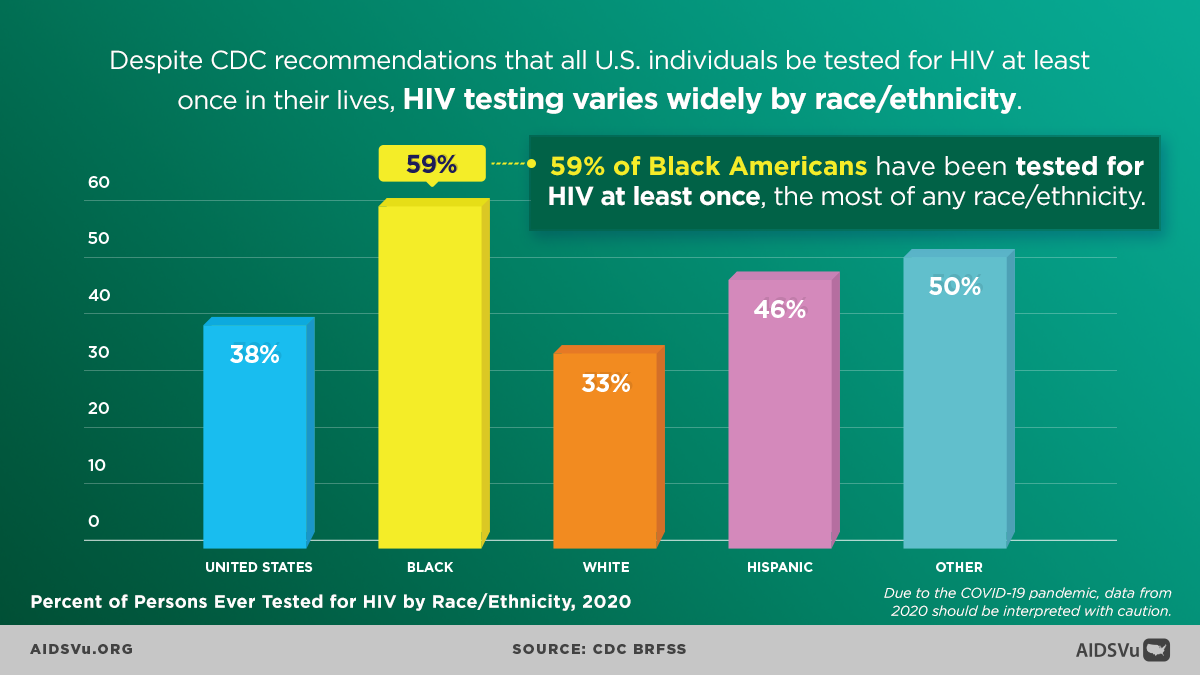
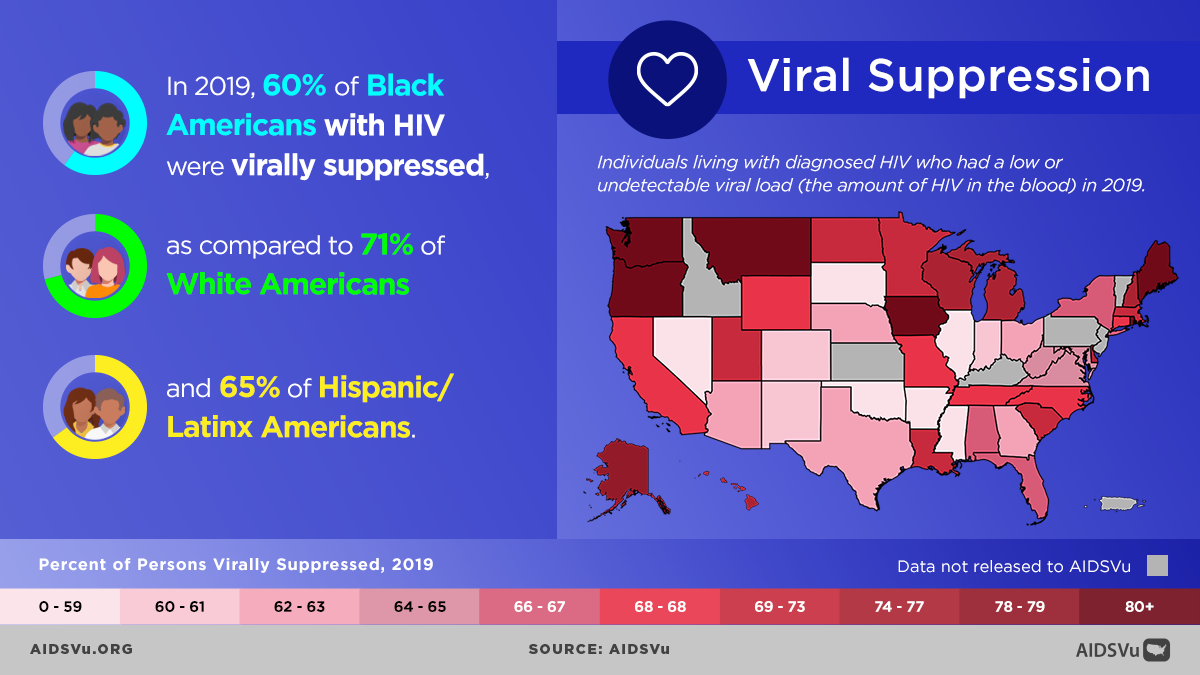
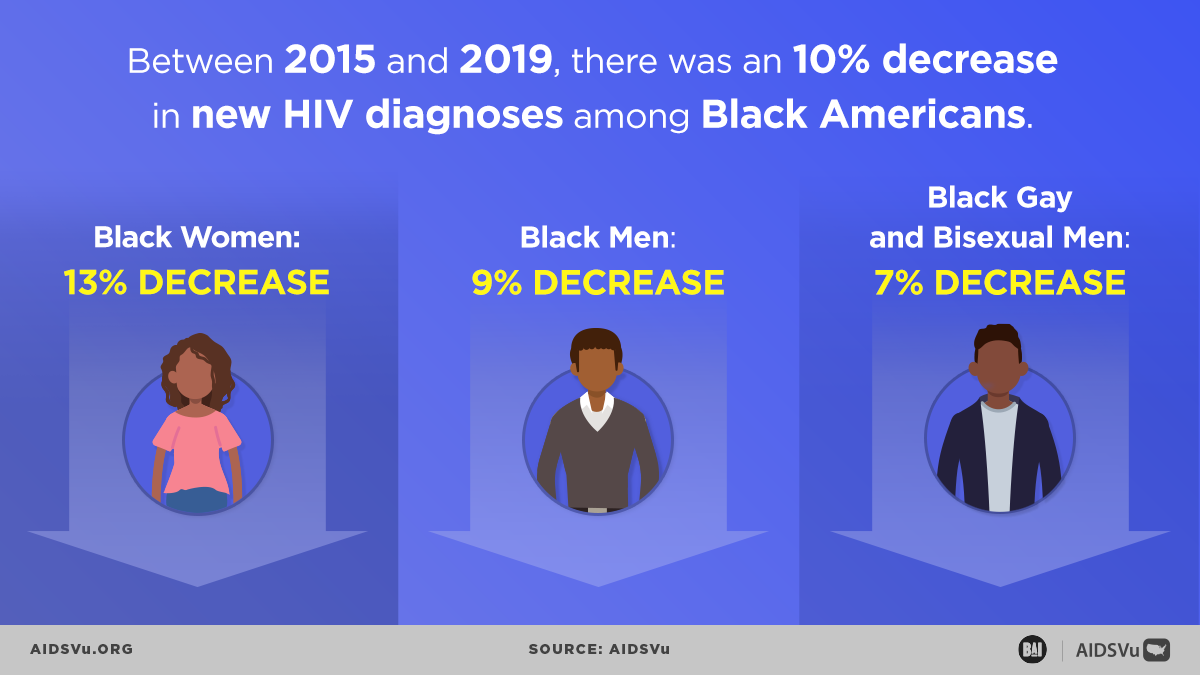
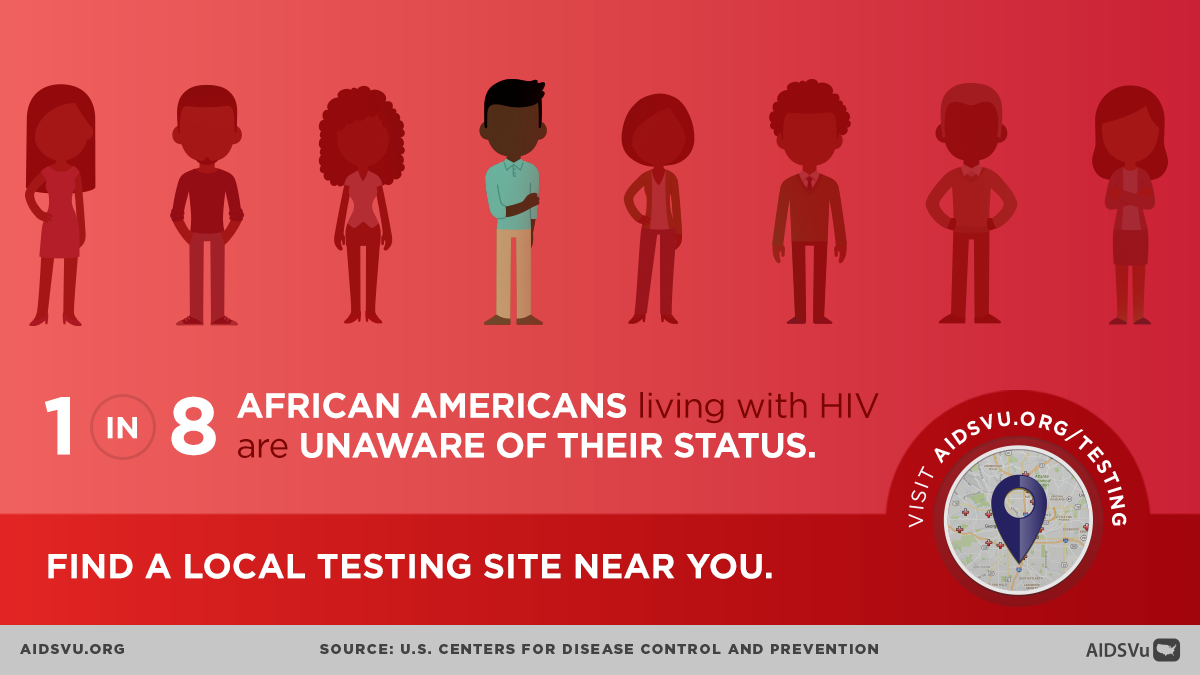
These structural challenges create cascading effects throughout the HIV care continuum. At the end of 2022, 88% of Black people with HIV were diagnosed, 64% were linked to care, and 53% were virally suppressed, compared to 89% of White people with HIV who were diagnosed, 70% who were linked to care, and 63% who were virally