Patrick Sullivan, DVM, PhD, is a Professor in the Department of Epidemiology at Rollins School of Public Health of Emory University and the Principal Scientist for AIDSVu.
Q: The Centers for Disease Control and Prevention (CDC) recently launched Take Me Home, a new program within the Ending the HIV Epidemic in the U.S. initiative, to distribute free, anonymous at-home HIV self-test kits to adults aged 17 and older in the U.S. What was the impetus for starting this program and how did you get involved?
Our PRISM (Programs, Research & Innovation in Sexual Minority Health) team at Emory University has been working with the CDC for several years to show how mailing out HIV self-test kits can really improve people’s ability to follow the CDC guidelines for HIV testing. The Take Me Home site expands that research to a national scale that allows U.S. adults aged 17 and older to order their own testing kits.
Although the CDC recommends at least one annual test for people who are at high risk for HIV infection, we know that many people don’t meet that benchmark. This can be for several reasons: people might not think they’re at risk for HIV, they might not want to go to a testing location because of the stigma they may experience when requesting an HIV test, or it might just be hard to find a time for testing in their schedules. Therefore, it makes a lot of sense to give people the option of ordering an HIV test so they can test in the privacy of their own home.
Q: Take Me Home provides HIV self-testing kits for individuals to test themselves and a friend or partner. What is the importance of self-testing and how does it contribute to efforts to end the HIV epidemic?
Self-testing is just one of many ways to test for HIV that allow people to take care of their health in a way that works best for them. Sometimes it’s important to get tested at a doctor’s office or at a community-based organization where you can ask questions about reducing risks or start another risk-reduction service like pre-exposure prophylaxis (PrEP). People also may want to do their annual HIV testing in conjunction with other routine health care.
Other times, it might make more sense for people to test themselves at home. It provides a more private environment and can be more convenient if people don’t have questions and only need an HIV test. Our goal is for people who are at elevated risk for HIV to test for HIV at least once every year, so we need to ensure there are multiple testing options available to meet that goal. That may mean a combination of self-testing and other opportunities to test in different venues.
Q: How has the COVID-19 pandemic impacted HIV testing efforts? Is the expansion of self-testing options a response to the decline in in-person testing due to the pandemic?
The COVID-19 pandemic has affected all kinds of access to health care services. There’s good evidence that many people are deferring routine health maintenance and putting off regular preventive health visits and measures. This has reduced the number of routine HIV screening tests. The availability of self-testing can help people who have been weighing the health benefits of getting their routine annual HIV test against the risks of exposure to COVID-19 if they test in person.
As more and more people get vaccinated against COVID-19, I think people will gradually return to their usual health care routines. At the same time, I hope that people who used HIV self-tests during the pandemic consider how they can integrate self-tests into their own personal health plan. For example, depending on individual risks, the CDC recommends that Gay and Bisexual Men get tested for HIV at least once a year. But Gay and Bisexual Men who have frequent partner changes may benefit from testing more often than that. If an individual was already getting tested for HIV annually and experienced HIV self-testing for the first time during the pandemic, they might think about increasing their testing frequency at the six-month mark by supplementing the annual in-person test with the at-home test.
Q: The COVID-19 pandemic has raised awareness of infectious diseases overall – how has the narrative and perceptions surrounding COVID-19 testing impacted screening for other infectious diseases, including HIV?
Within my lifetime, I don’t think awareness around infectious disease testing has ever been as high as it is now. Early in the COVID-19 pandemic, access to COVID testing was really limited and many people who had symptoms wanted to get a test. I think those experiences reset our understanding of the health opportunities we have during normal times, when access to testing (including HIV testing) is quite unfettered. Since the CDC recommends that people at risk for HIV be tested annually, I think this is an important time to think about how we can utilize all the opportunities we have for HIV testing. That could mean integrating HIV screening with other blood tests at the doctor’s office, testing at a community-based organization, an at-home HIV test, or a combination of those options.
Q: AIDSVu recently added a self-testing option to our service locator. How does that addition help individuals find the testing services that are right for them?
We’re very excited that AIDSVu recently added a self-testing option to the HIV service locator. For many years, AIDSVu users could input their ZIP code and find a list of HIV testing locations in their area. The development of the Take Me Home site, along with CDC support to mail out HIV self-test kits, showed the importance of having an option to test at home.
In addition, the self-testing option increases access to medically underserved populations, such as individuals living in rural areas without an HIV testing location nearby. Some people seeking an HIV test between their annual tests or who want to test for HIV more frequently can now do that test at home. We want everybody to be able to find HIV testing in a comfortable, convenient space that fits their own schedules and needs for prevention services. If one of those tests is best taken through the self-testing option, we are happy to be able to refer people to that resource.
Q: June 27 is HIV Testing Day, an opportunity to highlight the importance of HIV testing, prevention, and treatment. What message do you have for the wider HIV community, especially individuals who may be hesitant to seek HIV testing services?