suppressed. However, there are encouraging signs of progress, particularly in HIV testing awareness and uptake. In 2022, over half (57%) of Black adults reported ever having been tested for HIV, a greater share than among Latino or White adults (44% and 32%, respectively). This demonstrates both increased health awareness and the critical importance of community-based testing initiatives.
Black Women and HIV: A Crisis Within a Crisis
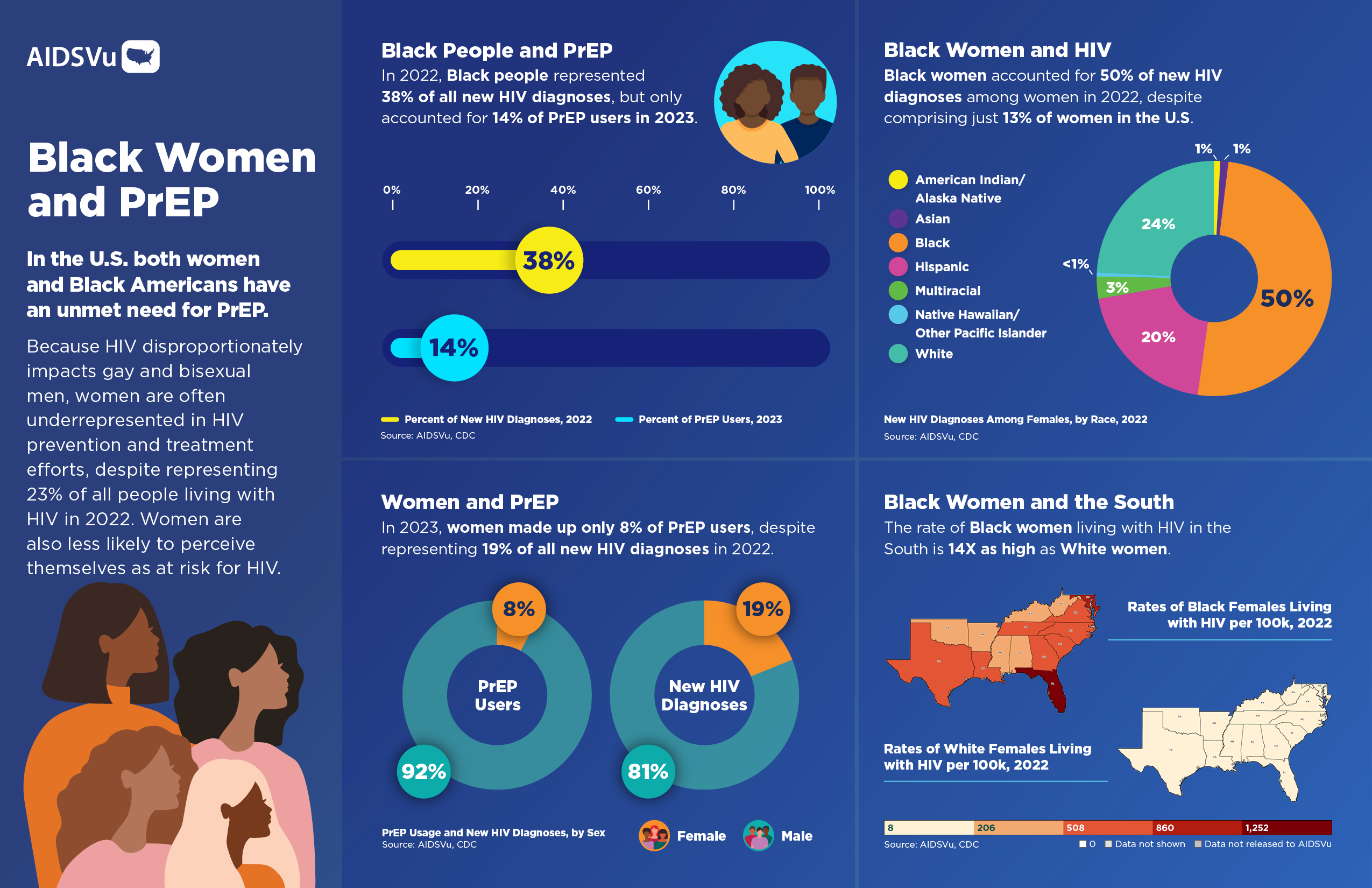
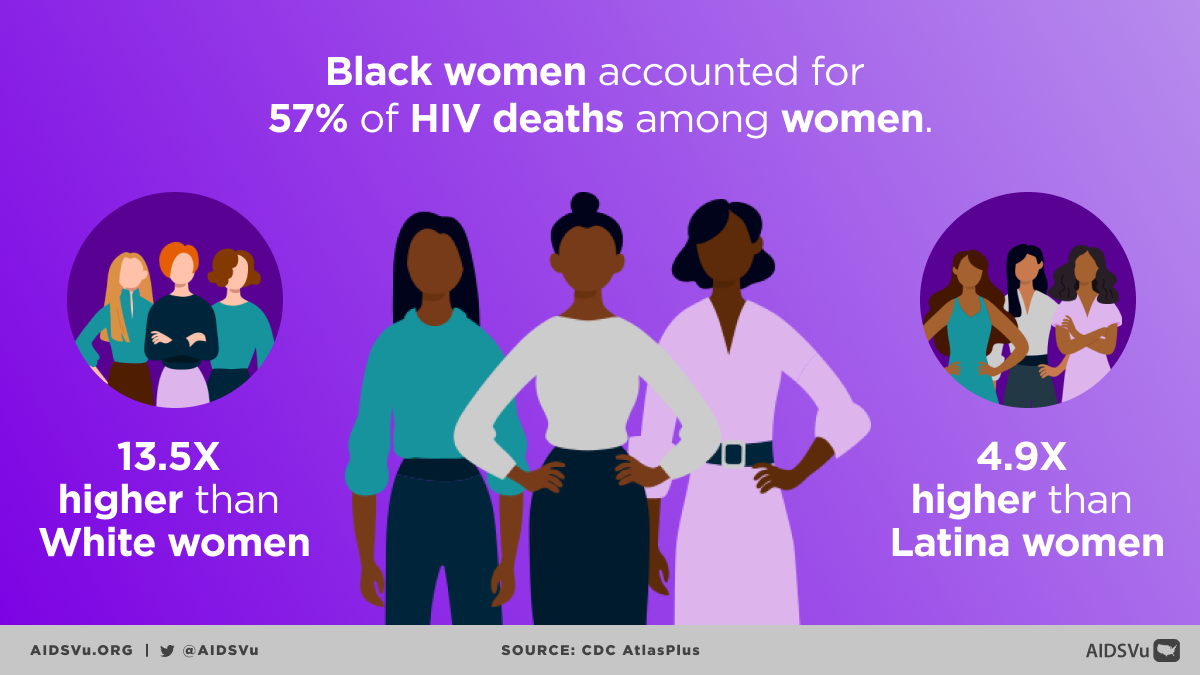
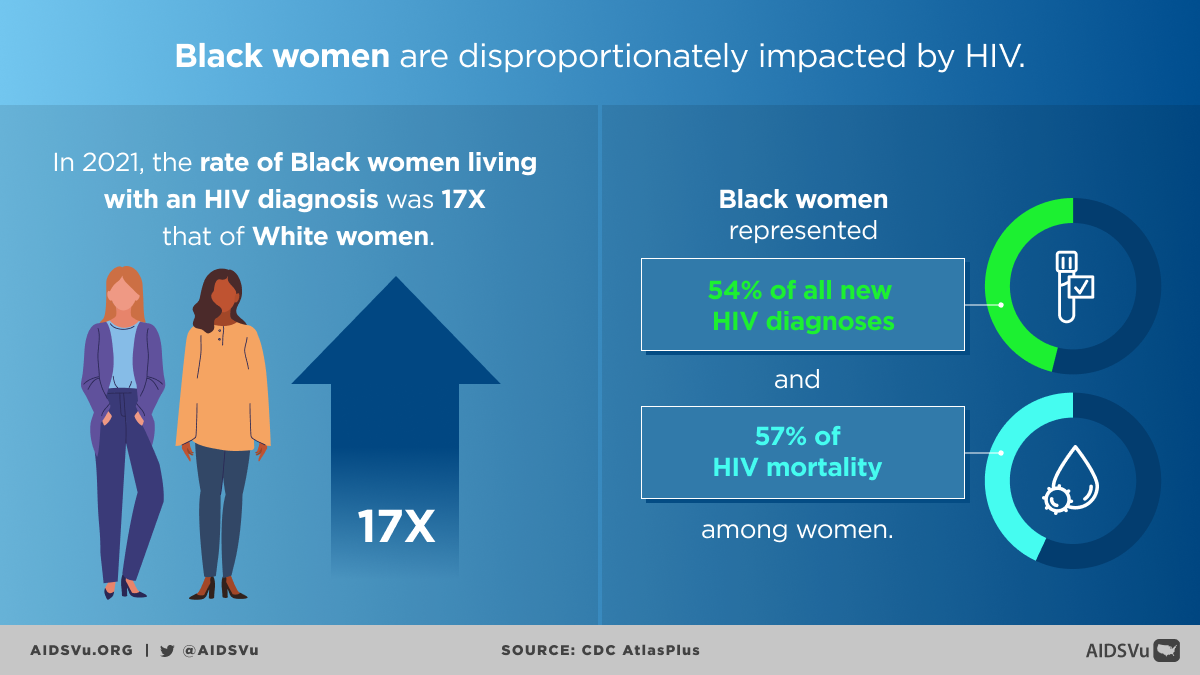
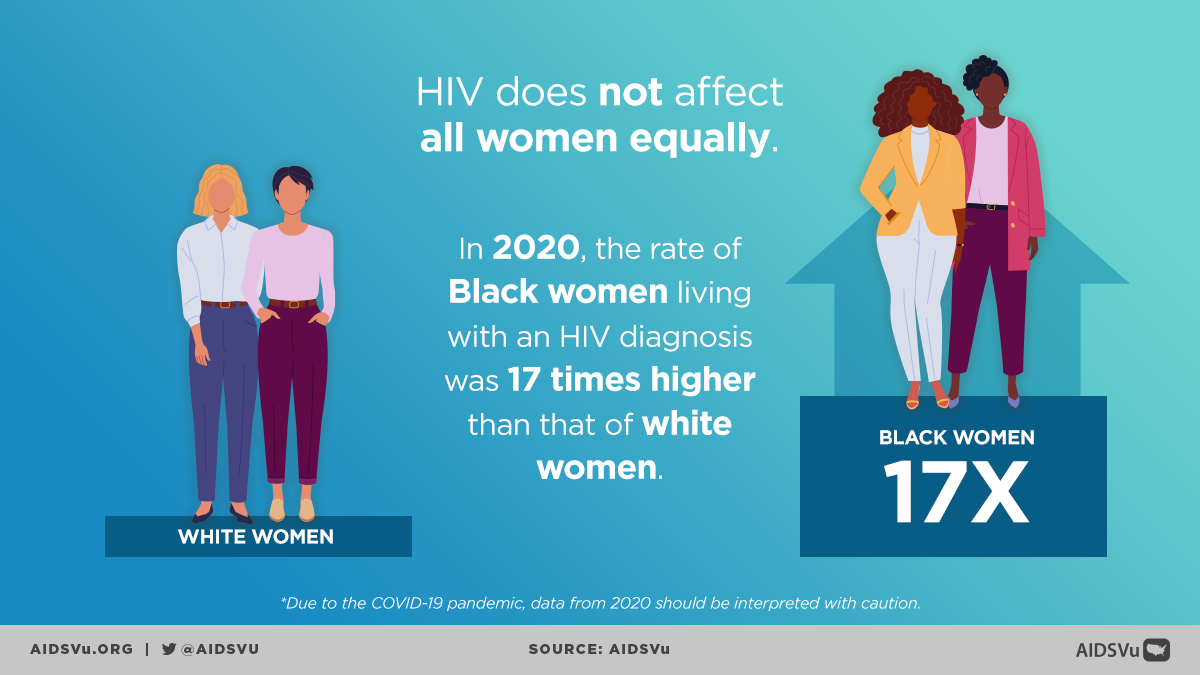
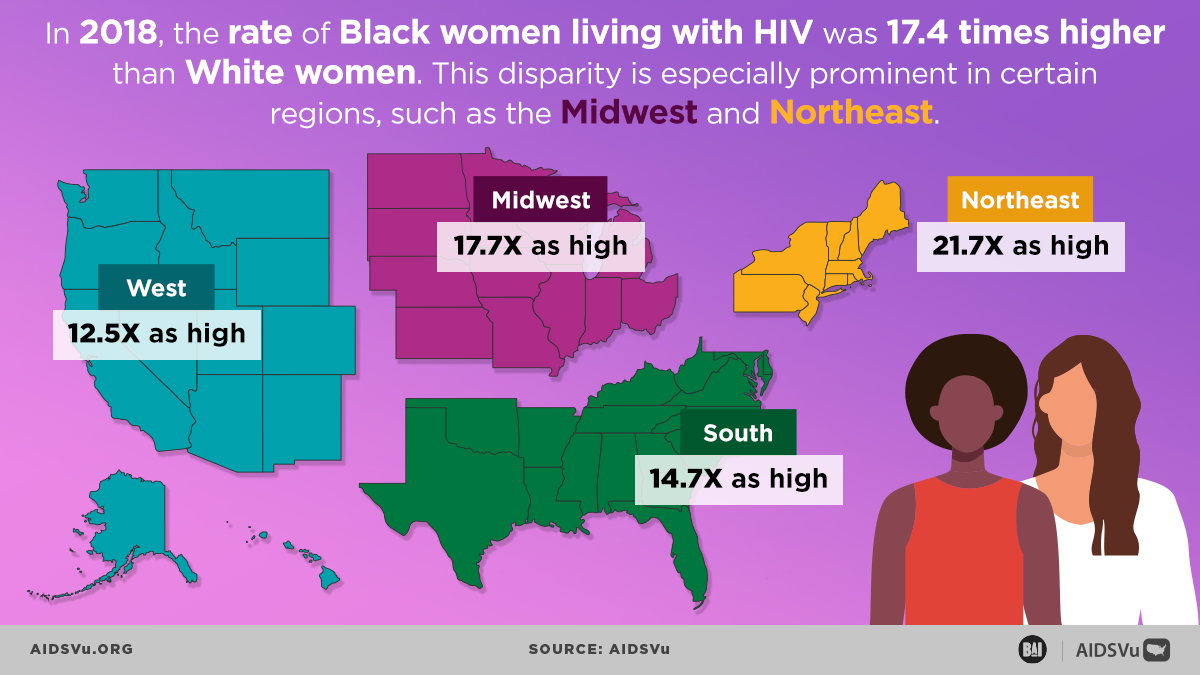
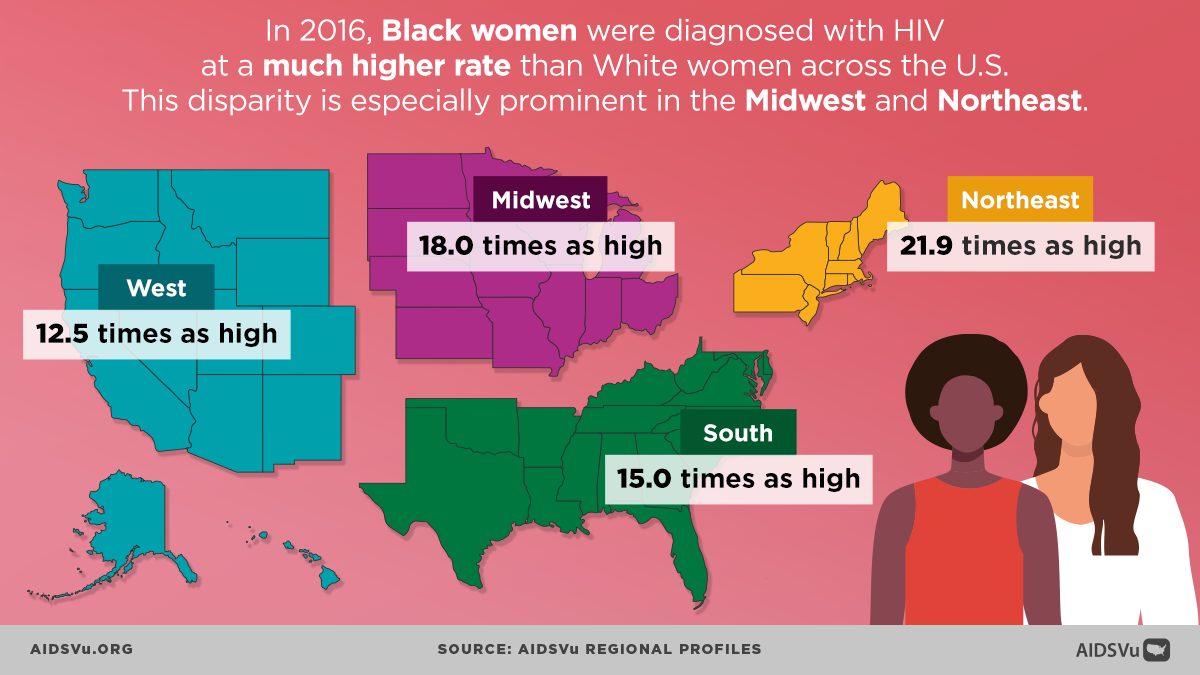
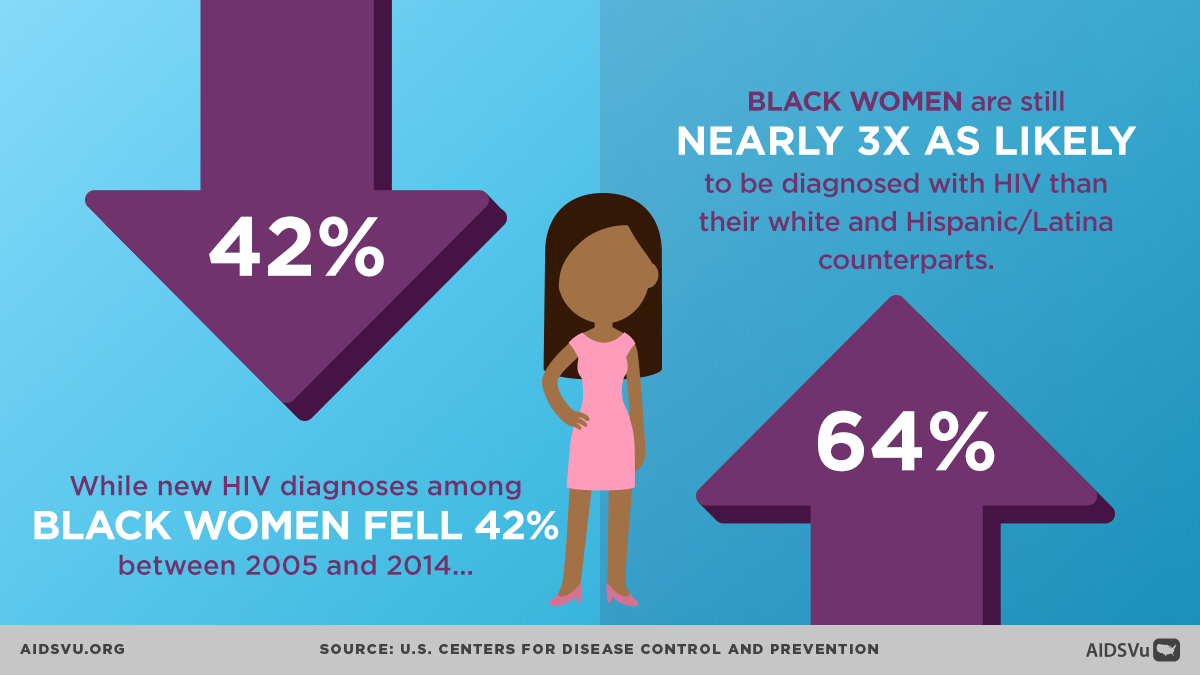
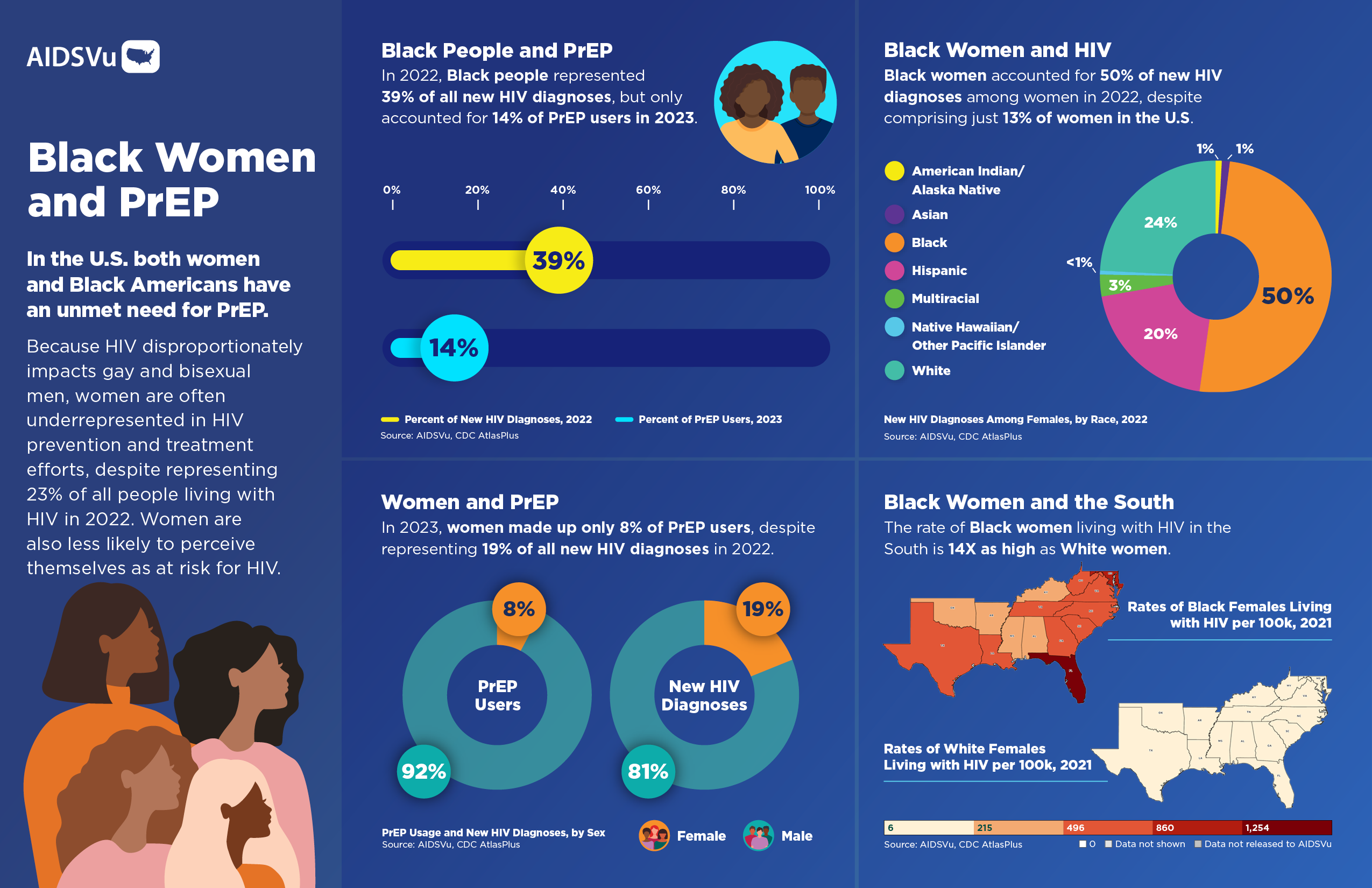
Black women face a particularly severe burden of HIV infection that reflects the intersection of racial, gender, and economic inequities. Despite representing less than 13% of the female population in the United States, Black women accounted for 