It’s important to say that so much of our efforts to end the HIV epidemic start with testing. Testing is the launch point in the next steps to protect our health. Once a person knows their status, whether it’s positive or negative, there’s a set of next steps they can take to maintain good health and have confidence in their sexual relationships to protect their health and the health of their partners.
My message for the wider HIV community and folks who may be hesitant to seek HIV services is to remind them that we have so many tools to help people. If you test and find out that you are HIV negative, we can have a conversation about how to maintain your negative status, if PrEP is right for you, and whether there are other kinds of testing you might need to take care of your sexual health. For people who test and learn that they are living with HIV, there are referrals to medications that are very effective and help people live a full lifespan. Once those medications work to reach viral suppression, there is effectively no risk for someone living with HIV to sexually transmit the virus to a partner. But the entry point for all these solutions and options is an HIV test.
The CDC recommends that all adult Americans aged 13-64 be tested for HIV every year, and for people at higher risk for HIV, testing is recommended more frequently. You can ask your health care provider what the right testing frequency is for you. I encourage people to think about all the different ways they can access HIV testing. Knowledge is power and knowing our personal HIV status really allows us to take advantage of the opportunities to protect our health and the health of those we care about.
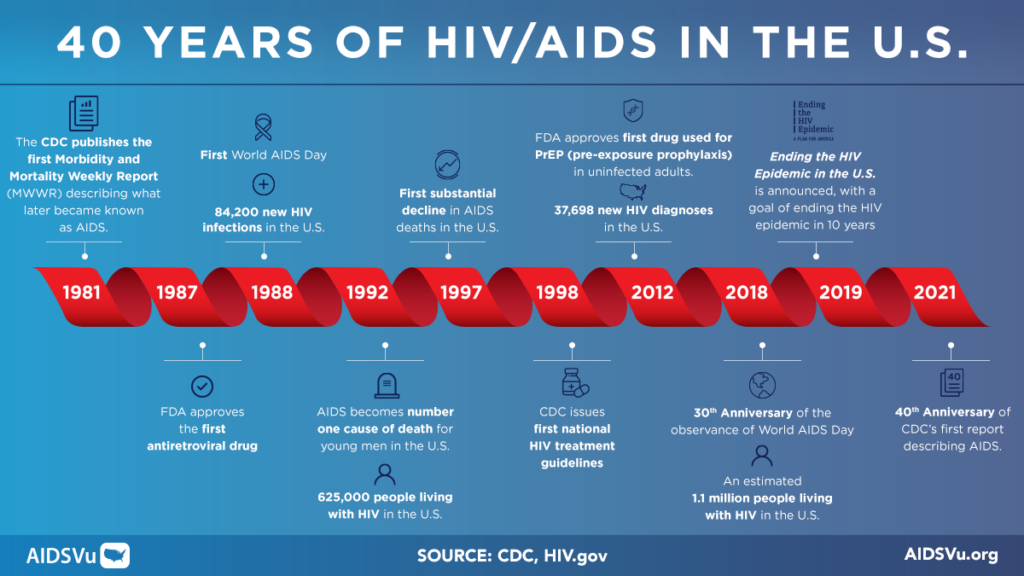
Q: This month is the 40th anniversary of the CDC’s Morbidity and Mortality Weekly Report (MMWR) first describing what became known as AIDS. After four decades, where does the HIV epidemic stand and what does the future look like?
The HIV epidemic has changed so much in the last 40 years. Initially, there really weren’t any treatments. There was a lot unknown about how HIV was transmitted, creating fear and stigma towards people living with HIV. After forty years, I think some things have changed, but we must do more. What’s most exciting for me is that we now have a full array of medications and treatments that can help those living with HIV live a full lifespan.
Yet, there is still stigma around conversations about HIV status and the behaviors that can put people at risk for the virus. We need to think and talk about HIV as a chronic disease that can be managed with medications, much like other chronic diseases that people acquire during their lifetime. For example, we don’t stigmatize people living with high blood pressure, or those who take medication to keep their blood pressure low. Similarly, it’s important to de-stigmatize folks living with HIV taking treatments to sustain their health and folks who are at risk for HIV taking medications to reduce their risks.
In the past year, we’ve learned a lot more about vaccine technologies and immune responses—and that’s continuing to build the pathway for a future HIV vaccine. COVID-19 has been remarkable because of the rapid development and deployment of a vaccine to a completely new infectious agent within a year. It can be frustrating knowing that we’re at the 40th anniversary of the AIDS epidemic and we still don’t have a vaccine, but I think it’s important that we continue to support a systematic scientific process and recognize the progress in HIV treatment, HIV prevention, and the path to an HIV vaccine. I am hopeful for the future because there is a real commitment to research to cure HIV and find a vaccine. Until that time, testing will be a critical piece of the puzzle to minimize the health impacts of HIV and protect ourselves and our partners.