50% (3,523) of new HIV infections among all women in 2022. This disparity is even more pronounced when examining infection rates: Black women are diagnosed with HIV at a rate of 19.2 per 100,000—10 times higher than white women (1.9) and 3 times higher than Latinas (5.5).
Among Black women living with HIV, most infections (approximately 85%) are attributed to heterosexual contact, often linked to having male partners who are at increased risk due to factors such as incarceration history, substance use, or undiagnosed HIV status. The convergence of gender-based power dynamics, economic vulnerability, and limited access to prevention resources creates a perfect storm of HIV risk.
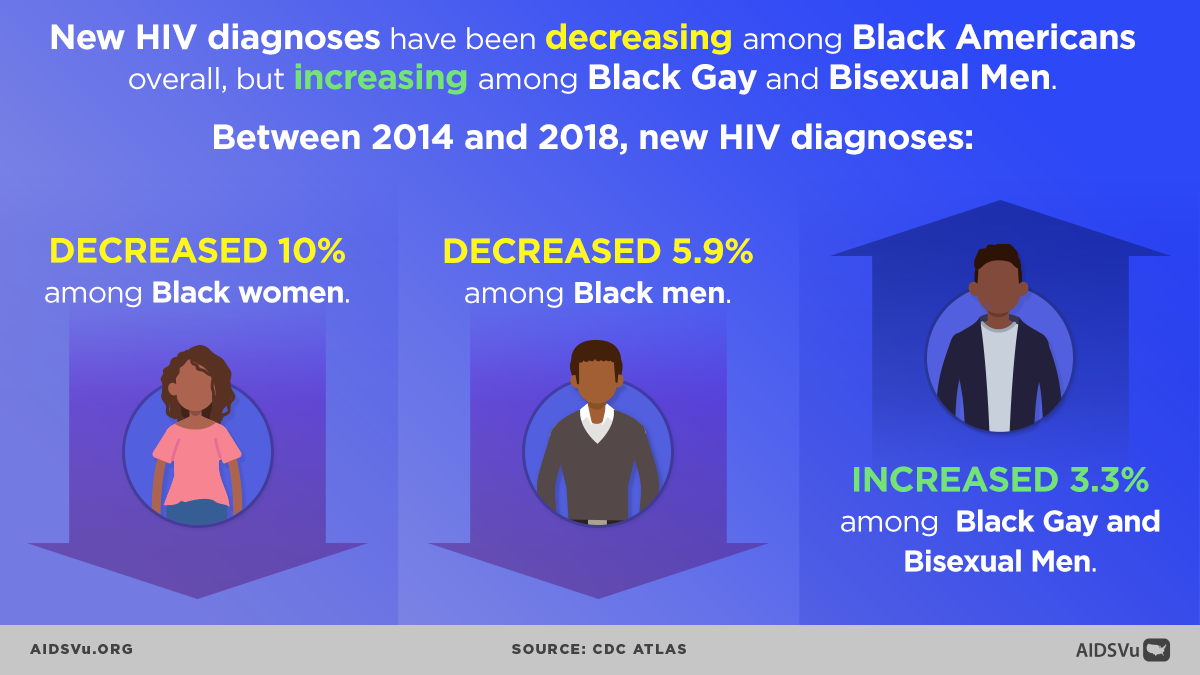
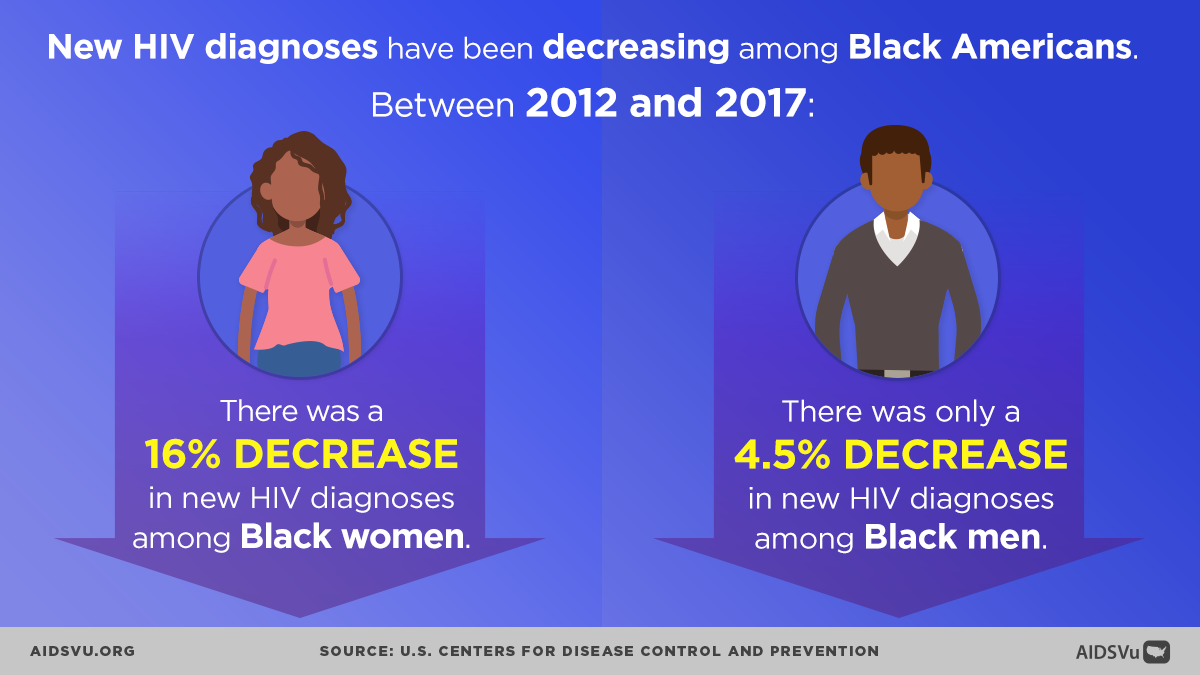
While there has been progress—with a 39% decrease in new HIV diagnoses among Black women between 2010 and 2022—recent trends show this improvement has stalled, with diagnoses essentially flat from 2018 to 2022 (decreasing by just 1%).
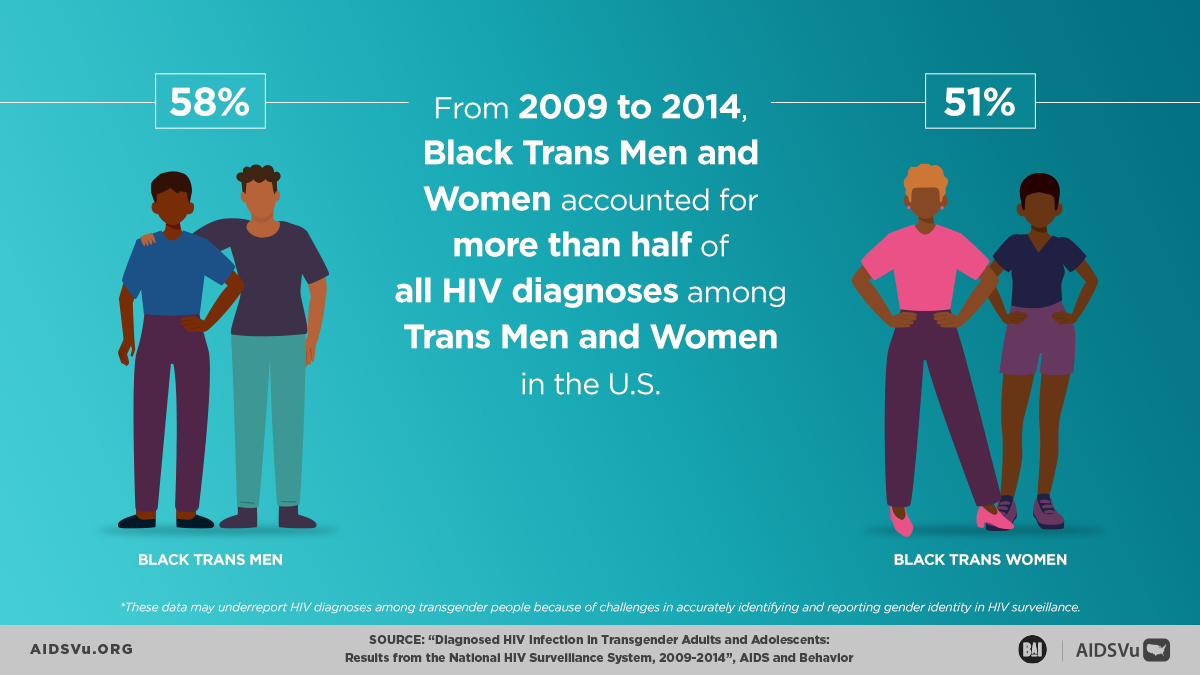
The disparities extend beyond cisgender women to transgender women as well. A recent CDC study examining HIV among transgender women in seven major U.S. cities found that Black transgender women accounted for 62% of HIV infections among transgender women with HIV. This population faces compound stigma related to both race and gender identity, creating additional barriers to healthcare access and HIV prevention services.
Perhaps most concerning is the significant gap in PrEP (pre-exposure prophylaxis) uptake among women. The disparity is particularly acute for Black women, who face additional barriers including provider bias, limited awareness about PrEP, and concerns about side effects or stigma associated with HIV prevention medication. This gap in prevention access occurs despite Black women comprising 24% of new HIV diagnoses among all Black people—a higher share than Latinas and White women (who represented 12% and 18% of new diagnoses among their respective racial/ethnic groups).
A Love Letter to Black Women
Beyond the Map
AIDSVu offers tools and resources beyond the HIV map that provide users with a deeper understanding of the HIV epidemic, its socioeconomic-driving factors, and services available at the community level.
Social Determinants of Health
See how HIV prevalence is related to poverty, high school education, median household income, etc.
Learn MoreFind Services
Use the testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services locators to find critical HIV/AIDS services near you.
Learn MoreLocal Data
View city and state profiles with local HIV/AIDS statistics, national comparison charts, and local resources.
Learn MorePrEP Access and Equity: Closing the Prevention Gap
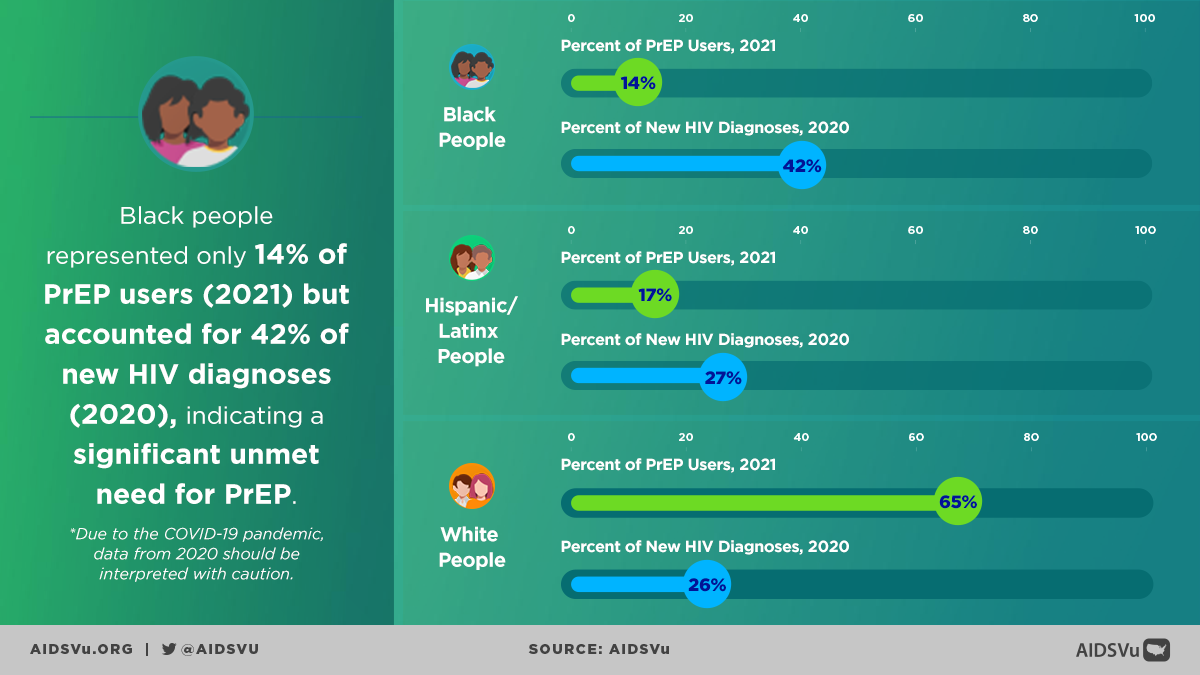
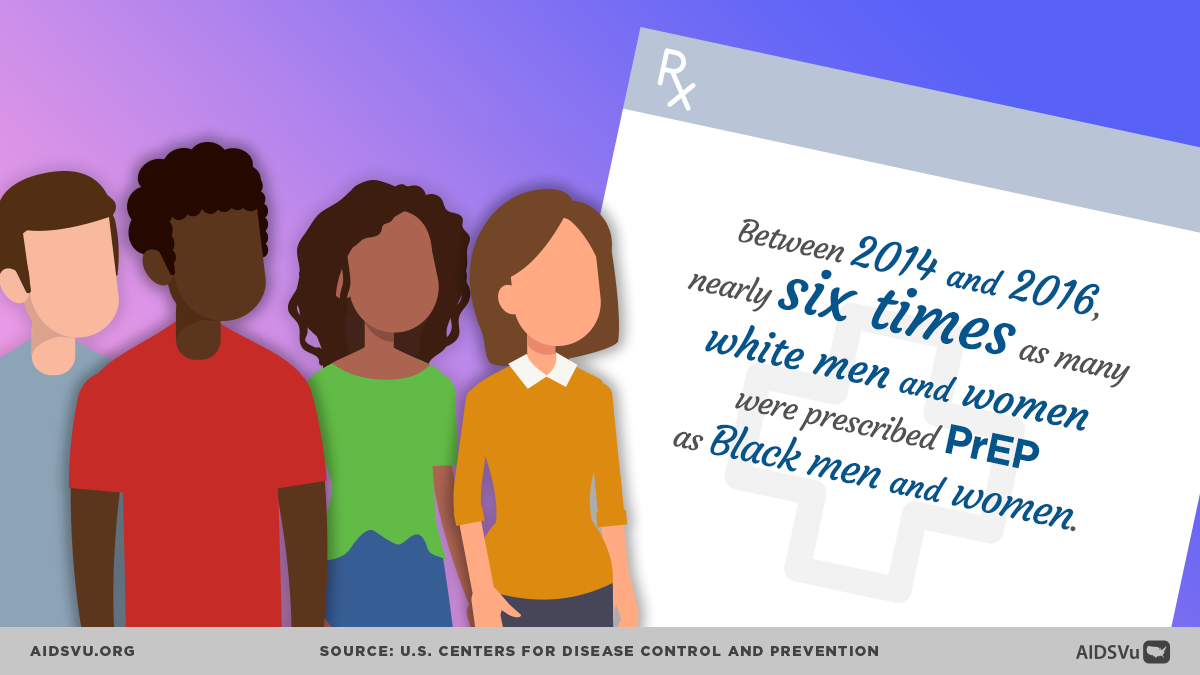
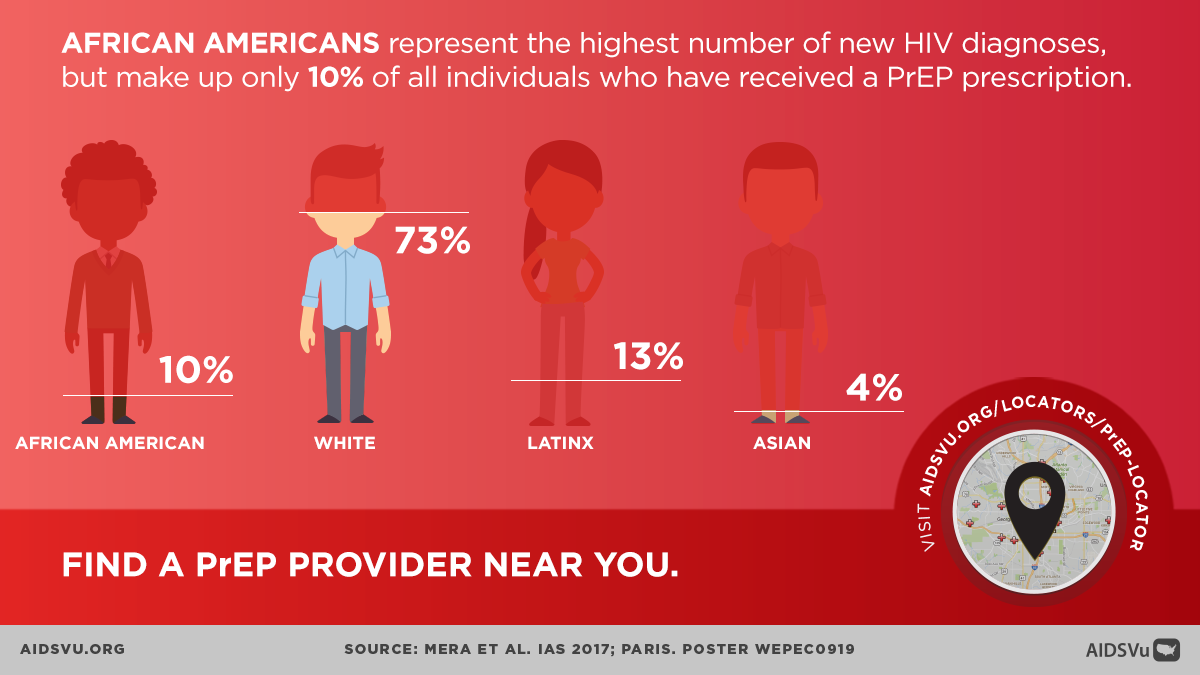
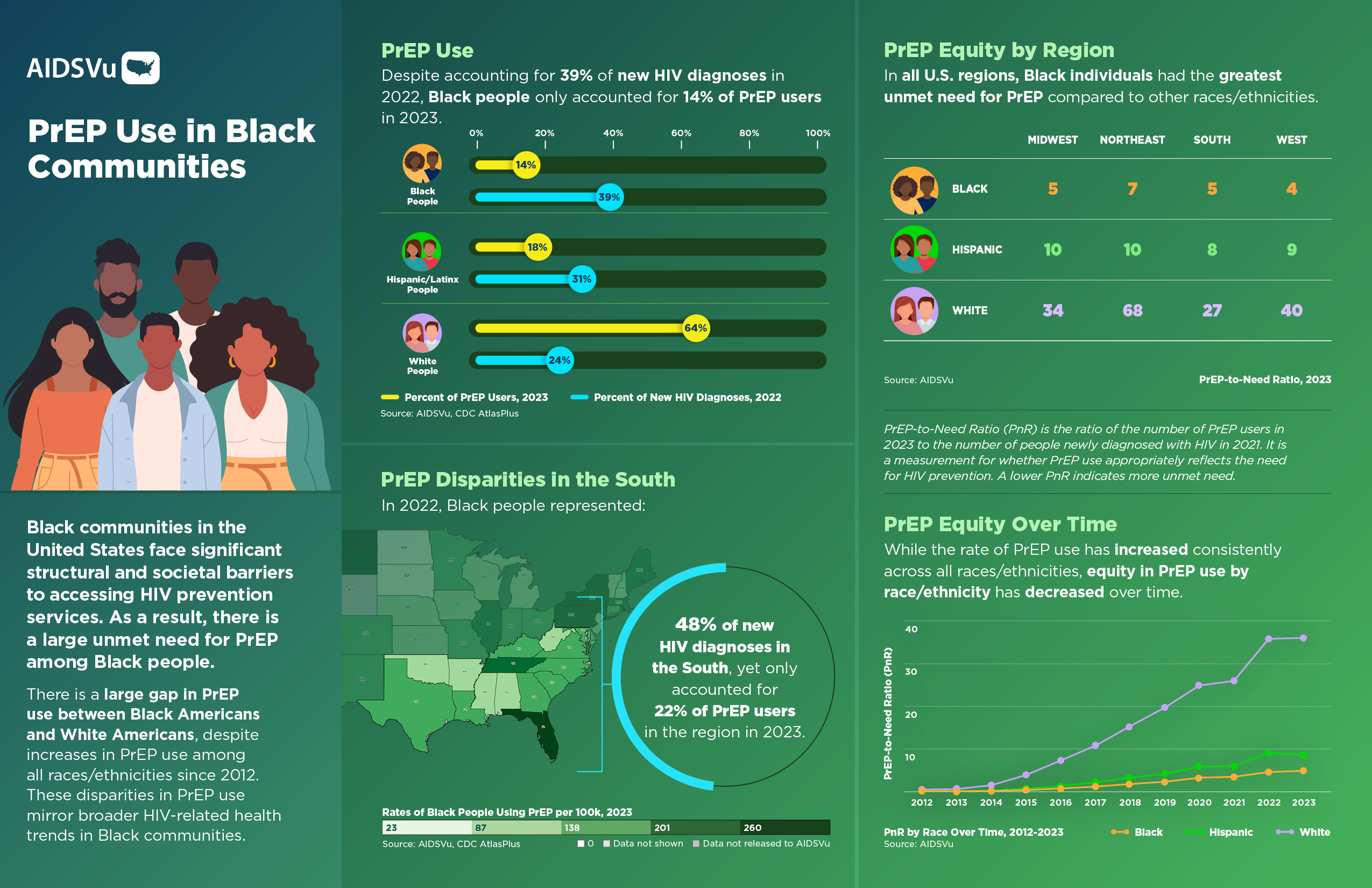
Pre-exposure prophylaxis (PrEP) represents one of the most significant advances in HIV prevention, reducing the risk of HIV transmission by more than 99% when taken consistently. However, the benefits of this breakthrough have not been equitably distributed. Black people make up a much smaller proportion of PrEP users compared to their representation among new HIV diagnoses, demonstrating significant prevention inequity.
The PrEP-to-Need Ratio (PnR) provides a useful metric for understanding these disparities. This ratio compares the number of PrEP users to the number of people newly diagnosed with HIV within a population. While PrEP use has increased consistently since 2012 across all demographic groups, significant equity gaps persist, indicating dramatically higher unmet need for PrEP in Black communities.
Multiple factors contribute to low PrEP uptake in Black communities:
Provider-level barriers: Many healthcare providers, particularly in primary care settings, lack knowledge about PrEP or comfort discussing HIV prevention. This is particularly problematic in communities where specialized HIV care is limited.
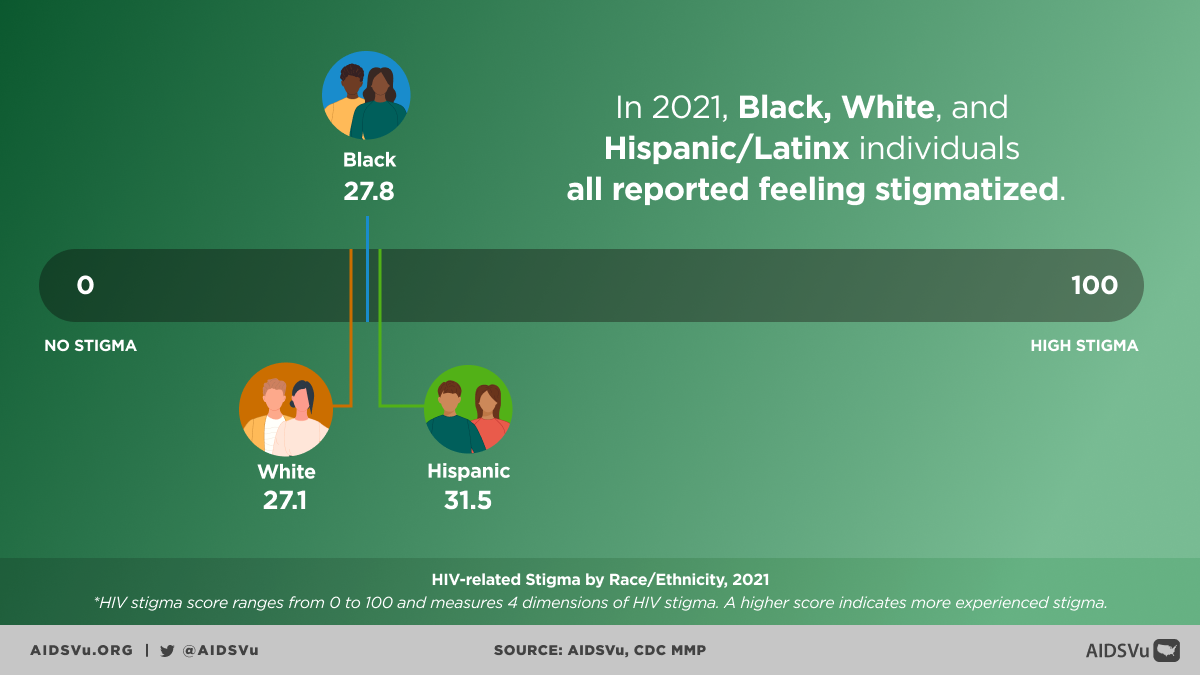
Individual-level barriers: Concerns about side effects, stigma associated with HIV prevention medication, and mistrust of medical institutions rooted in historical and ongoing experiences of discrimination all contribute to lower uptake.
Structural barriers: High costs (even with insurance), prior authorization requirements, and the need for regular lab monitoring create practical obstacles to PrEP access. Geographic barriers are also significant, as many rural and under-resourced areas lack providers who prescribe PrEP.
Cultural factors: In some communities, discussing HIV risk and prevention may be challenging due to stigma around sexuality, particularly for women and LGBTQ+ individuals.
Addressing these disparities requires comprehensive approaches that go beyond simply increasing PrEP availability. Successful interventions have included community-based PrEP programs, peer navigation services, and initiatives that address structural barriers such as transportation and childcare.
A Pattern of Health Inequity
The disparities in HIV outcomes among Black Americans are part of a broader pattern of health inequities that affect this community across multiple dimensions. From higher rates of cardiovascular disease and diabetes to lower life expectancy, Black Americans consistently experience worse health outcomes than their white counterparts. HIV disparities both contribute to and are exacerbated by these broader health inequities.
The COVID-19 pandemic highlighted many of these same structural inequities, with Black Americans experiencing higher rates of infection, hospitalization, and death. The parallels between HIV and COVID-19 disparities underscore the persistent nature of structural racism in healthcare and the urgent need for systematic change.
However, it’s crucial to recognize that addressing these disparities is not just about closing gaps—it’s about recognizing and building upon the tremendous strengths that exist within Black communities. Community organizations, faith-based institutions, advocacy groups, and informal networks have long served as sources of resilience and support. Many of the most innovative and effective HIV prevention and care programs have emerged from Black communities themselves.
5 Ways to Use AIDSVu
Explore Maps
Explore the interactive map, customize your view, and easily print for presentations, grant applications, or other materials.
Learn MoreView Local Statistics
View local statistics for your city or state, and download high-impact data visualizations for your work
Learn MoreDownload Data
Download the datasets that inform AIDSVu’s visualizations for your own research and analysis
Learn MoreLocate Services
Use AIDSVu’s service locators to find HIV testing, Pre-Exposure Prophylaxis (PrEP), and other HIV services near you
Learn MoreFor More Information
Learn more about the impact of HIV in Black communities with the following additional resources.